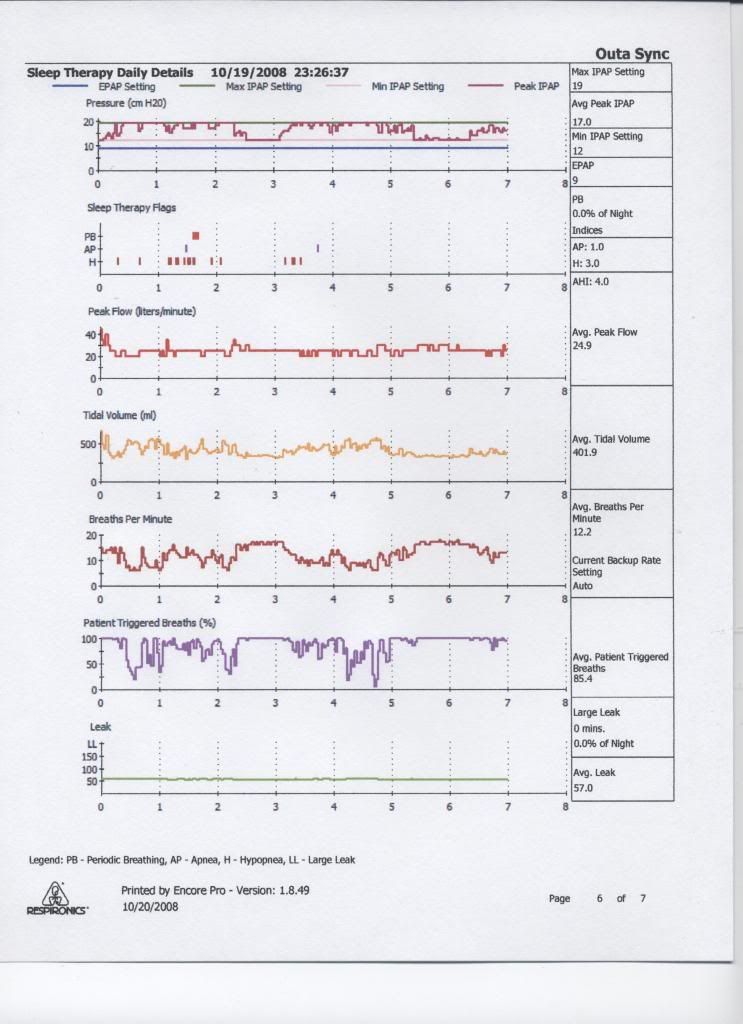
StillAnotherGuest wrote:But with that thing pegged at IPAP
max for about 5.5 hours out of a total about 9.5 hours (I don't think it's
completely pegged, short-cycle events should have at least
some IPAP
min time. I mean, the thing can't establish a baseline at IPAP
max, so it certainly seems real busy attacking something or other). However, this can't be determined due to the coarseness of the reporting mechanism. And why it is essential to qualify the underlying disease process.
Since Younes demonstrated that you can create "central dysregulation" in almost anybody
Susceptibility to periodic breathing with assisted ventilation during sleep in normal subjects
it is now impossible to determine whether this entire approach is correcting or creating "central dysregulation".
SAG, I agree with this assessment. We can see what is either outstanding or induced central dysregulation in Bev's Encore charts. Encore's scoring of PB is the strongest clue. The other revealing Encore data trace is the IPAP peak line. It shows the algorithm being very busy, sending IPAP peak all the way up to IPAP max for grotesquely extended periods. When SV successfully stabilizes periodic breathing, on an as-needed basis, there is absolutely no algorithmic basis to hold that IPAP max value for extended periods as we see on Bev's charts.
I'm also inclined to think that this machine's adaptive pressure response may be creating more problems for Bev than it is solving. Younes, et al cite that tendency in PAV, short of any temporal analysis the BiPAP autoSV algorithm may employ that experimental PAV circa 1998 did not employ. Despite the fact that the earlier implementation of PAV studied by Younes et al was not initially designed to address PB for lack of temporal variable analysis---and the fact that the Respironics implementation of autoSV claims to succesfully treat PB----there is absolutely no doubt in my mind whatsoever that the Respironics (and even Resmed) implementations of auto/adaptive SV can and will induce central dysregulation in
some patients for lack of necessary algorithmic and especially temporal-variable based controls. Unfortunately today's "automated" SDB technology is far from perfect---far from being any kind of SDB treatment panacea. Here, SV technology is extremely shortsighted in that it sorely lacks temporal variable analysis IMO.
Regarding Bev's tendency toward periodic breathing. My strong personal hunch is that Bev, like so many other patients, probably has a tendency toward (stimuli) "responsive" central dysregulation. I think those are likely the patients who, ironically, have an inordinately difficult time with SV adaptation during the wake/stage-1 transition----based on highly dynamic adaptive/maladaptive receptor sensitivities that might be theoretically inherent to certain autonomic defensive characteristics (but one possible genetic phenotype entailing viable evolutionary survival value). Any patient entailing highly characteristic/deterministic respiratory controller loop/gain dyscontrol should be much better suited for auto/adaptive SV in my own way of analyzing. Conversely, any patient with neurologically defensive adaptive/maladaptive receptor sensitivities are probably going to be extremely difficult for any temporally short-sighted auto/adaptive SV algorithm to resolve. Those chemoreceptor sensitivities are theoretically going to be a moving target. These latter patients may be the ones having an inordinately difficult time making that wake/stage-1 transition. Then off to high-strung and defensive autonomic breathing they eventually go, where they still may have a difficult time defensively and adaptively attempting to survive that highly dynamic stimuli presented by SV pressure therapy.
If this neurologically defensive genetic phenotype even exists, my hunch is that central dysregulation can be methodologically induced by presenting nothing more than external sensory stimuli---much more so than in any control set.
SAG wrote:As previously noted, this machine will "automatically" address "central dysregulation", but obstructive events need to be manually addressed. And if events cannot be accurately identified, how do know (1) when you've fixed them; or (2) if they're even there?
Another extremely valid point IMO. As always, thanks for your professionally seasoned and very wise input, SAG.
-----------------------------------------------------------------------------------
Bev, I'm still of the highly-speculative impression that you're a "tightly strung" or "neurologically defensive" sleeper. I think any set of disruptive stimuli is inclined to devastate your sleep architecture. That means GERD, pain, aerophagia, unfamiliar environmental input (new surroundings, new sound, etc.), and now the pressure pulsing of auto SV can account for deteriorated sleep and even defensively-dysregulated breathing at times.
If auto SV's highly dynamic pressure response is even capable of offsetting bifurcated central dysregulation in your hypothetical case, it's only going to be because you have come to consciously and subconsciously associate that same pressure stimuli as being familiar and friendly rather than being potentially threatening. And in my own view it's highly questionable whether any human can carry that adaptive association into sleep and autonomic breathing. I strongly suspect that may be an impossibility.
I also recommend finding a different sleep doctor in the upcoming insurance cycle---one who is open to the idea that your daytime cognitive issues and EDS are problems that need to be solved. Short of that I would suggest trying fixed BiLevel. There is a chance that fixed BiLevel may be a suitable modality for you. And if it turns out that you eventually become
extremely comfortable with fixed BiLevel, then the auto SV algorithm may be less-inclined to incessantly push at IPAP max as it currently does.