UARS: A Critical Link to Optimizing PAP Therapy Results
-
BarryKrakowMD
- Posts: 65
- Joined: Wed Dec 05, 2007 12:48 am
- Contact:
Quantitative Data
Let’s pick up again on the theme of quantitative data. I think it is a very important one, and virtually all the comments and threads made following my posts reflect a great deal of sophisticated thinking. But therein may lay the problem, because most of you probably know that the word sophisticated has links to sophistry.
The question I’m raising concerns not whether quantitative data provides useful information, but whether we should trust the “completeness” of the data or as a corollary whether the data will direct us properly or lead us astray.
My own experience with 420E data led me astray for nearly 2 years, but I confess that it might have been my poor interpretative skills that caused the problem.
I continued to see low AHIs with high run numbers, consistently in the 10 to 20 range, but because I felt so much better compared to straight CPAP, I continued to wed myself to my “new” normal and imagined that this degree of improvement was as good as it got. My nocturia was gone, and I figured that I could live with a little dry mouth in the morning and some residual fatigue and sleepiness.
By coincidence, or is it serendipity, I began to notice that another sleep tech, Bryan Ellis, at another sleep lab, http://www.highplainssleep.com, (for which I read sleep studies) was using bilevel on all his UARS patients in 2004. When I asked him why, he said the patients found it more comfortable, and he noticed they adapted more easily during the titrations.
I thought this idea was silly, because a few years earlier I tried bilevel one night and thought it the worst possible device (to be discussed in an upcoming new topic on bilevel). Pragmatically, though, I wasn’t going to argue with success, so we knew we owed it to ourselves and our patients to try out bilevel in the sleep lab on some SDB patients.
What we immediately saw (and what made me start kicking myself in the posterior shortly thereafter) was that the airflow signal looked fundamentally different than any other signal I had seen before, or at least seen consistently. Both the inspiratory and expiratory curves looked fully rounded (or elliptical in some cases) (please see graphic at http://www.sleepdynamictherapy.com), and the patients reported excellent results on the very first titration (or on a retitration).
Aside: The graphics posted previously are schematics and can be helpful, but they may also be misleading by not showing more precise relationships between the transition from inspiration to expiration or expiration to inspiration.
Greedily (I guess that makes me a corporation), I wanted to try bilevel right away as did my lead sleep tech at the time, Dominic Melendrez. Using a zero tolerance attitude about flow limitation, Dom titrated me to 18/14 (which we both thought insane since I’d been using APAP of 8 to 12 and rarely 10 to 14), and I titrated Dominic to 20 over whatever. It was around 4 am, and the assigned sleep tech kept saying, “are you sure that’s flow limitation?” My response, “I’m not sure, but it’s not rounded, so keep increasing until it rounds,” which it did at IPAP of 20.
From that point forward I started using bilevel at pressures around 14/10 and fairly rapidly worked my way up to 18/10…”and loving it!” to quote the immortal secret agent Maxwell Smart. Now, I'm at 21/12.5.
So, I realized that the runs were telling some truth; they were telling me that I still had flow limitation, so yes, it was valuable, but they weren’t telling me how I could solve the problem, and most importantly as we next discovered, the APAP device was also not offering me an opportunity to solve the problem. And, that’s what I mean by “incomplete” data.
Which brings me to the biggest slam I have about the quantitative approach; it’s steeped in reductionism while at the same time begging the question about its own validity. It may be science but it isn’t rocket science. So, by constantly or excessively relying on it, you may get the answers you want but not the ones you need.
Here’s an analogy to consider. Someone asks you to remodel a room and hands you a tape measure to use that only has the markings of “feet” on it, but no “inches” let alone “eighths of inches.” Surely, you would know you’re in for a long and tedious effort.
I believe that the current quantitative data in most of the machines I’ve dealt with represent incomplete data, just as I’m persuaded that probably all APAP machines have incomplete algorithms.
To reiterate, those of you with a keener data sense than I are clearly gaining information and benefits from that data, but I suspect that some proportion of those who rely too much on data are missing out on something more important by NOT spending more time “quantifying” the changes or lack thereof in their personal symptom load.
If the goal is normal breathing, then the question should be at minimum, “will normal breathing yield normal sleep?”
In my own experiences, I think I know what normal sleep is because I have experienced something very close to it many times in the last 10 years. And, I also know that with careful observation, I can usually discern within one hour of awakening each morning whether I had an 85%, 90%, or 95% night.
Would I love to get 100% (normal) every night? Yes, but I don’t think the technology is there to accomplish such a feat due to the relatively primitive nature of masks and PAP therapy machines. Still, I’m fairly convinced that I’m averaging nights between 88% to around 96% of my potential response much more consistently on bilevel than anything else I’ve tried.
Let me perseverate one more time by way of analogy again to close this post. Imagine you have never tasted chocolate candy and there is no way for you to taste it. Instead, scientists offer you various recipes to make chocolate candy, but you are on your own in cooking up a batch and assessing the quality of the product. In my experience, this is the critical barrier that tops all other barriers in the management of a sleep problem. Without a first hand experience with normal sleep, then all the puttering you do with the various recipes of APAP, CLFEX and so on, only permit you to guesstimate what “normal” sleep is like. For many people that guessing game is never sufficient to lead to a true optimization with PAP therapy, because most individuals stop as soon as they get better instead of searching for the “more better” I believe is available to most SDB patients.
Last, there are those among you who are much more capable, abstract thinkers than I am. Such people have a greater capacity to imagine what normal sleep is like and to therefore grade whatever current experience they have and contrast it with what they believe to be the ultimate goal—normal sleep.
My question for these gifted individuals is that even with your advanced ability to see, sense or know what’s missing, do you have the ability to fix this problem with your current focus on quantitative data from the downloads of your machines? Some of you apparently do, I imagine, based on the many commentaries I’ve read in the past week, but I suspect some of you do not.
Sad to say, it’s also apparent that many of you do not believe you can rush back to a sleep lab and get a great bilevel titration. So, we’ll resume the discussion in a new topic on bilevel to help you decide if it’s worth a try.
By the way, the push for bilevel is anything but an “establishment-driven” perspective. The consensus on practice parameters (see below) from the American Academy of Sleep Medicine does not indicate any preference for bilevel over CPAP in terms of promoting adherence to PAP therapy; it only states that bilevel may provide expiratory relief in patients using high CPAP pressures or who suffer lung diseases that make it difficult to use CPAP. That’s the party line. Our clinical experience differs from the establishment view, which is our rationale for recommending more bilevel devices to our patients.
Citation available at
http://www.journalsleep.org
SLEEP 2006 Mar 1;29(3):375-80.
Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders.
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J Jr, Friedman L, Kapen S, Kapur VK, Kramer M, Lee-Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS; American Academy of Sleep Medicine.
The question I’m raising concerns not whether quantitative data provides useful information, but whether we should trust the “completeness” of the data or as a corollary whether the data will direct us properly or lead us astray.
My own experience with 420E data led me astray for nearly 2 years, but I confess that it might have been my poor interpretative skills that caused the problem.
I continued to see low AHIs with high run numbers, consistently in the 10 to 20 range, but because I felt so much better compared to straight CPAP, I continued to wed myself to my “new” normal and imagined that this degree of improvement was as good as it got. My nocturia was gone, and I figured that I could live with a little dry mouth in the morning and some residual fatigue and sleepiness.
By coincidence, or is it serendipity, I began to notice that another sleep tech, Bryan Ellis, at another sleep lab, http://www.highplainssleep.com, (for which I read sleep studies) was using bilevel on all his UARS patients in 2004. When I asked him why, he said the patients found it more comfortable, and he noticed they adapted more easily during the titrations.
I thought this idea was silly, because a few years earlier I tried bilevel one night and thought it the worst possible device (to be discussed in an upcoming new topic on bilevel). Pragmatically, though, I wasn’t going to argue with success, so we knew we owed it to ourselves and our patients to try out bilevel in the sleep lab on some SDB patients.
What we immediately saw (and what made me start kicking myself in the posterior shortly thereafter) was that the airflow signal looked fundamentally different than any other signal I had seen before, or at least seen consistently. Both the inspiratory and expiratory curves looked fully rounded (or elliptical in some cases) (please see graphic at http://www.sleepdynamictherapy.com), and the patients reported excellent results on the very first titration (or on a retitration).
Aside: The graphics posted previously are schematics and can be helpful, but they may also be misleading by not showing more precise relationships between the transition from inspiration to expiration or expiration to inspiration.
Greedily (I guess that makes me a corporation), I wanted to try bilevel right away as did my lead sleep tech at the time, Dominic Melendrez. Using a zero tolerance attitude about flow limitation, Dom titrated me to 18/14 (which we both thought insane since I’d been using APAP of 8 to 12 and rarely 10 to 14), and I titrated Dominic to 20 over whatever. It was around 4 am, and the assigned sleep tech kept saying, “are you sure that’s flow limitation?” My response, “I’m not sure, but it’s not rounded, so keep increasing until it rounds,” which it did at IPAP of 20.
From that point forward I started using bilevel at pressures around 14/10 and fairly rapidly worked my way up to 18/10…”and loving it!” to quote the immortal secret agent Maxwell Smart. Now, I'm at 21/12.5.
So, I realized that the runs were telling some truth; they were telling me that I still had flow limitation, so yes, it was valuable, but they weren’t telling me how I could solve the problem, and most importantly as we next discovered, the APAP device was also not offering me an opportunity to solve the problem. And, that’s what I mean by “incomplete” data.
Which brings me to the biggest slam I have about the quantitative approach; it’s steeped in reductionism while at the same time begging the question about its own validity. It may be science but it isn’t rocket science. So, by constantly or excessively relying on it, you may get the answers you want but not the ones you need.
Here’s an analogy to consider. Someone asks you to remodel a room and hands you a tape measure to use that only has the markings of “feet” on it, but no “inches” let alone “eighths of inches.” Surely, you would know you’re in for a long and tedious effort.
I believe that the current quantitative data in most of the machines I’ve dealt with represent incomplete data, just as I’m persuaded that probably all APAP machines have incomplete algorithms.
To reiterate, those of you with a keener data sense than I are clearly gaining information and benefits from that data, but I suspect that some proportion of those who rely too much on data are missing out on something more important by NOT spending more time “quantifying” the changes or lack thereof in their personal symptom load.
If the goal is normal breathing, then the question should be at minimum, “will normal breathing yield normal sleep?”
In my own experiences, I think I know what normal sleep is because I have experienced something very close to it many times in the last 10 years. And, I also know that with careful observation, I can usually discern within one hour of awakening each morning whether I had an 85%, 90%, or 95% night.
Would I love to get 100% (normal) every night? Yes, but I don’t think the technology is there to accomplish such a feat due to the relatively primitive nature of masks and PAP therapy machines. Still, I’m fairly convinced that I’m averaging nights between 88% to around 96% of my potential response much more consistently on bilevel than anything else I’ve tried.
Let me perseverate one more time by way of analogy again to close this post. Imagine you have never tasted chocolate candy and there is no way for you to taste it. Instead, scientists offer you various recipes to make chocolate candy, but you are on your own in cooking up a batch and assessing the quality of the product. In my experience, this is the critical barrier that tops all other barriers in the management of a sleep problem. Without a first hand experience with normal sleep, then all the puttering you do with the various recipes of APAP, CLFEX and so on, only permit you to guesstimate what “normal” sleep is like. For many people that guessing game is never sufficient to lead to a true optimization with PAP therapy, because most individuals stop as soon as they get better instead of searching for the “more better” I believe is available to most SDB patients.
Last, there are those among you who are much more capable, abstract thinkers than I am. Such people have a greater capacity to imagine what normal sleep is like and to therefore grade whatever current experience they have and contrast it with what they believe to be the ultimate goal—normal sleep.
My question for these gifted individuals is that even with your advanced ability to see, sense or know what’s missing, do you have the ability to fix this problem with your current focus on quantitative data from the downloads of your machines? Some of you apparently do, I imagine, based on the many commentaries I’ve read in the past week, but I suspect some of you do not.
Sad to say, it’s also apparent that many of you do not believe you can rush back to a sleep lab and get a great bilevel titration. So, we’ll resume the discussion in a new topic on bilevel to help you decide if it’s worth a try.
By the way, the push for bilevel is anything but an “establishment-driven” perspective. The consensus on practice parameters (see below) from the American Academy of Sleep Medicine does not indicate any preference for bilevel over CPAP in terms of promoting adherence to PAP therapy; it only states that bilevel may provide expiratory relief in patients using high CPAP pressures or who suffer lung diseases that make it difficult to use CPAP. That’s the party line. Our clinical experience differs from the establishment view, which is our rationale for recommending more bilevel devices to our patients.
Citation available at
http://www.journalsleep.org
SLEEP 2006 Mar 1;29(3):375-80.
Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders.
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J Jr, Friedman L, Kapen S, Kapur VK, Kramer M, Lee-Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS; American Academy of Sleep Medicine.
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Puritan Bennett Breeze Nasal Pillows; ResMed Mirage Quattro FFM; Respironics Premium Chinstrap; Breath Right Nasal Strips |
Barry Krakow, MD
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
jskinner wrote:khvn,khvn wrote:Whoa, look at that EPAP line in the BIFLEX chart! The machine allows pressure to dip below EPAP--which is a no-no since not enough pressure would allow apnea to pop up here.
You honestly think they would design it to do that if it wasn't safe to do so? You act like the people who design these things are idiots and don't do any testing or have any expertise.
-James
Au contraire, James... I was actually a-d-m-i-r-i-n-g the *thoughtful* and *clever* way the BIFLEX handles the EPAP dip. I'm sure you've heard people exclaim "Whoa, I couldn't believe they did that..." in a *good* way, haven't you?
-
Guest
Again, Doctor, I say thank you. When I initially started I raised my pressure from the 4 it was staying at because I felt I was suffocating. Then I kept raising it to an APAP setting of 8-12 and felt better, and stopped. There I have been for months. I have tweaked my vitamins, my diet, my exercise, anything I can think of to feel normal again. And I feel a ton better, unimaginably much better. But I don't think I feel well, I don't know that I am there yet, wherever there may be.
So, I am digging out my self assessment of symptoms check list and playing with my pressure. I will take it slow so I have time to see the changes, and really shoot for feeling great.
Thanks for all of the information, it's nice to have someone knowledgeable posting about UARS.
So, I am digging out my self assessment of symptoms check list and playing with my pressure. I will take it slow so I have time to see the changes, and really shoot for feeling great.
Thanks for all of the information, it's nice to have someone knowledgeable posting about UARS.
guy you have no idea what you are talking about other than screwing up this thread where a lot of people want to learn from it.khvn wrote:Whoa, look at that EPAP line in the BIFLEX chart! The machine allows pressure to dip below EPAP--which is a no-no since not enough pressure would allow apnea to pop up here. What saves the day must be our own breath that compensates for the pressure loss and pushes the total pressure up to the safety of the EPAP line again.
dips in x-flex are only momentary and at the beginning of expiration which have been clinically shown not to impede therapy. The therapy splint is always maintained and the pressure never reaches zero.
someday science will catch up to what I'm saying...
Re: Quantitative Data
Very interesting points. I remember that I was somewhat disappointed with my sleep/titration study data, too. I had all those "spontaneous arousals" but no explanation. Now I have one, at least theoretically.BarryKrakowMD wrote:Let’s pick up again on the theme of quantitative data. I think it is a very important one, and virtually all the comments and threads made following my posts reflect a great deal of sophisticated thinking. But therein may lay the problem, because most of you probably know that the word sophisticated has links to sophistry.
The question I’m raising concerns not whether quantitative data provides useful information, but whether we should trust the “completeness” of the data or as a corollary whether the data will direct us properly or lead us astray.
. . .I believe that the current quantitative data in most of the machines I’ve dealt with represent incomplete data, just as I’m persuaded that probably all APAP machines have incomplete algorithms.
Two nights ago, due to these discussions, I did reset my machine to auto mode in order to track the flow limitations it recorded. So, I'm wondering if you are saying that the FL's shown on my REMSTAR classic auto machine are not the whole picture. Are you saying there might be substantially more than shown?
I don't have a PB machine. Would you explain what you mean by runs?My own experience with 420E data led me astray for nearly 2 years, but I confess that it might have been my poor interpretative skills that caused the problem.
I continued to see low AHIs with high run numbers, consistently in the 10 to 20 range, but because I felt so much better compared to straight CPAP, I continued to wed myself to my “new” normal and imagined that this degree of improvement was as good as it got. My nocturia was gone, and I figured that I could live with a little dry mouth in the morning and some residual fatigue and sleepiness.
I was using my data to detect leaks and also to see what pressure seemed optimal for me. This did improve my sleep up to a point. I think paying attention to how I feel yields another dimension. I'm sure my sleep is not yet optimal. The worst of the brain fog is gone, but I still get a brain slowdown from midafternoon on. I've had a few absolutely great days where I feel amazing. But not most of the time.To reiterate, those of you with a keener data sense than I are clearly gaining information and benefits from that data, but I suspect that some proportion of those who rely too much on data are missing out on something more important by NOT spending more time “quantifying” the changes or lack thereof in their personal symptom load.
I'm looking forward to the new topic discussion of this. First, how to find a lab where I could get a great bilevel titration. Second, to get the insurance company to pay for the titration. Since my first one was botched, perhaps that could be the rationale, especially given that the tech (not even certified) told me in advance that she planned to titrate me at 4 or 5 and that would take care of it. (I still had 21 spontaneous arousals/hour at this level).Sad to say, it’s also apparent that many of you do not believe you can rush back to a sleep lab and get a great bilevel titration. So, we’ll resume the discussion in a new topic on bilevel to help you decide if it’s worth a try.
- Rose
Thread on how I overcame aerophagia
http://www.cpaptalk.com/viewtopic/t3383 ... hagia.html
Thread on my TAP III experience
http://www.cpaptalk.com/viewtopic/t3705 ... ges--.html
Thread on how I overcame aerophagia
http://www.cpaptalk.com/viewtopic/t3383 ... hagia.html
Thread on my TAP III experience
http://www.cpaptalk.com/viewtopic/t3705 ... ges--.html
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Actually, in contrast to what you might predict, the airway generally collapses either towards the end of expiration or at the end of expiration in OSA patients. This is a time when the dilator muscles around the neck are electrically quiet, leaving the airway exposed to mass loading by the surrounding tissue/fat. This is referred to as passive collapse of the airway.krousseau wrote:Inhalation is when negative pressures occur in the airway causing it to collapse inward. Exhale---pinch your nostrils closed and keep your lips sealed---now try to inhale. You can feel the inward pull at your cheeks and back of your throat. Those are the forces that lead to collapse. When you exhale that doesn't happen.
Last edited by split_city on Mon Dec 17, 2007 10:02 pm, edited 1 time in total.
Dr. K:
Do you have any sample titration tables you can direct us to showing how you found your ideal EPAP pressure then continued on to obtain the ideal rounded flow curve?
In other words, what factors do you look for to tell you to stop at 18/14 for example, obviously if I was self-titrating I would only use high enough EPAP pressure to eliminate the apnea/snoring, then continue increasing with the IPAP to further reduce any hypopnea or flow limitation seen. In other words, how does your titration for elimination of FL'S associated with UARS differ from a conventional OSA bi-level titration?
if for example the hypopnea and FL's were eliminated at say 16/14, do you continue with IPAP looking then to only round off the flow curve?
I wonder why a mfg like Respironics doesn't build that function into its auto bi-pap algorithm, it would seem to me that machine could easily identify that curve you are looking for. Have you done any comparisons with the newer Bi-pap autos to compare to the manual titrations?
Wish Wally was reading this thread, he had "FL's at 18 cm pressure and his sleep was at times a train wreck. I think he has done some experimenting with his pressures and the Bipap Auto will record those events in Bipap mode.
Do you have any sample titration tables you can direct us to showing how you found your ideal EPAP pressure then continued on to obtain the ideal rounded flow curve?
In other words, what factors do you look for to tell you to stop at 18/14 for example, obviously if I was self-titrating I would only use high enough EPAP pressure to eliminate the apnea/snoring, then continue increasing with the IPAP to further reduce any hypopnea or flow limitation seen. In other words, how does your titration for elimination of FL'S associated with UARS differ from a conventional OSA bi-level titration?
if for example the hypopnea and FL's were eliminated at say 16/14, do you continue with IPAP looking then to only round off the flow curve?
I wonder why a mfg like Respironics doesn't build that function into its auto bi-pap algorithm, it would seem to me that machine could easily identify that curve you are looking for. Have you done any comparisons with the newer Bi-pap autos to compare to the manual titrations?
Wish Wally was reading this thread, he had "FL's at 18 cm pressure and his sleep was at times a train wreck. I think he has done some experimenting with his pressures and the Bipap Auto will record those events in Bipap mode.
someday science will catch up to what I'm saying...
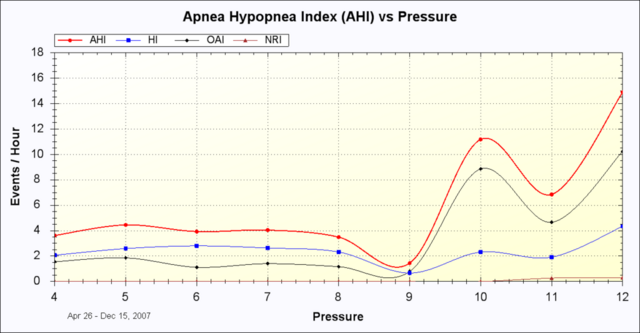
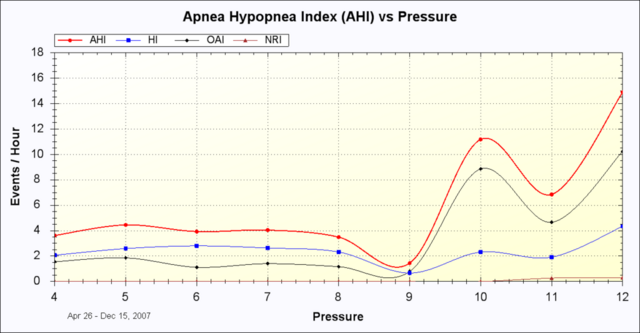
Here's some of my data from James Skinner's Encore Pro Analyzer The first one shows the flow limitations my machine records at various pressures. The second one is my AHI at various pressures. 9.0 seems to be my sweet spot for both, using an autopap. In the second graph you can see how my AHI begins to go up dramatically just after 9.0. It is my understanding that these may be central apneas triggered by the machine. And indeed at the levels of 11 and 12, the data begins to show NR's, probable centrals triggered by the higher levels.
However, my FL's are shown as fairly low in this data. I'm wondering if the 21/hr spontaneous arousals are mostly taken care of by the machine, since I'm now using a higher pressure (9.0) than tech in my titration study set me at (5.0). She never went above 5.0 in my study, so there's no way of knowing whether or not my spontaneous arousals would have disappeared on a higher pressure. Since I cannot measure them directly, there's no way to know. I'm not assuming that the FL's will show them.

_________________
CPAPopedia Keywords Contained In This Post (Click For Definition): Titration, Encore Pro, AHI
However, my FL's are shown as fairly low in this data. I'm wondering if the 21/hr spontaneous arousals are mostly taken care of by the machine, since I'm now using a higher pressure (9.0) than tech in my titration study set me at (5.0). She never went above 5.0 in my study, so there's no way of knowing whether or not my spontaneous arousals would have disappeared on a higher pressure. Since I cannot measure them directly, there's no way to know. I'm not assuming that the FL's will show them.

_________________
CPAPopedia Keywords Contained In This Post (Click For Definition): Titration, Encore Pro, AHI
- Rose
Thread on how I overcame aerophagia
http://www.cpaptalk.com/viewtopic/t3383 ... hagia.html
Thread on my TAP III experience
http://www.cpaptalk.com/viewtopic/t3705 ... ges--.html
Thread on how I overcame aerophagia
http://www.cpaptalk.com/viewtopic/t3383 ... hagia.html
Thread on my TAP III experience
http://www.cpaptalk.com/viewtopic/t3705 ... ges--.html
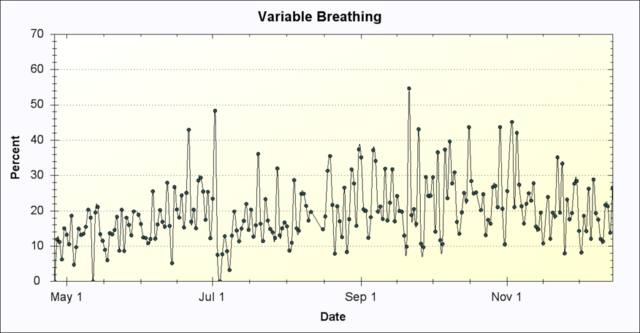
those are good graphs Rose, but what Dr. K is suggesting is it doesn't stop with a zero AHI or total elimination of FL's, as that would be seen as accomplished in your case, but is it enough to eliminate the unstable breathing, this is where they continue to titrate increasing IPAP for obtaining the rounded flow curve (you cannot see that from your report).
There is another graph Jame's report includes (not included on EncorePro version of the reports), but the data is there and it represents the stability of your breathing, maybe James or someone else can think of the report, my mind has gone blank.
There is another graph Jame's report includes (not included on EncorePro version of the reports), but the data is there and it represents the stability of your breathing, maybe James or someone else can think of the report, my mind has gone blank.
someday science will catch up to what I'm saying...
-
Guest
Please read post again. Did I say anything about pressure dips to zero? Nope! I don't know where you get that. Maybe this will help:Snoredog wrote:guy you have no idea what you are talking about other than screwing up this thread where a lot of people want to learn from it.khvn wrote:Whoa, look at that EPAP line in the BIFLEX chart! The machine allows pressure to dip below EPAP--which is a no-no since not enough pressure would allow apnea to pop up here. What saves the day must be our own breath that compensates for the pressure loss and pushes the total pressure up to the safety of the EPAP line again.
dips in x-flex are only momentary and at the beginning of expiration which have been clinically shown not to impede therapy. The therapy splint is always maintained and the pressure never reaches zero.
EPAP dip + pressure from your own breath = EPAP
I wouldn't know how to make it any clearer.
I found the one called "variable breathing." I've never understood what that one was about. Here's the image of that report. My variable breathing has ranged from 55% down to 0%. I still don't understand it, though, in light of the current discussion.Snoredog wrote:those are good graphs Rose, but what Dr. K is suggesting is it doesn't stop with a zero AHI or total elimination of FL's, as that would be seen as accomplished in your case, but is it enough to eliminate the unstable breathing, this is where they continue to titrate increasing IPAP for obtaining the rounded flow curve (you cannot see that from your report).
There is another graph Jame's report includes (not included on EncorePro version of the reports), but the data is there and it represents the stability of your breathing, maybe James or someone else can think of the report, my mind has gone blank.
Edited to add: I found this on the site that Derek made that James has a link to:
http://lewiston.mit.edu/myencore/DailyC ... #VarBreathFraction of Time in Variable Breathing: "Variable breathing" is defined as the situation when a person is not undergoing the quiet steady breathing of several stages of sleep. In particular, according to the Respironics patent" it happens during wakefulness, distress, and REM sleep. This chart may be taken as an indication of how "peaceful" a night was. Since REM sleep is a desirable state, some variable breathing is obviously a good thing.
In my sleep studies, my REM sleep was 17% (first study) and 13% (titration study). I had a lot of stage 4 (28% and 31%). Based on these figures (not ideal, but better than nothing), it seems like my VB should be 13 to 17%, to fit with the idea that some variable breathing, in REM is good. However, most nights VB is a higher percentage than that.
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition): AHI
Last edited by RosemaryB on Tue Dec 18, 2007 12:07 am, edited 2 times in total.
- Rose
Thread on how I overcame aerophagia
http://www.cpaptalk.com/viewtopic/t3383 ... hagia.html
Thread on my TAP III experience
http://www.cpaptalk.com/viewtopic/t3705 ... ges--.html
Thread on how I overcame aerophagia
http://www.cpaptalk.com/viewtopic/t3383 ... hagia.html
Thread on my TAP III experience
http://www.cpaptalk.com/viewtopic/t3705 ... ges--.html
Thanks for coming back and continuing the discussion, Dr. Krakow.
However, when you look at your AHI data in auto mode, you always have to ask how much time was spent at those higher pressures - if you have 3 doughnts and give them all to one child that's one thing - that child has 3 doughnuts. If you have 3 doughnuts to divide the among 9 children, that's different. The first kid may have too many, the 9 will think you're stingy...
So, to profit from AHI by pressure data, you have know how much time that refers to. The top few "AHI by pressure" will always be higher in auto mode, because that's where residual events are solved quickly, and where you spend very little time - the machine drops the pressure down very quickly.
O,
What I understood from Dr. K's posts it that frequently, pressure high enough to eliminate flow limitations when you inhale, will be so hard to breathe out against that you get flow limitation when you exhale. Think of trying to push a heavy box across a smooth polished surface, versus trying to push it across the a carpet. Your movement across the carpet will be jerky.RosmaryB wrote:It is my understanding that these may be central apneas triggered by the machine. And indeed at the levels of 11 and 12, the data begins to show NR's, probable centrals triggered by the higher levels.
However, when you look at your AHI data in auto mode, you always have to ask how much time was spent at those higher pressures - if you have 3 doughnts and give them all to one child that's one thing - that child has 3 doughnuts. If you have 3 doughnuts to divide the among 9 children, that's different. The first kid may have too many, the 9 will think you're stingy...
So, to profit from AHI by pressure data, you have know how much time that refers to. The top few "AHI by pressure" will always be higher in auto mode, because that's where residual events are solved quickly, and where you spend very little time - the machine drops the pressure down very quickly.
O,
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
ozij wrote:Thanks for coming back and continuing the discussion, Dr. Krakow.
What I understood from Dr. K's posts it that frequently, pressure high enough to eliminate flow limitations when you inhale, will be so hard to breathe out against that you get flow limitation when you exhale. Think of trying to push a heavy box across a smooth polished surface, versus trying to push it across the a carpet. Your movement across the carpet will be jerky.RosmaryB wrote:It is my understanding that these may be central apneas triggered by the machine. And indeed at the levels of 11 and 12, the data begins to show NR's, probable centrals triggered by the higher levels.
However, when you look at your AHI data in auto mode, you always have to ask how much time was spent at those higher pressures - if you have 3 doughnts and give them all to one child that's one thing - that child has 3 doughnuts. If you have 3 doughnuts to divide the among 9 children, that's different. The first kid may have too many, the 9 will think you're stingy...
So, to profit from AHI by pressure data, you have know how much time that refers to. The top few "AHI by pressure" will always be higher in auto mode, because that's where residual events are solved quickly, and where you spend very little time - the machine drops the pressure down very quickly.
O,
- Rose
Thread on how I overcame aerophagia
http://www.cpaptalk.com/viewtopic/t3383 ... hagia.html
Thread on my TAP III experience
http://www.cpaptalk.com/viewtopic/t3705 ... ges--.html
Thread on how I overcame aerophagia
http://www.cpaptalk.com/viewtopic/t3383 ... hagia.html
Thread on my TAP III experience
http://www.cpaptalk.com/viewtopic/t3705 ... ges--.html
- jskinner
- Posts: 1475
- Joined: Sat Aug 26, 2006 9:21 pm
- Location: Greenwich, Nova Scotia, Canada
- Contact:
My graph is similar, I start seeing NR's at about 10cm. Because of those NRs I was never been able to successfully get my AHI down below about 10 AHI. I'm wondering if a Bilevel would be able to lower my AHI without triggering the much dreaded NRs/centrals?RosemaryB wrote: In the second graph you can see how my AHI begins to go up dramatically just after 9.0. It is my understanding that these may be central apneas triggered by the machine. And indeed at the levels of 11 and 12, the data begins to show NR's, probable centrals triggered by the higher levels.
-James
Encore Pro Analyzer Author
Facebook Apnea Group
Facebook Apnea Group
-
Guest
Dr. K, you don't know how glad I am that you're back in here in time before the forum elders start to run out of patience and begin to raise their formidable staffs and shoo this unruly upstart out of the temple, or worse yet, cracking my head open...
While I'm here though, I must say that the following are the most perculiar things about your APAP-to-BIPAP crossover that hooked me bad:
(1) What is this mystery behind the bilevel that can afford you such a tremendous, but at the same time, agreeable treatment shift???
(2) No less outrageous is the reason why your old APAP didn't push on your hi setting to the point where it converges with your new hi on the BIPAP??? malfunctioning or bad algorithm?
Gotta run...
While I'm here though, I must say that the following are the most perculiar things about your APAP-to-BIPAP crossover that hooked me bad:
(1) What is this mystery behind the bilevel that can afford you such a tremendous, but at the same time, agreeable treatment shift???
(2) No less outrageous is the reason why your old APAP didn't push on your hi setting to the point where it converges with your new hi on the BIPAP??? malfunctioning or bad algorithm?
Gotta run...










