What can you do anyway?
-
Ionizer
- wading thru the muck!
- Posts: 2799
- Joined: Tue Oct 19, 2004 11:42 am
Liam, who should use his brain to make his buying decisions and not his wallet.
I'm disappointed I have not convinced you with my logic couched in esoteric analogies. Need I make it clearer? Mexico...middle of summer...heat on full blast.
That's what you get with a fixed pressure cpap. Heat in the winter...cooling in the summer. That's what you get with an auto. The guy that invented the first cpap used a vacuum run in reverse (got an old vacuum around? that would be cheaper than a fixed cpap)
The Pro is not upgradeable to an auto. (as far as I've heard)
regards,
wader, who has probably put his foot in his mouth and offended Liam, but hopes not.
I'm disappointed I have not convinced you with my logic couched in esoteric analogies. Need I make it clearer? Mexico...middle of summer...heat on full blast.
That's what you get with a fixed pressure cpap. Heat in the winter...cooling in the summer. That's what you get with an auto. The guy that invented the first cpap used a vacuum run in reverse (got an old vacuum around? that would be cheaper than a fixed cpap)
The Pro is not upgradeable to an auto. (as far as I've heard)
regards,
wader, who has probably put his foot in his mouth and offended Liam, but hopes not.
Last edited by wading thru the muck! on Wed Feb 02, 2005 9:37 pm, edited 1 time in total.
-
Sleeping With The Enemy
- Posts: 454
- Joined: Tue Jan 25, 2005 11:54 pm
- Location: Minnesota
Statistical Summary
More information on my experience with being on AutoSet Spirit for 90 hours spanning 12 nights. Averaging 7.26 hrs/day
Pressure 95th centile: 12.4 cm H20
Median Pressure: 8.1 cm H20
Maximum Pressure: 15.6 cm H20
Leak 95th centile: 0.00 l/sec
Median Leak: 0.00 l/sec
Maximum Leak: 2.01 l/sec
AHI: 5.8 events per hour
AI: 0.5 events per hour
HI: 5.3 events per hour
Time in Apnea: 0.2% Mask On Time
These are my readings for the 12 nights. During sleep study I had 67 episodes of apnea in a 60 minute time frame. My 02 saturations dropped into the low 80's.
Pressure 95th centile: 12.4 cm H20
Median Pressure: 8.1 cm H20
Maximum Pressure: 15.6 cm H20
Leak 95th centile: 0.00 l/sec
Median Leak: 0.00 l/sec
Maximum Leak: 2.01 l/sec
AHI: 5.8 events per hour
AI: 0.5 events per hour
HI: 5.3 events per hour
Time in Apnea: 0.2% Mask On Time
These are my readings for the 12 nights. During sleep study I had 67 episodes of apnea in a 60 minute time frame. My 02 saturations dropped into the low 80's.
Hi Muck,
That was a great reply to hhunt re the 95% solution! This kind of info is wonderful - now I need to get a reader for my smart card with Rem auto c-flex from CPAP.com - after I get reimbursed from insurance for initial purchase!
Please stay tuned as I'm sure there will be many questions then, when I try to figure out what is really happening after the lights go out.
That was a great reply to hhunt re the 95% solution! This kind of info is wonderful - now I need to get a reader for my smart card with Rem auto c-flex from CPAP.com - after I get reimbursed from insurance for initial purchase!
Please stay tuned as I'm sure there will be many questions then, when I try to figure out what is really happening after the lights go out.
unclebob
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
hi hhunt,
You wrote:
On an autopap, I think of it this way:
"It took pressures of 12.4 or below to prevent and/or deal with events 95% of the time I was sleeping."
Why does it make a difference which way you look at it? Well, if a person is going to be receiving a straight cpap to be set at one pressure blowing at them all night, they do want to set that single pressure to be high enough to take care of you most of the time.
However, if a person wants the comfort of sleeping with less pressure until 10, or 11, or 12.4 is actually needed during the night, then an autopap is a better choice.
When considering whether an autopap or a straight cpap would suit you, you'd need to look at each night's data instead of looking at a single "95%" number from 12 nights all lumped together. Look at each of the twelve nights and look at how many minutes of your sleep were spent at each of the pressures used during those individual nights.
You might be surprised to see that very little time was really spent up at 12.4 and a lot more time was spent down at varying lower pressures.
Example: here's a chart from my Respironics REMstar auto for a single night.
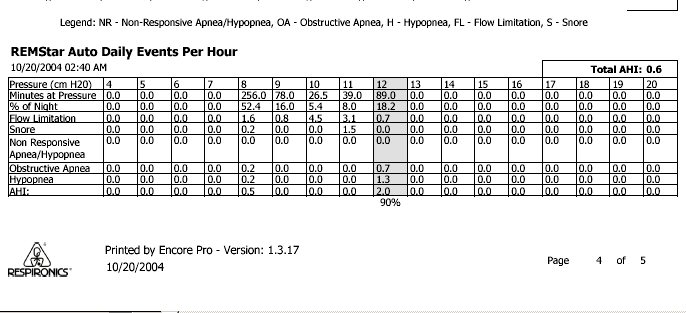
You'll see that the chart highlights the column for the pressure of 12 and labels that the "90 %" pressure.
But....look on the chart at the amount of time spent sleeping at pressures lower than 12 during that eight hour sleep session.
Minutes at pressure 12: 89 minutes
Minutes at pressure 11: 39 minutes
Minutes at pressure 10: 26.5 minutes
Minutes at pressure 9: 78 minutes
Minutes at pressure 8: 256 minutes
Much more than half my entire night was spent at several pressures below the "90% pressure". In fact, better than half the night was spent down at the lowest pressure ( 8 ) that I had set the machine's range for (8-16). That's true of every night I ever look at - much more time is spent well below the "90% pressure" on my autopap.
The less time one must spend up at a single high pressure, the less chance for springing mask leaks, swallowing air, having trouble exhaling, etc. I'd much rather spend as much time as possible at lower pressures, than have a steady blast of a single high pressure all night long. Especially if it's a pressure that I don't even need most of the time while I'm sleeping.
It makes no difference to me who uses cpap and who uses autopap, or bipap...whatever. I have no reason to push anyone toward "autopap" other than autopap simply gives a more comfortable treatment for many people, imho. People can do fine on straight cpap, too. As long as I have my autopap, I'm happy.
I've gone on and on at length about this, simply because I'd be very sorry to see people misinterpret what a DME says about what the "90% or 95%" pressure and think it meant a trial autopap had been using that particular high pressure almost constantly while they slept.
I also think there is a bit of misconception (perhaps on my part!) if someone thinks that autopaps are designed only to react to events. I don't think putt-putting along and simply waiting for apneas or hypopneas to happen before the autopap jumps into action is how they work. Certainly an event can sneak by occasionally, but my understanding is that the autopap is almost constantly "reading" the person's breathing and making smooth proactive pressure moves to prevent the throat from closing and prevent most events from happening at all.
I'm not a doctor or health care professional. Just my opinion.
You wrote:
hhunt, as Wader said, the 95% pressure number doesn't mean the autopap was blowing that pressure at you most of the night. If the doctor or DME had you doing a 12 day trial on autopap with the intention of finding a single pressure that takes care of you, and intended to put you on straight cpap after the autopap finds the highest pressure you might need...that's one thing. Yes, then the figure the software states as the "95% pressure" is useful to know.12.4 is what the autopap "clocked" me at 95% of the time for the 12 nights that I wore it in my own home from the DME, that is how she figured my pressure for the cpap machine.
On an autopap, I think of it this way:
"It took pressures of 12.4 or below to prevent and/or deal with events 95% of the time I was sleeping."
Why does it make a difference which way you look at it? Well, if a person is going to be receiving a straight cpap to be set at one pressure blowing at them all night, they do want to set that single pressure to be high enough to take care of you most of the time.
However, if a person wants the comfort of sleeping with less pressure until 10, or 11, or 12.4 is actually needed during the night, then an autopap is a better choice.
When considering whether an autopap or a straight cpap would suit you, you'd need to look at each night's data instead of looking at a single "95%" number from 12 nights all lumped together. Look at each of the twelve nights and look at how many minutes of your sleep were spent at each of the pressures used during those individual nights.
You might be surprised to see that very little time was really spent up at 12.4 and a lot more time was spent down at varying lower pressures.
Example: here's a chart from my Respironics REMstar auto for a single night.
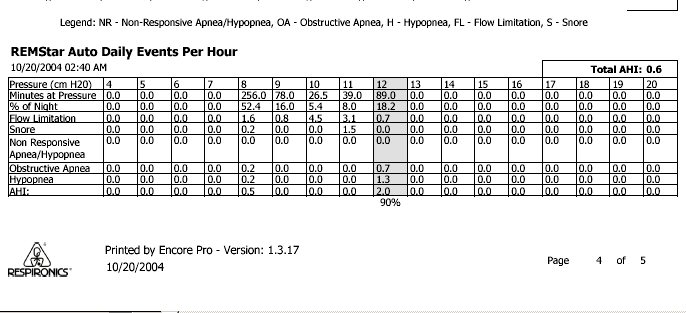
You'll see that the chart highlights the column for the pressure of 12 and labels that the "90 %" pressure.
But....look on the chart at the amount of time spent sleeping at pressures lower than 12 during that eight hour sleep session.
Minutes at pressure 12: 89 minutes
Minutes at pressure 11: 39 minutes
Minutes at pressure 10: 26.5 minutes
Minutes at pressure 9: 78 minutes
Minutes at pressure 8: 256 minutes
Much more than half my entire night was spent at several pressures below the "90% pressure". In fact, better than half the night was spent down at the lowest pressure ( 8 ) that I had set the machine's range for (8-16). That's true of every night I ever look at - much more time is spent well below the "90% pressure" on my autopap.
The less time one must spend up at a single high pressure, the less chance for springing mask leaks, swallowing air, having trouble exhaling, etc. I'd much rather spend as much time as possible at lower pressures, than have a steady blast of a single high pressure all night long. Especially if it's a pressure that I don't even need most of the time while I'm sleeping.
It makes no difference to me who uses cpap and who uses autopap, or bipap...whatever. I have no reason to push anyone toward "autopap" other than autopap simply gives a more comfortable treatment for many people, imho. People can do fine on straight cpap, too. As long as I have my autopap, I'm happy.
I've gone on and on at length about this, simply because I'd be very sorry to see people misinterpret what a DME says about what the "90% or 95%" pressure and think it meant a trial autopap had been using that particular high pressure almost constantly while they slept.
I also think there is a bit of misconception (perhaps on my part!) if someone thinks that autopaps are designed only to react to events. I don't think putt-putting along and simply waiting for apneas or hypopneas to happen before the autopap jumps into action is how they work. Certainly an event can sneak by occasionally, but my understanding is that the autopap is almost constantly "reading" the person's breathing and making smooth proactive pressure moves to prevent the throat from closing and prevent most events from happening at all.
I'm not a doctor or health care professional. Just my opinion.
I think it's a fair enough question to ask, whether or not everyone needs auto-PAP. Different people have different situations. Me, I bought the straight CPAP because it was a question of $1000 versus $2000 for the machine -- and no, don't say "you should have bought it from cpap.com" -- I live in Australia, I can't do that. (And yes, that's Australian dollars above). And no, my insurance only covers a $500 rebate on the machine, so, yes, it was a question of $$$$.
I did discuss this with my sleep specialist recently, because my parents said they'd help me to get an auto-CPAP if it would help, and my doctor said basically, wait until we get the results from another sleep study. Because my pressure of 12 is considered to be "moderate". The benefit of an auto-PAP is much more obvious for someone who needs a higher pressure. I don't need as high a pressure because, though I have very severe sleep apnea (RDI=110 (!!!)) most of the incidents are hypopneas rather than apneas.
But if it turns out that I do have a notable variation -- say, between when I'm on my back or when I'm on my side -- then it would be more justifiable to get an auto-PAP, than if the sleep study shows that my pressure needs don't vary a lot. I mean, it would be a waste of money to get another machine if I'm okay on my existing one -- the money could well be better spent on other things that could help improve my sleeping environment.
Everybody's different; not everyone has the same needs, money, insurance situation or whatever.
I did discuss this with my sleep specialist recently, because my parents said they'd help me to get an auto-CPAP if it would help, and my doctor said basically, wait until we get the results from another sleep study. Because my pressure of 12 is considered to be "moderate". The benefit of an auto-PAP is much more obvious for someone who needs a higher pressure. I don't need as high a pressure because, though I have very severe sleep apnea (RDI=110 (!!!)) most of the incidents are hypopneas rather than apneas.
But if it turns out that I do have a notable variation -- say, between when I'm on my back or when I'm on my side -- then it would be more justifiable to get an auto-PAP, than if the sleep study shows that my pressure needs don't vary a lot. I mean, it would be a waste of money to get another machine if I'm okay on my existing one -- the money could well be better spent on other things that could help improve my sleeping environment.
Everybody's different; not everyone has the same needs, money, insurance situation or whatever.
The best cure for insomnia is to get a lot of sleep. (W. C. Fields)
- wading thru the muck!
- Posts: 2799
- Joined: Tue Oct 19, 2004 11:42 am
rested gal,
Thanks for posting that chart. The info was what I was refering to and demonsrtates perfectly the benefit of an auto.
RubyKat,
I am in no way trying to convince you to but an auto-pap. You obviously are, until further notice, convinced otherwise. I would just like to clear up a few of your statements so that other browsers do not get mislead by them. I'll also restate a few where you are on the right track.
Thanks for posting that chart. The info was what I was refering to and demonsrtates perfectly the benefit of an auto.
RubyKat,
I am in no way trying to convince you to but an auto-pap. You obviously are, until further notice, convinced otherwise. I would just like to clear up a few of your statements so that other browsers do not get mislead by them. I'll also restate a few where you are on the right track.
- If you live in Australia you can buy from cpap.com
- A person with a titrated pressure of 12cm is probably at the pressure where an auto would do them the most good.
- An RDI of 110 is a reason an auto may be of little benefit to you. At that you may spend most, if not all of the time at the pressure required to resolve those 110 events per hour.
- Variations in requirements due to varied sleep position is a good reason to get an auto. It is one of the reasons I used to talk my Doc into prescribing one for me.
Sincerely,
wading thru the muck of the sleep study/DME/Insurance money pit!
wading thru the muck of the sleep study/DME/Insurance money pit!
-
Sleeping With The Enemy
- Posts: 454
- Joined: Tue Jan 25, 2005 11:54 pm
- Location: Minnesota
REASON
I want everyone to be clear that the only reason I posted this topic like this is so that I can build my case. I want to be sure that the autopap would be most beneficial for me. I need convincing evidence in the form of articles, research, etc., so I can bring this to my MD and say, hey, look at this infomation. Hopefully, it would be convincing and educational for her to make a decision on my behalf. You have to have a script that says autopap from my understanding. Also, I cannot outright buy an autopap. My tranny in my van just went out and it will cost $2100. I HAVE TO HAVE MY INSURANCE PAY FOR THIS MACHINE. I HAVE BLUE PLUS MINNESOTA
-
Sleeping With The Enemy
- Posts: 454
- Joined: Tue Jan 25, 2005 11:54 pm
- Location: Minnesota
clarification
Chrisp,
To clarify, with those pressures the DME has my Remstar Plus with C-Flex and humidification set at 12.4
To clarify, with those pressures the DME has my Remstar Plus with C-Flex and humidification set at 12.4
- wading thru the muck!
- Posts: 2799
- Joined: Tue Oct 19, 2004 11:42 am
hhunt,
I think you would do better with you your Doc if you tell her " I've spoken to many people who on successfully using a cpap for treatment of OSA. They all tell me that in their experience using an auto-pap is the best way to insure long term every night use." Tell her all our rational. Tell her you've thought long and hard about how this would work for you. Tell her you think this machine is what will work for you.
You may also what to talk with somebody at your insurance. Just because your doctor prescribes an auto does not mean the insurance will pay for one. Find out if they make you rent first (some do). That may actually help. If you can get the Doc to write for an auto and rent one, when it comes time to buy, if the machine you have is working for you, they are very unlikely to make you buy a different one.
I'd also find out some prices from the recommended DMEs and then calculate your deductable and out-of-pocket based on those prices. You may find that being it's early in the year, the total out-of-pocket is more than what it would cost you to buy out right from cpap.com.
Keep an open mind, completely work out all the angles and then decide what's the best resolution.
I think you would do better with you your Doc if you tell her " I've spoken to many people who on successfully using a cpap for treatment of OSA. They all tell me that in their experience using an auto-pap is the best way to insure long term every night use." Tell her all our rational. Tell her you've thought long and hard about how this would work for you. Tell her you think this machine is what will work for you.
You may also what to talk with somebody at your insurance. Just because your doctor prescribes an auto does not mean the insurance will pay for one. Find out if they make you rent first (some do). That may actually help. If you can get the Doc to write for an auto and rent one, when it comes time to buy, if the machine you have is working for you, they are very unlikely to make you buy a different one.
I'd also find out some prices from the recommended DMEs and then calculate your deductable and out-of-pocket based on those prices. You may find that being it's early in the year, the total out-of-pocket is more than what it would cost you to buy out right from cpap.com.
Keep an open mind, completely work out all the angles and then decide what's the best resolution.
Sincerely,
wading thru the muck of the sleep study/DME/Insurance money pit!
wading thru the muck of the sleep study/DME/Insurance money pit!
Interesting followup....
I was told today by my sleep doctor that the reason why Auto-PAP is probably not right for me is that Auto-PAP only detects ... (ok, it's early, I'm forgetting the medical terminology) events where you actually stop breathing. He says that there are a number of apnea events, not all of them involve a full stoppage of breathing, some (and these are the sort I apparently have a lot of) involve awakening BEFORE the breathing stops enough to be detected as a breath stoppage.
His opinion is that someone like me on an auto-pap would actually NOT get much benefit, because the machine would detect that I was breathing fine all night, and so would give me the minimum pressure.
Now, I don't know if he was just (ahem) blowing hot air, but that was his opinion.
And in the "As always, the medical communities left and right hands don't speak" category, there's another sleep doctor, at a different clinic, that Kim, my DME, says ONLY prescribes APAP.
So... I don't know what to believe right now, but I CERTAINLY don't want to shell out 50% more out of pocket for something which is going to do me a DISSERVICE.
Liam, who wonders if bi-paps really swing both ways.
I was told today by my sleep doctor that the reason why Auto-PAP is probably not right for me is that Auto-PAP only detects ... (ok, it's early, I'm forgetting the medical terminology) events where you actually stop breathing. He says that there are a number of apnea events, not all of them involve a full stoppage of breathing, some (and these are the sort I apparently have a lot of) involve awakening BEFORE the breathing stops enough to be detected as a breath stoppage.
His opinion is that someone like me on an auto-pap would actually NOT get much benefit, because the machine would detect that I was breathing fine all night, and so would give me the minimum pressure.
Now, I don't know if he was just (ahem) blowing hot air, but that was his opinion.
And in the "As always, the medical communities left and right hands don't speak" category, there's another sleep doctor, at a different clinic, that Kim, my DME, says ONLY prescribes APAP.
So... I don't know what to believe right now, but I CERTAINLY don't want to shell out 50% more out of pocket for something which is going to do me a DISSERVICE.
Liam, who wonders if bi-paps really swing both ways.
-
Guest
THANKS!!! Continuing to Build My Case
Thanks to everyone, especially those of you who go into such great detail and really put thought and care into your replies. I APPRECIATE ALL OF THE REPLYS AS I CONTINUE TO FORM MY OPINION ABOUT THIS!
Interesting doctor...
Liam1965 wrote:Interesting followup....
I was told today by my sleep doctor that the reason why Auto-PAP is probably not right for me is that Auto-PAP only detects ... (ok, it's early, I'm forgetting the medical terminology) events where you actually stop breathing. He says that there are a number of apnea events, not all of them involve a full stoppage of breathing, some (and these are the sort I apparently have a lot of) involve awakening BEFORE the breathing stops enough to be detected as a breath stoppage.
If your doctor actually scored your raw PSG sleep data (or at least carefully analyzed your many pages of raw PSG data) then he may actually have a point there. However, not only would your (AutoPAP-preclusive) distribution of obstructive sleep events be a bit on the rare side, but your sleep doctor would be preeminently rare! Most sleep doctors rarely if ever delve into the raw PSG data, and most sleep doctors do not know the algorithmic ins-and-outs of AutoPAP sleep event detection/response. Rather most sleep doctors end up with a text and tabular summary of what occured during the overnight PSG. If your sleep doctor has a bias against AutoPAPs and simply intends to verbally defend that bias, then maybe he's not such a rare sleep doctor after all!
But yes, there really are some sleep-disordered-breathing (SDB) cases where patients are actually better on CPAP than AutoPAP. Modern AutoPAPs attempt to keep obstructive sleep events at bay in a proactive manner even more than they do as a matter of response or reaction to apneas/hypopneas. They do this primarily with two proactive strategies: 1) they maintain pressure after an initial apnea/hypopnea has been detected, hoping to proactively stave off subsequent apneas/hypopneas, and 2) they look for obstructive "precursors" by the way of breath waveform and even volume. Those obstructive precursors can be snoring, lesser flow limitations, and even lesser flow restrictions yet (known as "intermediate respiratory cycles"). For rare lack of adequate obstructive precursors, exactly as your doctor suggests, an AutoPAP would be reduced to determining your necessary pressure purely by proactive algorithmic strategy number one above coupled with a pure response for any and all subsequent events not proactively addressed by pressure.
Curious, Liam, did you snore before CPAP? If so, then your doctor was, indeed, either giving you a line of B.S. or he just doesn't understand how an AutoPAP triggers.
Re: Interesting doctor...
Sometimes, but not always. When we first suspected Apnea, my wife started paying particular attention (she requires much less sleep than I, and apparently enjoys watching me sleep when she wakes early and has nothing to do).-SWS wrote:Curious, Liam, did you snore before CPAP? If so, then your doctor was, indeed, either giving you a line of B.S. or he just doesn't understand how an AutoPAP triggers.
Anyway, she said I SOMETIMES snore, generally on the nights when I'm all stuffed up and am mouth-breathing, but that she noticed some minor hitches in my breathing even when I wasn't snoring.
Liam, who can't attest to any of it, he has a tendency to sleep through his snoring(*).
(* Actually not, or else I wouldn't need to be on CPAP, would I. )












