SAG,StillAnotherGuest wrote:Well, my first thought would be that where you take measurements is academic. If you know the characteristics of the machine tubing, planned leaks (mask vent rate) and the unplanned leaks are relatively constant, you could calculate everything you need to know no matter where you take the measurements. Further, the purpose of ASV is simply to supply ventilation during periods of reduction (specifically central apnea) and both machines do this quite well.Banned wrote:I assumed, until now, the Respironics BiPAP SV had the ancillary sensor line. I know with my Adapt SV when I stop breathing (hold my breath) the Adapt SV starts ramping to provide much more air by my next breath. When ResMed says on a "breath-by-breath" basis, it's true. Exhalation (EEP) is fixed, but I can watch the Inhalation pressure change with each breath on the Adapts LCD. If I had serious issues with stopping breathing at night (which I do) I would be hard pressed to want to snuggle up to a Respironics BiPAP SV without any feedback from the mask.
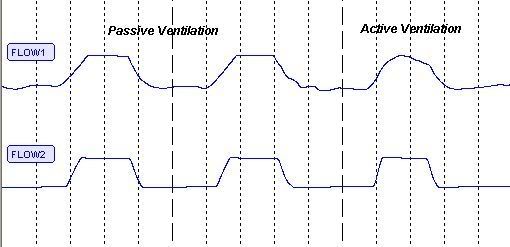
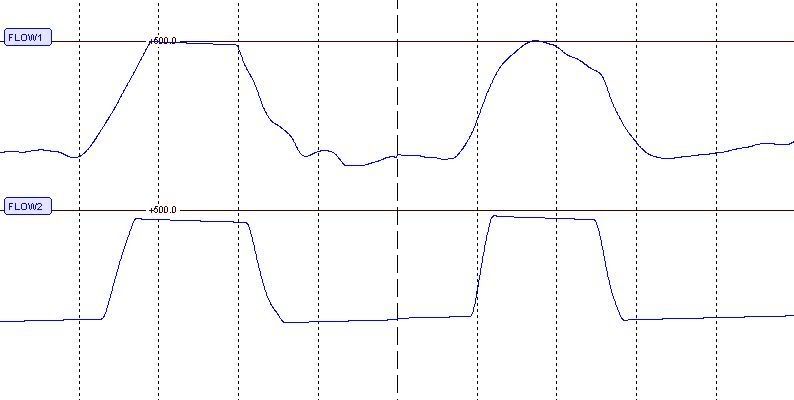
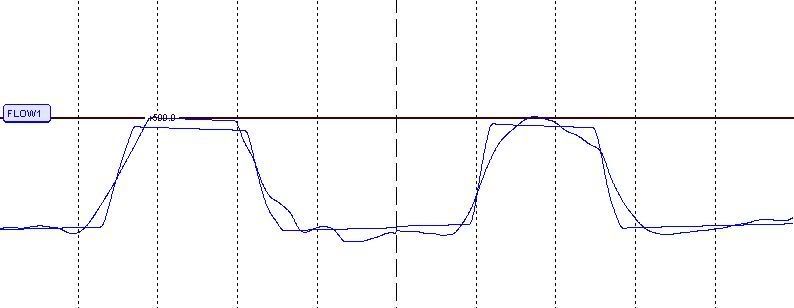
The advantage of measuring proximal airway pressure (pressure at the mask), would be that (theoretically) you could match up machine breaths to patient breaths more easily. I believe that measuring breaths at the machine is less sensitive when there is patient effort (patient is actively particiapting in ventilation, rather than letting the machine do all the work), as shown in this graph of pressure measurements taken in an AdaptSV circuit at patient airway (Flow 1) and machine (Flow 2):
When the breath is largely from the machine, both waveforms are similar, but during periods of greater patient effort, changes are seen in the patient waveform that are not reflected in the machine waveform. So if the ASV is trying to recreate a breath pattern that closely mirrors patient effort (more like PAV technology), then this might be a better way to do that.
Now, one might ask, what value is this information? If you're asleep, having a central apnea, and the ASV is simply trying to generate a breath that is tailored not for comfort, but rather to a volume to stabilize breathing, then I'm thinking, "Who cares?" I mean, great, perhaps you can duplicate waveforms so the waveforms "look" the same, but you're ASLEEP! So is this really just another Wake comfort measure, or is there true physiological value to this?
Besides, with the newer bilevel technologies, there aren't any more square waveforms, they're all much more patient-friendly.
Again, this boils down to "what is it you're trying to fix?" If you're trying to fix CSA, you have to see that machine performance is addressing exactly that. While it may be attractive to say. "Look at that proximal patient line, that must really DO something!", you really have to see which machine fixes the underlying problem better.
This is also another good example demonstrating that the waveform out the machine is not necessarily the same as what the patient is getting, so "treating the waveform" can get you in a real rut. If the machine generates a square waveform, and patient effort is passive, then it will have a flat appearance as flow appears constant. This does not signify a flow limitation, only that the machine is delivering steady pressure.
SAG
Good points & well put.
So which machine do the patients prefer & which machine delivers best ? that is the bottom line !.
DSM