Hello,
I have been dealing with chronic fatigue for about three and a half years and was recently diagnosed with upper airway resistance syndrome. There is remarkably little information about this condition (and there are remarkably few doctors equipped to address it), so I am feeling a little dispirited. I would like to hear from others who are successfully treating UARS -- what methods you used (nasal optimazation (sprays, breathing strips, sinus or turbinate surgery); CPAP (type of machine, mask, and pressure settings); oral appliance; or apnea surgery). Really, any and all information will be most appreciated.
Thank you!
Seeking Upper Airway Resistance Syndrome Success Stories
Re: Seeking Upper Airway Resistance Syndrome Success Stories
kkt,
I have a summary of this medical report that was published in this magazine about UARs in 2011:
http://www.chestnet.org/
You can't access this anymore b/c it now requires a subscription.
A couple of years ago I could access it and even posted here a nice summary.
But in the meantime a competing Sleep Website copied it. So this time I copy it from them:
As you said, not much could be done about treating URS but to continue CAPAing.
The Sleep Doc, Barry Krakow, has UARs himself and recommends a BIPAP machine (BiLevel in Resmed). He uses hi pressure if around 18 cm to treat his URS. That's why he uses a BiPAP which allows him to reduce the pressure for exhalation.
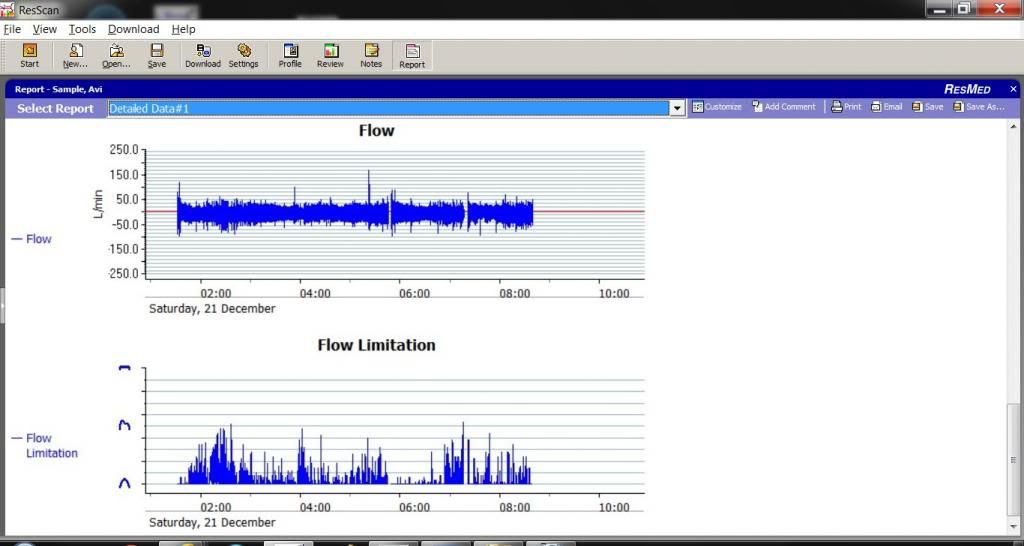
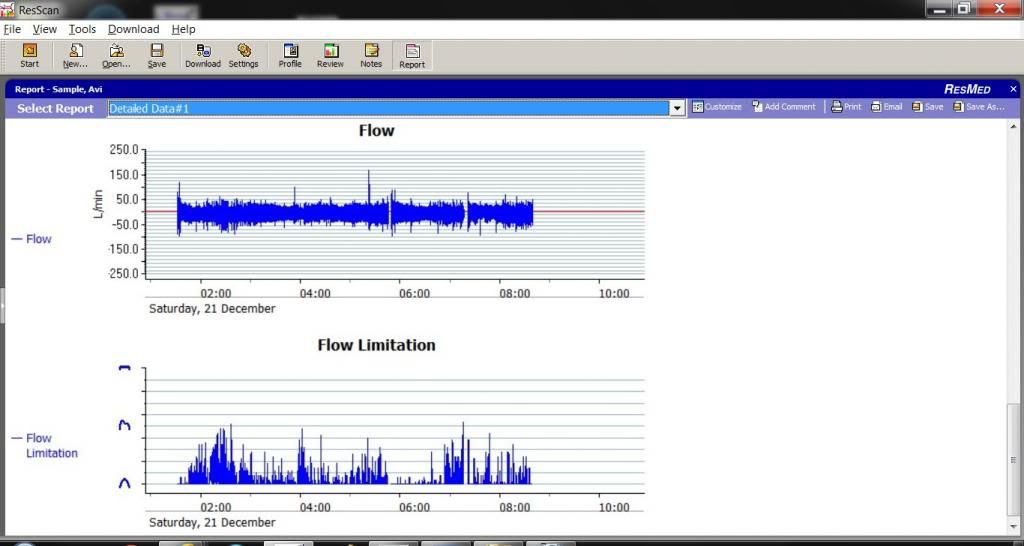
Resmed machines, combine the UARs under Flow Limitations (FL) and provide a graph of it. They measure the level of the FL
by the degree of flattening of the Respiration flow wave curve. FL causes the normal rounded top of the respiration wave curve to flatten and resemble the shape of the letter "r".
I myself have some FL to certain degree which I can follow on my Resmed S9 Autoset machine by using ResScan software.
Here is a recent example:
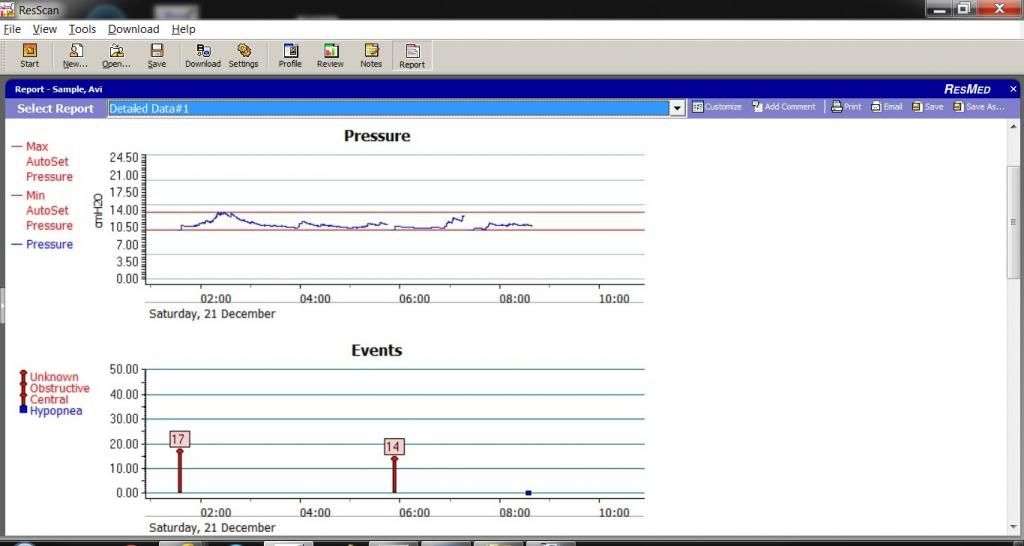
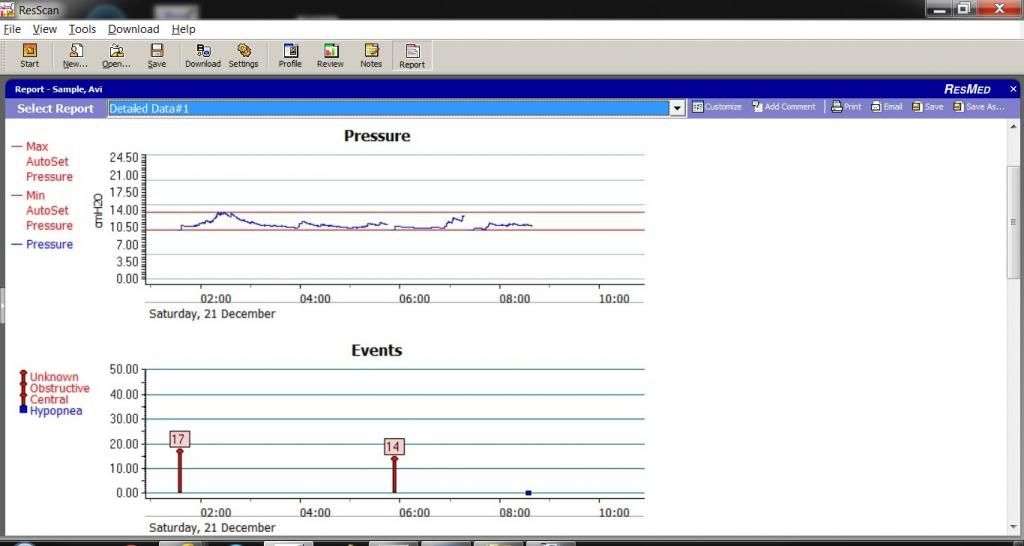
The following are ResScan graphs of the pressure and events associated with the above:
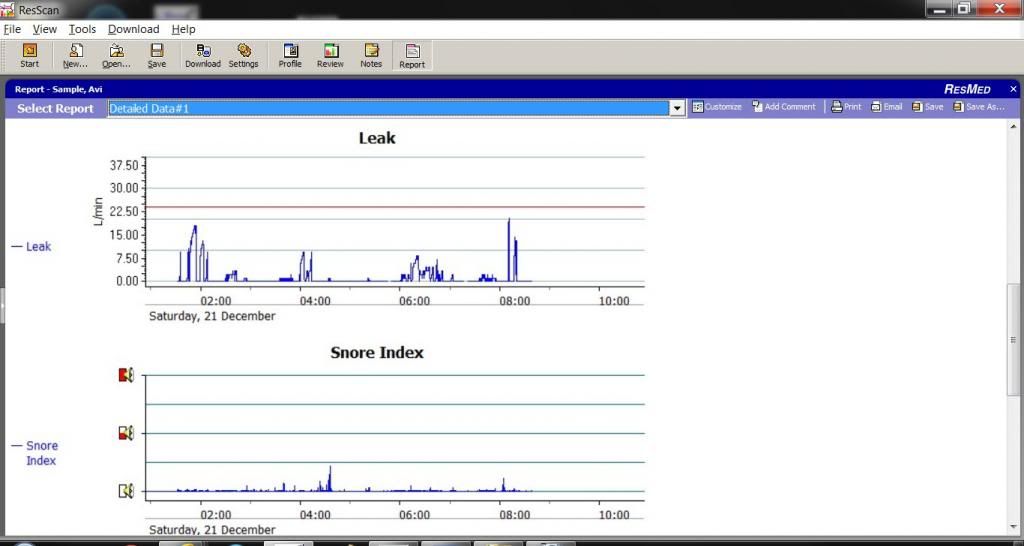
And these 2 graphs I also check:
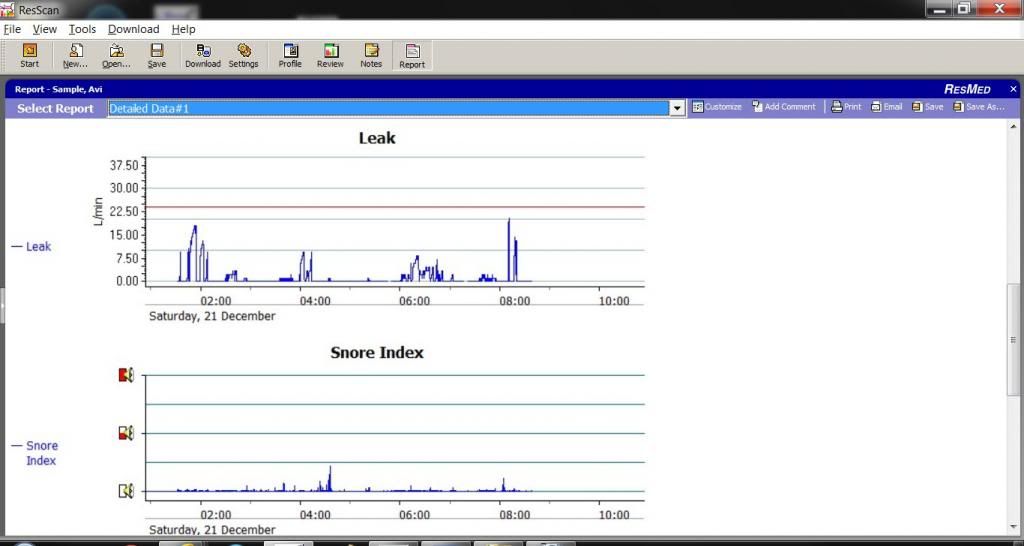
IMO, my FL is caused by my stuffy nose. I have Vasomotor Rehinitis which is effected by air flow, and its temperature, from the APAP. This Rehinitis is not an allergy one. My nose gets also stuffy when I touch the cold marble counter top in my kitchen.
So before I mask I blow my nose to get rid of the WHOLE junk. And if it gets stuffy again before I fall asleep I blow it again and again.
Here is the summary that I mentioned above and which I took this time from:
http://www.apneaboard.com/forums/Thread ... e-Syndrome
The top U.S. maven in this field Dr Guilleminault, is lead author.
Upper Airway Resistance Syndrome
Over the past few years, numerous articles have been published that have increased our understanding of the features of upper airway resistance syndrome (UARS). UARS has been previously described as a distinct clinical syndrome, although there is ongoing controversy and some consider it to be part of a spectrum of sleep-disordered breathing that includes primary snoring, obstructive hypopnea syndrome (OHS), and obstructive sleep apnea syndrome (OSAS). However, patients with UARS present with different polysomnographic abnormalities and do not meet generally accepted criteria for either apneas or hypopneas. The lack of education about UARS in the medical community has allowed these patients to go undiagnosed and untreated. Increased research into UARS will help us to identify the optimal treatment for these patients, as well as to educate clinicians about this relatively under-recognized population.
Introduction
UARS is characterized by abnormal respiratory effort, nasal airflow limitation, absence of obstructive sleep apnea, minimal pulse oximetry fluctuation with oxygen saturation nadirs >92%, and frequent nocturnal arousals or reflex brainstem activation. It was first recognized in children in 1982, although the term UARS was not used until the first adult cases were reported in 1993. The incidence and prevalence of UARS has been systematically investigated in a recent São Paulo epidemiologic study (discussed below in "Epidemiologic Studies of UARS"). Prior to the São Paulo study, some have reported prevalence rates of 8% to 20% in the literature.5,6 We now know that this syndrome has recognizable clinical and polysomnographic characteristics that differ from those observed in patients with OHS/OSAS. UARS occurs in all age groups without any clear sex preferences, although some studies suggest that women may be at increased risk. UARS has the potential for significant impact on the daytime functioning and quality of life in untreated patients and there is growing evidence to suggest that symptoms are progressive without treatment.
Treatment
The optimal treatment for patients with UARS is not currently known. Continuous positive airway pressure (CPAP) has been quite useful in the treatment of sleep-disordered breathing and there are some notable positive results in CPAP treatment of UARS. In a study of 15 heavy snorers with clinical evidence of UARS, treatment with nasal CPAP was associated with decreases in observed nocturnal arousals on polysomnography and decreases in mean sleep latency times on multiple sleep latency testing (MSLT) after several nights of treatment.3,36 A follow-up study of 15 subjects (in the original description of UARS) with daytime sleepiness and fatigue and who had undergone a therapeutic trial of positive pressure therapy reported similar findings. After treatment with approximately a month of nasal CPAP, significant improvements were seen in mean sleep latency times on MSLT (5.3 minutes vs 13.5 minutes), Pes nadir pressure (-33.1 cm H2O vs -5.3 cm H2O), amount of slow-wave sleep (1.2% vs 9.7%), and EEG arousals (31.3 vs 7.9 events/hour of sleep). Along with an improvement in sleep latency times on MSLT, there were subjective reports of improved daytime symptoms. Lastly, in a study of 130 postmenopausal women with chronic insomnia and evidence of UARS (n=62) or normal breathing (n=68), treatment with either nasal turbinectomy or nasal CPAP was associated with improvements in subjective reports of sleep quality as measured with a visual analog scale as well as mean sleep latency times on polysomnography. Despite the growing body of evidence supporting the use of positive pressure therapy for UARS patients, it remains difficult to obtain therapy. In a follow-up study of more than 90 patients conducted 4 to 5 years after the initial diagnosis of UARS was made, none of the subjects were receiving CPAP treatment; the main rationale given was that their insurance provider declined to provide the necessary equipment. Formal follow-up clinical evaluations of these patients noted significant worsening in their sleep-related complaints, with increased reports of fatigue, insomnia, and depressive mood. More disturbingly, prescriptions for hypnotics, stimulants, and antidepressants increased more than fivefold.
Other interventions, such as surgery or oral appliances, have also been used with some success in the treatment of patients with UARS. Procedures such as uvulopalatopharyngoplasty, laser-assisted uvuloplasty (LAUP), septoplasty with turbinate reduction, genioglossus advancement, and radiofrequency ablation of the palate have all been described in the literature.37-40 A study of LAUP in nine patients with UARS who underwent uvulopalatopharyngoplasty (n=2), multilevel pharyngeal surgery (n=1), or LAUP (n=6) reported improvements in subjective daytime sleepiness as measured with Epworth Sleepiness Scale scores. In the two patients for whom postoperative polysomnographic data was available, significant improvements in Pes nadir pressures were seen. But patients had several interventions and it is difficult to assess which one was successful. A study of 14 patients with UARS who underwent radiofrequency ablation of the palate also reported improvement in subjective sleepiness, with concurrent improvements in Pes nadir levels and reports of snoring. However, prior reviews of the available literature have noted that many of the studies evaluated small numbers of patients, consisted of uncontrolled case reports or series without clear characterization of the subjects enrolled, and had no consistent end points for an adequate evaluation of efficacy. Further investigation is required to determine the specific role for surgical intervention in these patients. Other authors have also reported successful treatment of UARS with use of oral appliances, although these studies suffer from the same limitations as the surgical literature. In children, orthodontic approaches, such as maxillary distraction or use of expanders, have also shown promising results.
Conclusion
Although UARS has a symptomatology close to the one seen in patients with OSAS, there are distinct clinical differences between the two syndromes. In clinical studies, it is seen more in younger, slim subjects and in premenopausal women; it is more commonly associated with an increase in vagal tone during sleep than with sympathetic hyperactivity (as seen in association with apnea and hypopnea and oxygen desaturation).21 Can individuals with UARS become patients with OSAS? Guilleminault and colleagues suggested that weight increase (with development of a chest-bellow problem related to abdominal obesity) and the association of the supine position and sleep (leading to a restrictive impairment and secondary oxygen saturation drop and sympathetic hyperactivity) will lead to passage from one presentation to another with different complications; but more data are needed from additional systematic, longitudinal studies. UARS is underdiagnosed owing to unfamiliarity with the syndrome and the lack of polysomnographic criteria for either hypopneas or apneas that are associated with other types of sleep-disordered breathing. The advent of use of an esophageal catheter for esophageal pressure measurement (Pes) has allowed clinicians to more clearly identify patients with UARS. Although Pes measurement is the most sensitive method available to detect the abnormal respiratory events in UARS, it has not been used widely for several reasons, including lack of clinician experience and patient reports of discomfort. Usage of the nasal cannula pressure transducer allows recognition of flow limitation. But guidelines on how to tabulate the amount of flow limitation during total sleep time are lacking. Patients with UARS have significant impairment in their daytime functioning, with reports of sleepiness, fatigue, and sleep disruption. A follow-up study of these patients has shown that they often go untreated and experience progressive worsening of their symptoms. Among those patients who have been treated, typically with CPAP therapy, many have experienced symptomatic improvement. The current fund of knowledge regarding UARS has been growing, and we are beginning to understand the underlying pathophysiology
More on it:
Clinical Features Associated With UARS
Daytime symptoms:
Excessive daytime sleepiness
Fatigue
Morning headaches
Myalgia’s [muscle pain]
Difficulty concentrating
Sleep disturbances:
Frequent nocturnal awakenings
Difficulties initiating sleep
Insomnia
Bruxism [teeth clenching]
Restless leg syndrome
Unrefreshing sleep
Autonomic nervous system:
Hypotension
Orthostasis [maintenance of an upright standing posture]
Cold hands and feet
Functional somatic syndrome associations:
Depression
Anxiety
Chronic fatigue syndrome
Irritable bowel syndrome
Fibromyalgia
Polysomnographic abnormalities Increased RERAs:
Increased nocturnal arousals
Increased CAP rate [cyclical alternating pattern in EEG]
Alpha intrusion during sleep
I have a summary of this medical report that was published in this magazine about UARs in 2011:
http://www.chestnet.org/
You can't access this anymore b/c it now requires a subscription.
A couple of years ago I could access it and even posted here a nice summary.
But in the meantime a competing Sleep Website copied it. So this time I copy it from them:
As you said, not much could be done about treating URS but to continue CAPAing.
The Sleep Doc, Barry Krakow, has UARs himself and recommends a BIPAP machine (BiLevel in Resmed). He uses hi pressure if around 18 cm to treat his URS. That's why he uses a BiPAP which allows him to reduce the pressure for exhalation.
Resmed machines, combine the UARs under Flow Limitations (FL) and provide a graph of it. They measure the level of the FL
by the degree of flattening of the Respiration flow wave curve. FL causes the normal rounded top of the respiration wave curve to flatten and resemble the shape of the letter "r".
I myself have some FL to certain degree which I can follow on my Resmed S9 Autoset machine by using ResScan software.
Here is a recent example:
The following are ResScan graphs of the pressure and events associated with the above:
And these 2 graphs I also check:
IMO, my FL is caused by my stuffy nose. I have Vasomotor Rehinitis which is effected by air flow, and its temperature, from the APAP. This Rehinitis is not an allergy one. My nose gets also stuffy when I touch the cold marble counter top in my kitchen.
So before I mask I blow my nose to get rid of the WHOLE junk. And if it gets stuffy again before I fall asleep I blow it again and again.
Here is the summary that I mentioned above and which I took this time from:
http://www.apneaboard.com/forums/Thread ... e-Syndrome
The top U.S. maven in this field Dr Guilleminault, is lead author.
Upper Airway Resistance Syndrome
Over the past few years, numerous articles have been published that have increased our understanding of the features of upper airway resistance syndrome (UARS). UARS has been previously described as a distinct clinical syndrome, although there is ongoing controversy and some consider it to be part of a spectrum of sleep-disordered breathing that includes primary snoring, obstructive hypopnea syndrome (OHS), and obstructive sleep apnea syndrome (OSAS). However, patients with UARS present with different polysomnographic abnormalities and do not meet generally accepted criteria for either apneas or hypopneas. The lack of education about UARS in the medical community has allowed these patients to go undiagnosed and untreated. Increased research into UARS will help us to identify the optimal treatment for these patients, as well as to educate clinicians about this relatively under-recognized population.
Introduction
UARS is characterized by abnormal respiratory effort, nasal airflow limitation, absence of obstructive sleep apnea, minimal pulse oximetry fluctuation with oxygen saturation nadirs >92%, and frequent nocturnal arousals or reflex brainstem activation. It was first recognized in children in 1982, although the term UARS was not used until the first adult cases were reported in 1993. The incidence and prevalence of UARS has been systematically investigated in a recent São Paulo epidemiologic study (discussed below in "Epidemiologic Studies of UARS"). Prior to the São Paulo study, some have reported prevalence rates of 8% to 20% in the literature.5,6 We now know that this syndrome has recognizable clinical and polysomnographic characteristics that differ from those observed in patients with OHS/OSAS. UARS occurs in all age groups without any clear sex preferences, although some studies suggest that women may be at increased risk. UARS has the potential for significant impact on the daytime functioning and quality of life in untreated patients and there is growing evidence to suggest that symptoms are progressive without treatment.
Treatment
The optimal treatment for patients with UARS is not currently known. Continuous positive airway pressure (CPAP) has been quite useful in the treatment of sleep-disordered breathing and there are some notable positive results in CPAP treatment of UARS. In a study of 15 heavy snorers with clinical evidence of UARS, treatment with nasal CPAP was associated with decreases in observed nocturnal arousals on polysomnography and decreases in mean sleep latency times on multiple sleep latency testing (MSLT) after several nights of treatment.3,36 A follow-up study of 15 subjects (in the original description of UARS) with daytime sleepiness and fatigue and who had undergone a therapeutic trial of positive pressure therapy reported similar findings. After treatment with approximately a month of nasal CPAP, significant improvements were seen in mean sleep latency times on MSLT (5.3 minutes vs 13.5 minutes), Pes nadir pressure (-33.1 cm H2O vs -5.3 cm H2O), amount of slow-wave sleep (1.2% vs 9.7%), and EEG arousals (31.3 vs 7.9 events/hour of sleep). Along with an improvement in sleep latency times on MSLT, there were subjective reports of improved daytime symptoms. Lastly, in a study of 130 postmenopausal women with chronic insomnia and evidence of UARS (n=62) or normal breathing (n=68), treatment with either nasal turbinectomy or nasal CPAP was associated with improvements in subjective reports of sleep quality as measured with a visual analog scale as well as mean sleep latency times on polysomnography. Despite the growing body of evidence supporting the use of positive pressure therapy for UARS patients, it remains difficult to obtain therapy. In a follow-up study of more than 90 patients conducted 4 to 5 years after the initial diagnosis of UARS was made, none of the subjects were receiving CPAP treatment; the main rationale given was that their insurance provider declined to provide the necessary equipment. Formal follow-up clinical evaluations of these patients noted significant worsening in their sleep-related complaints, with increased reports of fatigue, insomnia, and depressive mood. More disturbingly, prescriptions for hypnotics, stimulants, and antidepressants increased more than fivefold.
Other interventions, such as surgery or oral appliances, have also been used with some success in the treatment of patients with UARS. Procedures such as uvulopalatopharyngoplasty, laser-assisted uvuloplasty (LAUP), septoplasty with turbinate reduction, genioglossus advancement, and radiofrequency ablation of the palate have all been described in the literature.37-40 A study of LAUP in nine patients with UARS who underwent uvulopalatopharyngoplasty (n=2), multilevel pharyngeal surgery (n=1), or LAUP (n=6) reported improvements in subjective daytime sleepiness as measured with Epworth Sleepiness Scale scores. In the two patients for whom postoperative polysomnographic data was available, significant improvements in Pes nadir pressures were seen. But patients had several interventions and it is difficult to assess which one was successful. A study of 14 patients with UARS who underwent radiofrequency ablation of the palate also reported improvement in subjective sleepiness, with concurrent improvements in Pes nadir levels and reports of snoring. However, prior reviews of the available literature have noted that many of the studies evaluated small numbers of patients, consisted of uncontrolled case reports or series without clear characterization of the subjects enrolled, and had no consistent end points for an adequate evaluation of efficacy. Further investigation is required to determine the specific role for surgical intervention in these patients. Other authors have also reported successful treatment of UARS with use of oral appliances, although these studies suffer from the same limitations as the surgical literature. In children, orthodontic approaches, such as maxillary distraction or use of expanders, have also shown promising results.
Conclusion
Although UARS has a symptomatology close to the one seen in patients with OSAS, there are distinct clinical differences between the two syndromes. In clinical studies, it is seen more in younger, slim subjects and in premenopausal women; it is more commonly associated with an increase in vagal tone during sleep than with sympathetic hyperactivity (as seen in association with apnea and hypopnea and oxygen desaturation).21 Can individuals with UARS become patients with OSAS? Guilleminault and colleagues suggested that weight increase (with development of a chest-bellow problem related to abdominal obesity) and the association of the supine position and sleep (leading to a restrictive impairment and secondary oxygen saturation drop and sympathetic hyperactivity) will lead to passage from one presentation to another with different complications; but more data are needed from additional systematic, longitudinal studies. UARS is underdiagnosed owing to unfamiliarity with the syndrome and the lack of polysomnographic criteria for either hypopneas or apneas that are associated with other types of sleep-disordered breathing. The advent of use of an esophageal catheter for esophageal pressure measurement (Pes) has allowed clinicians to more clearly identify patients with UARS. Although Pes measurement is the most sensitive method available to detect the abnormal respiratory events in UARS, it has not been used widely for several reasons, including lack of clinician experience and patient reports of discomfort. Usage of the nasal cannula pressure transducer allows recognition of flow limitation. But guidelines on how to tabulate the amount of flow limitation during total sleep time are lacking. Patients with UARS have significant impairment in their daytime functioning, with reports of sleepiness, fatigue, and sleep disruption. A follow-up study of these patients has shown that they often go untreated and experience progressive worsening of their symptoms. Among those patients who have been treated, typically with CPAP therapy, many have experienced symptomatic improvement. The current fund of knowledge regarding UARS has been growing, and we are beginning to understand the underlying pathophysiology
More on it:
Clinical Features Associated With UARS
Daytime symptoms:
Excessive daytime sleepiness
Fatigue
Morning headaches
Myalgia’s [muscle pain]
Difficulty concentrating
Sleep disturbances:
Frequent nocturnal awakenings
Difficulties initiating sleep
Insomnia
Bruxism [teeth clenching]
Restless leg syndrome
Unrefreshing sleep
Autonomic nervous system:
Hypotension
Orthostasis [maintenance of an upright standing posture]
Cold hands and feet
Functional somatic syndrome associations:
Depression
Anxiety
Chronic fatigue syndrome
Irritable bowel syndrome
Fibromyalgia
Polysomnographic abnormalities Increased RERAs:
Increased nocturnal arousals
Increased CAP rate [cyclical alternating pattern in EEG]
Alpha intrusion during sleep
_________________
| Humidifier | ||||
 | ||||
| Additional Comments: CareFusion chinstrap. Quite stiff and not smooth. Not for delicate faces. | ||||
Last edited by penuel on Fri Dec 27, 2013 1:49 pm, edited 1 time in total.
Re: Seeking Upper Airway Resistance Syndrome Success Stories
I believe I had UARS as a child and teenager, which later developed into OSA with centrals (complex sleep apnea). So for me, VPAP controls my sleep apnea and presumably my underlying UARS as well. I also had turbinate reduction surgery which helped.
_________________
| Mask: Simplus Full Face CPAP Mask with Headgear |
| Additional Comments: Resmed VPAP Adapt SV for Complex Sleep Apnea |
Re: Seeking Upper Airway Resistance Syndrome Success Stories
Hi,kkt wrote:I would like to hear from others who are successfully treating UARS -- what methods you used...
When I was losing weight, my OSA became much less of an issue, allowing me to learn that I had UARS hiding behind the OSA. UARS was my primary issue for about a year. The only way I found to deal with it was to experiment with pressure levels. I found that setting pressure based on AHI was great for treating OSA, but I would wake up feeling like a zombie despite having a zero AHI. I had to set the pressure much higher in order to wake up feeling good. That pressure level varied as I lost weight, so I had to tweak it every month or so to find a good pressure. After I lost the bulk of the excess weight, I was able to go back to an auto mode and run based on AHI. However, the UARS fading away seemed to be much correlated with improving upper body strength (doing a lot of exercise) than it was on my weight loss, whereas the OSA seemed to be very much connected to my excess weight.
-john-
Re: Seeking Upper Airway Resistance Syndrome Success Stories
I have UARS. It has been shown with CT scan that I have an extremely small throat, which may explain the chronic fatigue-type events that I have experienced many times in the past.
I don't do well with a CPAP or BiPAP. I tried for 8 months, but get complex apneas, periodic breathing, etc., and feel terrible. Dr. Krakow titrated me on an ASV and I felt much better after a week or so. My health is still really marginal, though. I get painful bouts of aerophagia, and seem to get colds/illness much more now that I sleep with a machine. I suspect I am still having numerous interruptions in my sleep, as the prescription pressure has been set low due to aerophagia pain.
In 2012 I went to Stanford and had a sleep test - I actually managed to tolerate the PES. It took some determination, but I felt the positive diagnosis was necessary before considering surgery.
I don't do well with a CPAP or BiPAP. I tried for 8 months, but get complex apneas, periodic breathing, etc., and feel terrible. Dr. Krakow titrated me on an ASV and I felt much better after a week or so. My health is still really marginal, though. I get painful bouts of aerophagia, and seem to get colds/illness much more now that I sleep with a machine. I suspect I am still having numerous interruptions in my sleep, as the prescription pressure has been set low due to aerophagia pain.
In 2012 I went to Stanford and had a sleep test - I actually managed to tolerate the PES. It took some determination, but I felt the positive diagnosis was necessary before considering surgery.
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: VPAP Adapt SV Bilevel machine, reviewing data with Sleepyhead 9.2-1 |
-
mellabella
- Posts: 326
- Joined: Wed Dec 26, 2007 10:57 am
Re: Seeking Upper Airway Resistance Syndrome Success Stories
BiPap, set at 15/18. Use auto function only for titration nights--the ramping up and down that happens on auto always makes me feel exhausted the morning after. For perspective, I wasted years at 7 and 11 straight CPAP before I switched over--and my AHI isn't much lower but the results have spoken for themselves. I still have a long way to go.
_________________
| Mask: Mirage™ FX Nasal CPAP Mask with Headgear |
| Additional Comments: UARS; pressure 15/19 |
Re: Seeking Upper Airway Resistance Syndrome Success Stories
I was fortunate enough to have my initial sleep study done at a lab that routinely conducts Pes on patients who fit the classical physical profile for UARS. Since I fit the bill, except for being a 60+ yr old male, I had Pes during both my first night diagnostic study and the second night titration study. Pes is not particularly comfortable and I had to have it removed about two thirds of the way through the titration study, but we learned what was needed and I would not be where I am today without it.
The Pes was especially important during the titration study because the Pes indicated that I needed a minimum of 9cm pressure. Running the titration test without the Pes would have resulted in treatment at a lower pressure, which the Pes showed was insufficient to treat my UARS.
I am still in the early stages of aPAP treatment and am still in the stage of fully adjusting to the mask. My first mask caused as many arousals at night as the machine was "fixing" from UARS. My new mask is better, but I am still not quite to where I should be even though I feel better.
As for the other approaches, I have not tried the breathing strips because I had septoplasty a number of years ago and the quick tests indicate the strips provide much more help. As for nasal spray, I occasionally use a saline spray and/or saline rinse during the spring and fall to help supplement my allergy treatments. I have not tried an oral appliance yet, but that might be next.
I should also add that my official diagnosis was "mild OSA" because my insurance company considers all treatments for UARS to be experimental. By being classified as OSA, allowed the xPAP treatment to be covered.
The Pes was especially important during the titration study because the Pes indicated that I needed a minimum of 9cm pressure. Running the titration test without the Pes would have resulted in treatment at a lower pressure, which the Pes showed was insufficient to treat my UARS.
I am still in the early stages of aPAP treatment and am still in the stage of fully adjusting to the mask. My first mask caused as many arousals at night as the machine was "fixing" from UARS. My new mask is better, but I am still not quite to where I should be even though I feel better.
As for the other approaches, I have not tried the breathing strips because I had septoplasty a number of years ago and the quick tests indicate the strips provide much more help. As for nasal spray, I occasionally use a saline spray and/or saline rinse during the spring and fall to help supplement my allergy treatments. I have not tried an oral appliance yet, but that might be next.
I should also add that my official diagnosis was "mild OSA" because my insurance company considers all treatments for UARS to be experimental. By being classified as OSA, allowed the xPAP treatment to be covered.
_________________
| Mask: SleepWeaver Anew™ Full Face Mask with Headgear |
| Additional Comments: Pressure 9-12, Sleepyhead V9.3-0 |
Re: Seeking Upper Airway Resistance Syndrome Success Stories
I have had neck/lung/sinus/congestion issues for many many years, and was only diagnosed/treated for sleep apnea a few years ago. Tried nasal strips, decongestants etc.
It was actually my ophthalmologist who, when discussing dry eyes (dry air, dry house, allergies, cpap blowing air etc. etc.), who recently suggested the following to help with night-time congestion:
1) Get some Allegra-D (has to be this specifically - I am not sure exactly why...was his terminology).
2) Break tablet in half (the package says NOT to break tablet, but the doctor said to specifically break it in two).
3) Take before bed
Been using this for the last week and it has helped greatly....sleeping more deeply, and for at least six to seven hours. Waking up clear headed etc. The last year or so I have been fighting "suffocating" feelings more and more...waking up with my heart racing etc (the usual apnea issues), and I believe it is sinus congestion etc. causing it.
Now I just have to research issues with taking Allegra-D long term....any thoughts?
Grant
It was actually my ophthalmologist who, when discussing dry eyes (dry air, dry house, allergies, cpap blowing air etc. etc.), who recently suggested the following to help with night-time congestion:
1) Get some Allegra-D (has to be this specifically - I am not sure exactly why...was his terminology).
2) Break tablet in half (the package says NOT to break tablet, but the doctor said to specifically break it in two).
3) Take before bed
Been using this for the last week and it has helped greatly....sleeping more deeply, and for at least six to seven hours. Waking up clear headed etc. The last year or so I have been fighting "suffocating" feelings more and more...waking up with my heart racing etc (the usual apnea issues), and I believe it is sinus congestion etc. causing it.
Now I just have to research issues with taking Allegra-D long term....any thoughts?
Grant












