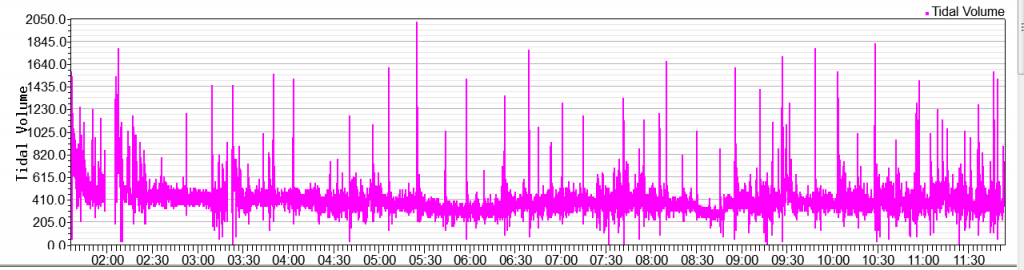
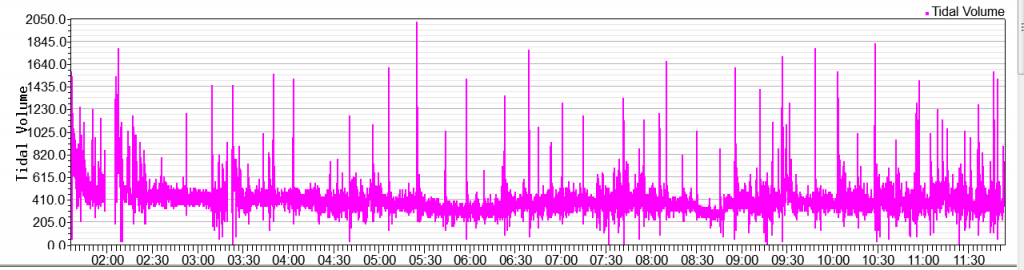
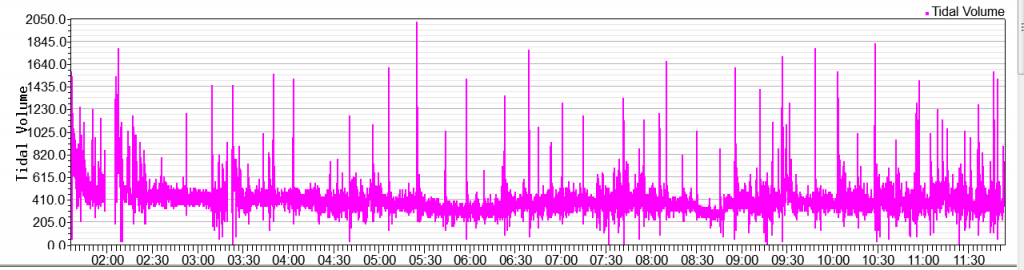
Spikes in Tidal Volume
Spikes in Tidal Volume
Would this be a cause of concern with the spikes?
Re: Spikes in Tidal Volume
There is a phenomenon during sleep called sighing.
The person periodically takes a single deep breath and then exhales followed by resumption of normal breathing pattern.
This is apparently a common phenomenon with no sleep disturbance significance or so my neurologist/sleep specialist thinks. I see it frequently in my waveform data.
The person periodically takes a single deep breath and then exhales followed by resumption of normal breathing pattern.
This is apparently a common phenomenon with no sleep disturbance significance or so my neurologist/sleep specialist thinks. I see it frequently in my waveform data.
_________________
| Mask: Oracle HC452 Oral CPAP Mask |
| Humidifier: DreamStation Heated Humidifier |
| Additional Comments: EverFlo Q 3.0 Liters O2 PR DSX900 ASV |
Oracle 452 Lessons Learned Updated
DSX900 AutoSV with HC150 extra humidifier and Hibernite heated hose
Settings: EPAP Min-10.0, EPAP Max-17, PS Min-3, PS Max-10, Max Pressure-20, Rate-Auto, Biflex-1.
Sleepyhead and Encore Pro 2.21.
DSX900 AutoSV with HC150 extra humidifier and Hibernite heated hose
Settings: EPAP Min-10.0, EPAP Max-17, PS Min-3, PS Max-10, Max Pressure-20, Rate-Auto, Biflex-1.
Sleepyhead and Encore Pro 2.21.
Re: Spikes in Tidal Volume
Is it this phenomena:
Nocturnal moaning and groaning-catathrenia or nocturnal vocalizations
http://www.ncbi.nlm.nih.gov/pubmed/21380609
Nocturnal moaning and groaning-catathrenia or nocturnal vocalizations
http://www.ncbi.nlm.nih.gov/pubmed/21380609
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Re: Spikes in Tidal Volume
Interesting but I don't think so. The "sighing" thing is a single inhale-exhale cycle that, for me, lasts aprox. 4 seconds corresponding to my sleep breathing rate of 15 BPM.
_________________
| Mask: Oracle HC452 Oral CPAP Mask |
| Humidifier: DreamStation Heated Humidifier |
| Additional Comments: EverFlo Q 3.0 Liters O2 PR DSX900 ASV |
Oracle 452 Lessons Learned Updated
DSX900 AutoSV with HC150 extra humidifier and Hibernite heated hose
Settings: EPAP Min-10.0, EPAP Max-17, PS Min-3, PS Max-10, Max Pressure-20, Rate-Auto, Biflex-1.
Sleepyhead and Encore Pro 2.21.
DSX900 AutoSV with HC150 extra humidifier and Hibernite heated hose
Settings: EPAP Min-10.0, EPAP Max-17, PS Min-3, PS Max-10, Max Pressure-20, Rate-Auto, Biflex-1.
Sleepyhead and Encore Pro 2.21.
Re: Spikes in Tidal Volume
James, I see a similar graph of Tidal Volume spiking with this James (age 36!):

Source:
http://www.apneasupport.org/post191044.html?style=2
Also, CSR:


Source:
http://www.apneasupport.org/post191044.html?style=2
Also, CSR:

_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Re: Spikes in Tidal Volume
IMO, the treatment for the Tidal Volume Hyper Ventilation (spikes) is in additional O(2) supply.
Reference:
CONCLUSION:
The data demonstrate that using a titration protocol with CPAP and then PAP with O(2) effectively eliminates CSA in individuals with underlying comorbid conditions and prescription opioid use. Comparative studies with other therapeutic modalities are required.
http://www.ncbi.nlm.nih.gov/pubmed/23066368
Reference:
CONCLUSION:
The data demonstrate that using a titration protocol with CPAP and then PAP with O(2) effectively eliminates CSA in individuals with underlying comorbid conditions and prescription opioid use. Comparative studies with other therapeutic modalities are required.
http://www.ncbi.nlm.nih.gov/pubmed/23066368
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Re: Spikes in Tidal Volume
avi123
So you saying that having a large number of spikes is the body trying to get enough 0² and keeps resetting the blood CO² levels? I read that hyperventilation is not the best way to increase o² levels as normal steady breathing?
So you saying that having a large number of spikes is the body trying to get enough 0² and keeps resetting the blood CO² levels? I read that hyperventilation is not the best way to increase o² levels as normal steady breathing?
Re: Spikes in Tidal Volume
avi123:avi123 wrote:IMO, the treatment for the Tidal Volume Hyper Ventilation (spikes) is in additional O(2) supply.
Reference:
CONCLUSION:
The data demonstrate that using a titration protocol with CPAP and then PAP with O(2) effectively eliminates CSA in individuals with underlying comorbid conditions and prescription opioid use. Comparative studies with other therapeutic modalities are required.
http://www.ncbi.nlm.nih.gov/pubmed/23066368
I seemed to miss something in the referenced article. It seems to be discussing people with CSA and with comorbid conditions and doesn't seem to have anything to do with tidal volume spikes in respirations.
O(2) supplementation may very well help with the tidal volume spikes but this article doesn't indicate such a connection.
_________________
| Mask: Oracle HC452 Oral CPAP Mask |
| Humidifier: DreamStation Heated Humidifier |
| Additional Comments: EverFlo Q 3.0 Liters O2 PR DSX900 ASV |
Oracle 452 Lessons Learned Updated
DSX900 AutoSV with HC150 extra humidifier and Hibernite heated hose
Settings: EPAP Min-10.0, EPAP Max-17, PS Min-3, PS Max-10, Max Pressure-20, Rate-Auto, Biflex-1.
Sleepyhead and Encore Pro 2.21.
DSX900 AutoSV with HC150 extra humidifier and Hibernite heated hose
Settings: EPAP Min-10.0, EPAP Max-17, PS Min-3, PS Max-10, Max Pressure-20, Rate-Auto, Biflex-1.
Sleepyhead and Encore Pro 2.21.
Re: Spikes in Tidal Volume
I know that some spikes are normal but if you get many of them at 4 to 5 times the normal rate I think that the body is trying to tell me something. Sighing as one poster mention is more of a emotional or anxiety response when you are in deep sleep? Not sure that is really the case here. I am going to see my new sleep doctor this week.
Re: Spikes in Tidal Volume
James and John, I am relating to the two modalities to treat the hyperventilations (spikes in the Tidal Volume graph) that are mentioned in my above links to reports, in this thread:
1) "Either positive pressure therapy (PAP) or supplemental oxygen (O(2)) may stabilize respiration in CSA by reducing ventilatory chemoresponsiveness",
Treatment of central sleep apnea in U.S. veterans.
Chowdhuri S, Ghabsha A, Sinha P, Kadri M, Narula S, Badr MS.
and
2) Treatment of positive airway pressure treatment-associated respiratory instability with enhanced expiratory rebreathing space (EERS).
Treatment of positive airway pressure treatment-associated respiratory instability with enhanced expiratory rebreathing space (EERS).
Gilmartin G, McGeehan B, Vigneault K, Daly RW, Manento M, Weiss JW, Thomas RJ.
1) "Either positive pressure therapy (PAP) or supplemental oxygen (O(2)) may stabilize respiration in CSA by reducing ventilatory chemoresponsiveness",
Treatment of central sleep apnea in U.S. veterans.
Chowdhuri S, Ghabsha A, Sinha P, Kadri M, Narula S, Badr MS.
and
2) Treatment of positive airway pressure treatment-associated respiratory instability with enhanced expiratory rebreathing space (EERS).
Treatment of positive airway pressure treatment-associated respiratory instability with enhanced expiratory rebreathing space (EERS).
Gilmartin G, McGeehan B, Vigneault K, Daly RW, Manento M, Weiss JW, Thomas RJ.
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Re: Spikes in Tidal Volume
AVI123
The first study says to add supplemental O² may help stabilize respiration
The second says to add CO² re-breathing may help with respiratory instability.
While I am not a medical expert it seems that the two studies statements contradict with each other, in other words does not make much sense to me.
The first study says to add supplemental O² may help stabilize respiration
The second says to add CO² re-breathing may help with respiratory instability.
While I am not a medical expert it seems that the two studies statements contradict with each other, in other words does not make much sense to me.
Re: Spikes in Tidal Volume
John yes, they are the opposite but we need to find which one is the needed one, or possibly both.
Check this:
http://www.normalbreathing.com/CO2-breath-control.php
Breath control in the sick: increased role of O2
Older man breathing oxygen Control of breathing of sick people is done, in addition to CO2, by current blood O2 concentrations. The urge for oxygen gets stronger with the advance of many diseases.
The control of the breathing of sick people is accomplished by blood and brain CO2 concentrations and O2 drive, which becomes stronger with progression of chronic diseases and increasing cell hypoxia due to increased respiration (elevated minute ventilation).
In severely sick people, O2 can become the main factor in regulation of respiration.
The change in air composition during human evolution and evolution of animals on the Earth was the key factor that led to appearance of chronic diseases. This is because hyperventilation was beneficial for creatures living in primitive air with very low O2 content and high CO2 content 1-2 millions of years ago, but overbreathing destroys health now.
Also:
Pathophysiology of Central Sleep Apnea
http://emedicine.medscape.com/article/3 ... view#a0104
Check this:
http://www.normalbreathing.com/CO2-breath-control.php
Breath control in the sick: increased role of O2
Older man breathing oxygen Control of breathing of sick people is done, in addition to CO2, by current blood O2 concentrations. The urge for oxygen gets stronger with the advance of many diseases.
The control of the breathing of sick people is accomplished by blood and brain CO2 concentrations and O2 drive, which becomes stronger with progression of chronic diseases and increasing cell hypoxia due to increased respiration (elevated minute ventilation).
In severely sick people, O2 can become the main factor in regulation of respiration.
The change in air composition during human evolution and evolution of animals on the Earth was the key factor that led to appearance of chronic diseases. This is because hyperventilation was beneficial for creatures living in primitive air with very low O2 content and high CO2 content 1-2 millions of years ago, but overbreathing destroys health now.
Also:
Pathophysiology of Central Sleep Apnea
http://emedicine.medscape.com/article/3 ... view#a0104
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Re: Spikes in Tidal Volume
One group posits that as the blood moves toward a hypocapnic state it tends to hyper-sensitize the peripheral chemoreceptors. In other words blowing off too much CO2 causes the resultant blood chemistry to make the carotid bodies more sensitive to deoxygenated blood cells and so produces a larger breathing signal than is appropriate for the current metabolism levels.john5757 wrote:AVI123
The first study says to add supplemental O² may help stabilize respiration
The second says to add CO² re-breathing may help with respiratory instability.
While I am not a medical expert it seems that the two studies statements contradict with each other, in other words does not make much sense to me.
The larger breathing signal then further reduces the blood CO2 levels which reduces the flow of blood to the brain and separates the central from peripheral chemoreceptors. The control of breathing therefore becomes very unstable.
Well now, if you add O2 to the incoming air then the proposed hyper-sensitized state of the peripheral chemoreceptors would have much less effect. That is, it takes less breathing to satisfy what the chemoreceptors would be happy with. Say they normally want to see “no more than 4% deoxygenated blood cells in the blood on the way to the brain” (sensing at the carotid bodies). Then they become hyper-sensitized and so want to see “no more than 2% deoxygenated blood cells in the blood on the way to the brain”. If you are using supplemental O2 you can meet that criteria with a lot less breathing. Less breathing results in better CO2 maintenance.
Perhaps the peripheral chemoreceptors become hyper-sensitive due to excessive central nervous system activity or stress hormone levels. Whatever the source supplemental O2 would quiet things down.
Supplemental O2 seems to initially work to stabilize breathing but seems to become less effective over time. I have found the re-breathing approach is consistently effective. That said, I use it only as necessary (2-3 months a year).
May any shills trolls sockpuppets or astroturfers at cpaptalk.com be like chaff before the wind!
Re: Spikes in Tidal Volume
You're getting colder...
Re: Spikes in Tidal Volume
I think it would also be good to add that adding supplemental O2 or CO2 (re-breathing or otherwise) are steps likely to have side effects. Today I will be spending some quality time with my machine during the day to help breathing reflexes with the machine while breathing quietly become more established in my reflexes. I will also be doing some aerobic steps and may well do some 85% of maximum heart rate work to help my breathing reflexes in general. I will also do some meditation and prayer.Todzo wrote:One group posits that as the blood moves toward a hypocapnic state it tends to hyper-sensitize the peripheral chemoreceptors. In other words blowing off too much CO2 causes the resultant blood chemistry to make the carotid bodies more sensitive to deoxygenated blood cells and so produces a larger breathing signal than is appropriate for the current metabolism levels.john5757 wrote:AVI123
The first study says to add supplemental O² may help stabilize respiration
The second says to add CO² re-breathing may help with respiratory instability.
While I am not a medical expert it seems that the two studies statements contradict with each other, in other words does not make much sense to me.
The larger breathing signal then further reduces the blood CO2 levels which reduces the flow of blood to the brain and separates the central from peripheral chemoreceptors. The control of breathing therefore becomes very unstable.
Well now, if you add O2 to the incoming air then the proposed hyper-sensitized state of the peripheral chemoreceptors would have much less effect. That is, it takes less breathing to satisfy what the chemoreceptors would be happy with. Say they normally want to see “no more than 4% deoxygenated blood cells in the blood on the way to the brain” (sensing at the carotid bodies). Then they become hyper-sensitized and so want to see “no more than 2% deoxygenated blood cells in the blood on the way to the brain”. If you are using supplemental O2 you can meet that criteria with a lot less breathing. Less breathing results in better CO2 maintenance.
Perhaps the peripheral chemoreceptors become hyper-sensitive due to excessive central nervous system activity or stress hormone levels. Whatever the source supplemental O2 would quiet things down.
Supplemental O2 seems to initially work to stabilize breathing but seems to become less effective over time. I have found the re-breathing approach is consistently effective. That said, I use it only as necessary (2-3 months a year).
I think that there are many things we can do to add to our health that do not involve pharmaceuticals or mechanical splints and that we should concentrate on those things.
May any shills trolls sockpuppets or astroturfers at cpaptalk.com be like chaff before the wind!