patrissimo wrote: But statistically, this means that any evidence we have on, say, the performance of ASV vs. CPAP on one population applies 50% to the other. If ASV is twice as good as CPAP at reducing the OAI in ComplexSAS, we would expect it to be 1.5x as good on OSA. That is basic statistics. Of course, if we tested it, it probably wouldn't turn out to be 1.5x as good, because the two treatments likely wouldn't be exactly equal at the 50% of events that are unique to plain OSA. But the most accurate guess we can make using that information is 1.5x - that ASV will do twice as well on the half of events that are the same, and that the two will perform equally well on the events that are different (that's our best guess when we have no other information about relative performance on this sample).
You never presented a shred of evidence for commonality. Rather you worked on a vague and under-researched supposition of commonality as established fact. Sleep researchers have yet to agree on commonality, if any, in the pathogenesis for these two populations.[/quote]
I don't see why I need to prove commonality between the two populations when they are so similar. Sure, the opioid-induced SDB population may be totally different. But the ComplexSAS population? They started out the same as the OSA population, and the two split based on whether their obstructive apneas could be treated by a level of pressure that didn't introduce centrals. I am baffled that you could think that makes the two populations 100% different. Or even 50% different!
We start out with 100 people with OSA, and we crank up their CPAP pressure. 80 of them find a pressure that brings their AHI < 1, and causes no centrals. The other 20 of them develop CPAP-induced central sleep apnea, and are moved to ASV machines, which bring their AHI < 1. It seems you are saying that the obstructive apneas that come up during the night for the first 80 people have a completely different pathogenesis than the obstructive apneas that come up for the second 20 people.
That just seems really implausible to me. I'm not saying that the pathogenesis is 100% identical, I totally buy that there are differences between the populations, and differences between the obstructive events that they experience, but how can you claim it is 100% different and has no similarity? There are only so many mechanisms for pathogenesis, it seems really implausible that the separation procedure that I just outlined would neatly divide the 100 people into 80 people with only pathogenesis types A, B, and C, and 20 people with only types X, Y, and Z. Doesn't it?
patrissimo wrote: In order for ASV vs. CPAP performance on obstructive apneas in ComplexSAS to tell us *absolutely nothing* about ASV vs. CPAP performance on obstructive apneas in OSA, it would have to be the case, not merely that they are somewhat different, not merely that the populations aren't identical, but that there was absolutely no similarity. If there is any overlap in pathogenesis between the events in the two populations, then we can statistically infer that a treatment that is better on one is, before testing, more likely than not to be better on the other.
Your scope of statistical analysis also fails to factor iatrogenic effects of unnecessary PS.[/quote]
Yes, definitely. I was only directly addressing the question of whether we can extrapolate from the performance of ASV vs. CPAP on obstructive apneas in the ComplexSAS population to an expected performance difference on the OSA population. My reason for doing that was to extrapolate an expected performance difference on not just apneas, but hypnopneas, and not just hypnopneas, but flow limitations of all sorts. And my reason for doing that was to make guesses about which would best relieve EDS in a person with SDB. As the inferences get increasingly remote from the original data, more and more other factors come into play. Perhaps one lowers the AHI through a treatment that also narrows the glottis by adduction of the vocal cords, decreasing the effective ventilation that reaches the lungs, and worsening sleep fragmentation and EDS. I am open to other metrics and other treatments.
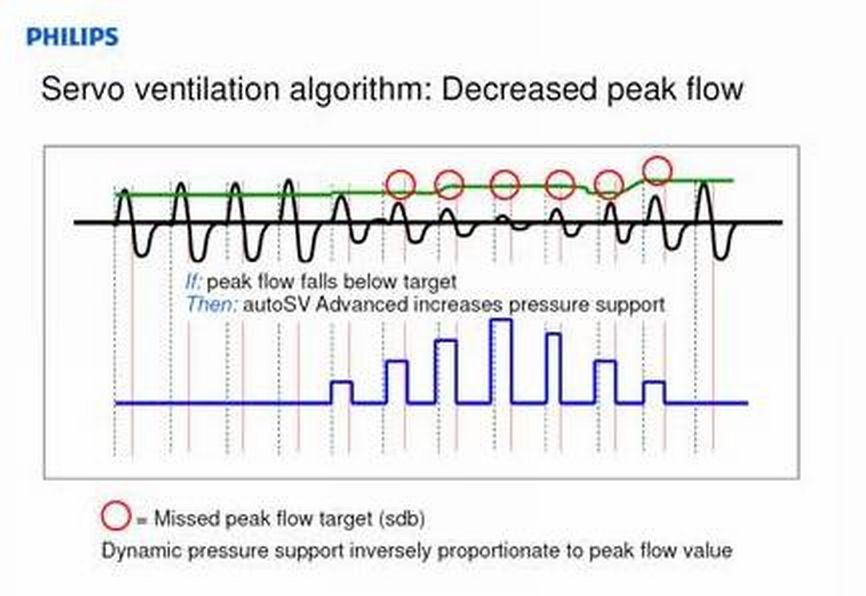
But wouldn't an ASV tend to have less unnecessary PS, due to the split-second response, then something like fixed CPAP or BiPAP which you have to set high enough to splint the airway during all sleep stages?