Disabling fatigue--have you ever been this down?
Disabling fatigue--have you ever been this down?
Hi:
Has anyone gotten to the point where you simply couldn't function?
For many years I started many days believing I couldn't function, but could still drag myself through the day. Recently though, things have taken a scary turn for the ultimate worst. I literally cannot hold my eyes open for much of the day, or remain vertical for more than 10-15 minutes without needing to lie down. My mind is going blank for significant stretches of time, when in the past I was the kind of hyper-analytical person that would earn remarks of "you think too much." I have constant pain in my eye sockets. Even the most trivial technical challenges of my profession are too mentally demanding for me to even look at.
I finally decided Thursday to tell my boss that I would come in "as able," an outcome I have been struggling desperately for months to avoid. I've tried Nuvigil, which worked for a few months, and now only makes me feel like I should have energy, but I still can't keep my eyes open. I'll leave the story of my caffeine escapade for another post. Suffice it to say, that if I took a single dose of caff. right now of 5x the amount that worked the first time 8 months ago, it would probably work, for about 2-3 hours. But then the next 2 days afterward would be even worse. Surely such a habit is not sustainable which is why I've discontinued using caffeine.
The only thing saving me right now from maddening despair is that after 16 years of working off a faulty negative diagnosis for OSA, I now know that I have it and am eagerly awaiting to begin CPAP treatment in just a few more days.
I am quite worried though, that things might actually get worse before they get better. But I feel like I am near rock bottom, so what does "worse" actually mean? My mind cannot fathom it. Since my condition now is basically unable to work without using a drug (with only marginal benefit) or unable to work at all, I dread the thought of having this persist or worsen for any length of time.
I sure hope things improve, even if just a little bit, fairly quickly.
Has anyone reached, and then recovered from completely disabling fatigue?
Thanks for input.
Has anyone gotten to the point where you simply couldn't function?
For many years I started many days believing I couldn't function, but could still drag myself through the day. Recently though, things have taken a scary turn for the ultimate worst. I literally cannot hold my eyes open for much of the day, or remain vertical for more than 10-15 minutes without needing to lie down. My mind is going blank for significant stretches of time, when in the past I was the kind of hyper-analytical person that would earn remarks of "you think too much." I have constant pain in my eye sockets. Even the most trivial technical challenges of my profession are too mentally demanding for me to even look at.
I finally decided Thursday to tell my boss that I would come in "as able," an outcome I have been struggling desperately for months to avoid. I've tried Nuvigil, which worked for a few months, and now only makes me feel like I should have energy, but I still can't keep my eyes open. I'll leave the story of my caffeine escapade for another post. Suffice it to say, that if I took a single dose of caff. right now of 5x the amount that worked the first time 8 months ago, it would probably work, for about 2-3 hours. But then the next 2 days afterward would be even worse. Surely such a habit is not sustainable which is why I've discontinued using caffeine.
The only thing saving me right now from maddening despair is that after 16 years of working off a faulty negative diagnosis for OSA, I now know that I have it and am eagerly awaiting to begin CPAP treatment in just a few more days.
I am quite worried though, that things might actually get worse before they get better. But I feel like I am near rock bottom, so what does "worse" actually mean? My mind cannot fathom it. Since my condition now is basically unable to work without using a drug (with only marginal benefit) or unable to work at all, I dread the thought of having this persist or worsen for any length of time.
I sure hope things improve, even if just a little bit, fairly quickly.
Has anyone reached, and then recovered from completely disabling fatigue?
Thanks for input.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Software: Sleepyhead v0.9.2-1 |
__________
Good day!
Good day!
Re: Disabling fatigue--have you ever been this down?
most people with OSA who've had it for a long time before treatment know the feeling quite well!
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Actually a S9 VPAP Adapt, and Respironics M Series Auto BiPAP |
- MaxDarkside
- Posts: 1199
- Joined: Sun Dec 18, 2011 4:21 pm
- Location: Minneapolis, MN
Re: Disabling fatigue--have you ever been this down?
Yes, me. I was having TIA like symptoms, being lost, disoriented, was totally work-non-functional, I was in quite bad shape and was functionally going STRAIGHT DOWN just before I got my APAP machine. I got it in the NICK OF TIME !! I own a very high tech analytics software and services company, CTO ("you think too much" person too), and my work was suffering terribly, I could not concentrate AT ALL and I had some big projects coming that I had to PERFORM outstandingly. THEN...AHI15 wrote:Has anyone gotten to the point where you simply couldn't function?
I got my ResMed S9 AutoSet and started the road to recovery. It's taken some months of step by step improvement, the "TIA" part never reoccurred, my heart arrhythmias started to fade, my concentration abilities rose again, bit by bit over 9 months. I'm not where I once was, but I'm getting older too.
You mention a high EBV antibody count in an earlier post (I looked ). There are numerous of those anti-bodies and you might talk to your doctors about which ones because the combination of them tell a story, like you are presently battling, or maybe they say you merely were at one time. If you add sleep apnea on top of such a current malady, I can imagine you would be very much like you say you are, I mean by that what you are describing could be about right. You also mentioned "flow limitation not included in AHI but disrupting sleep was noted in 85% of total sleep time.". That'll also put a torpedo into the side of your cognitive and daytime alertness.
So, I think you have treatment (a machine) coming, yes? Consider it a life saving device, no whining about compliance. Consider it a MUST DO. Next, I'd talk to the doc about those antibodies, which ones, in what proportion and if he does not know what that means, then maybe find a EBV top-notch doc who can give you the all clear (was in past, is not now) or help with that.
My 2 cents. You get what you pay for (zero cents)
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: CMS-50E Oximeter, Zeo Bedside, Software: Comm'l grade AI analytics server & tools & SleepyHead |
Do or Die... Sleep Apnea killed me, but I came back. Click for my story
Please visit my My Apnea Analytics blog. Maybe we can help each other.
54 yrs, 6' 1", 160->172 lbs
Please visit my My Apnea Analytics blog. Maybe we can help each other.
54 yrs, 6' 1", 160->172 lbs
- MaxDarkside
- Posts: 1199
- Joined: Sun Dec 18, 2011 4:21 pm
- Location: Minneapolis, MN
Re: Disabling fatigue--have you ever been this down?
AHI 15,
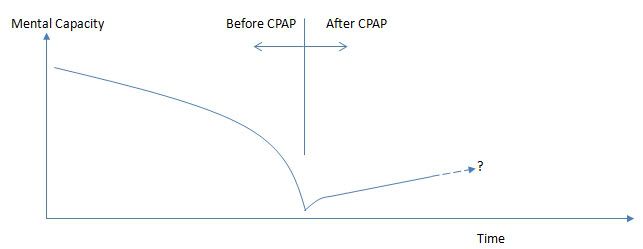
Since you know what a tuning eye is, you know what a non-linear function is and what happens when that's non-linear DOWNWARD. Below is a graphic I made of what I've experienced.
In the beginning OSA causes a slow degradation of abilities, fairly linear, the body is a very adaptive compensating system, but the effect accumulates over time and also can cause brain damage. Your de-sats I think you said were in the low 90's, not too bad, so that's good. Mine were into the 70's and thus not so good. Over time I got worse faster and from just before getting the sleep study ordered, then the study, then the diagnosis, then the prescription then getting the machine, some 3 months I think, I had reached the part of the curve where I was degenerating RAPIDLY downward. Once I got treatment, things reversed, not as good as before yet, but still climbing, as I show in the diagram. Where I end up, I don't know, but I am WAY better than what I was before, still some daytime grog, but there are times I do return to "cognitive brilliance" briefly, when I'm "in the flow state". Before APAP, forget any flippin' "flow state". I was a vegetable ready to be planted 6 feet under.
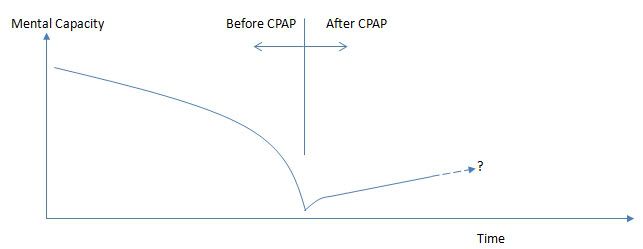
Since you know what a tuning eye is, you know what a non-linear function is and what happens when that's non-linear DOWNWARD. Below is a graphic I made of what I've experienced.
In the beginning OSA causes a slow degradation of abilities, fairly linear, the body is a very adaptive compensating system, but the effect accumulates over time and also can cause brain damage. Your de-sats I think you said were in the low 90's, not too bad, so that's good. Mine were into the 70's and thus not so good. Over time I got worse faster and from just before getting the sleep study ordered, then the study, then the diagnosis, then the prescription then getting the machine, some 3 months I think, I had reached the part of the curve where I was degenerating RAPIDLY downward. Once I got treatment, things reversed, not as good as before yet, but still climbing, as I show in the diagram. Where I end up, I don't know, but I am WAY better than what I was before, still some daytime grog, but there are times I do return to "cognitive brilliance" briefly, when I'm "in the flow state". Before APAP, forget any flippin' "flow state". I was a vegetable ready to be planted 6 feet under.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: CMS-50E Oximeter, Zeo Bedside, Software: Comm'l grade AI analytics server & tools & SleepyHead |
Do or Die... Sleep Apnea killed me, but I came back. Click for my story
Please visit my My Apnea Analytics blog. Maybe we can help each other.
54 yrs, 6' 1", 160->172 lbs
Please visit my My Apnea Analytics blog. Maybe we can help each other.
54 yrs, 6' 1", 160->172 lbs
- Sir NoddinOff
- Posts: 4189
- Joined: Mon May 14, 2012 5:30 pm
- Location: California
Re: Disabling fatigue--have you ever been this down?
I know things look bleak but remember that we are all here for you. You can lay your weary head down with the members watching over you... rest... then find a new way.
_________________
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Additional Comments: Sleepyhead software v.0.9.8.1 Open GL and Encore Pro v2.2. |
I like my ResMed AirFit F10 FFM - reasonably low leaks for my ASV therapy. I'm currently using a PR S1 AutoSV 960P Advanced. I also keep a ResMed S9 Adapt as backup. I use a heated Hibernite hose. Still rockin' with Win 7 by using GWX to stop Win 10.
Re: Disabling fatigue--have you ever been this down?
Yes, but add in some car accidents, broken bones too. Things get better with cpap.
_________________
| Mask: SleepWeaver Elan™ Soft Cloth Nasal CPAP Mask - Starter Kit |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: It's not about how many breaths you take; it's about the moments that take your breath away! |
Re: Disabling fatigue--have you ever been this down?
Yes, there was a time when I felt much like you describe. I was dealing with limb movements in addition to OSA, but therapeutically treating my sleep apnea was the beginning of me feeling as if I was heading away from the grave rather than toward it. Once you get your equipment consider yourself in recovery and get plenty of rest and take very good care of yourself nutritionally to give your body what it needs to begin to heal. Everybody's speed and degree of recovery is different, as the extent of damage varies, but it's very realistic to expect improvement, and who knows, maybe you'll be even better than you dared dream.
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: Disabling fatigue--have you ever been this down?
hi AHI15 ~
My mom (catnapper) pointed out your post to me and asked me if i might respond.
some of what you are describing sounds like myalgic encephalomeylitis (ME), as it's known through most of the world. In the US, it's more commonly referred to as "Chronic Fatigue Syndrome" -a poorly understood and wildly underfunded illness that affects an estimated million people in the US, 17 million world-wide. It is possible to have a diagnosis of ME co-morbid with OSA, though *untreated* OSA is considered an exclusionary diagnosis. Someone referred to you having high EBV titres, and the re-activation or chronic appearance of the ubiquitous herpes-viruses (HHV-6, cytomegalovirus, EBV, etc.) can be associated with the immune dysfunction commonly observed in ME. Having severe untreated OSA can be very hard on one's immune system, along with the overall systemic stress.
first of all, the sign (a symptom that is specific to a given illness) for ME is "post exertional neurological exhaustion" - (PENE) - which means that when you do things that were in the past trivial for you, and which didn't cause problems, now those same activities cause relapse or intensification of other symptoms (cognitive problems, pain, weakness, flu-like symptoms, dizziness, nausea, among others).
I would suggest that you read the ICC (International Consensus Criteria) and decide whether your symptoms fit with the description. The relevant part is just a few pages long. (I'll copy a link to the full article, as well as excerpting the criteria.) You may have to start and progress with your OSA treatment before you can really get help with the ME diagnosis. It's possible, though, given the symptoms you describe, that you could be doing significant damage to your system by pushing through. Please consider asking your employer for temporary medical leave. If you are at a large enough company, you should be eligible for FMLA without danger to your job. My doctor put me on orders not to work more than 10 hours per week, in 5 hours or less per day, with no field work, and primarily working from home, for the first 6 months. Because I had pushed so hard (like you, trying to retain function and fulfill my responsibilities), my condition continued to deteriorate for those 6 months, and eventually I became totally disabled. Please be careful and try to seriously curtail your activities and get as much rest as you can. I know it feels really impossible to do that, but it's important to try to salvage your health.
you're welcome to pm me if you want.
best regards,
Bast
links and excerpt below:
from this article: http://onlinelibrary.wiley.com/doi/10.1 ... 428.x/full
Here are the diagnostic criteria:
The Canadian Consensus Criteria were used as a starting point, but significant changes were made. The 6-month waiting period before diagnosis is no longer required. No other disease criteria require that diagnoses be withheld until after the patient has suffered with the affliction for 6 months. Notwithstanding periods of clinical investigation will vary and may be prolonged, diagnosis should be made when the clinician is satisfied that the patient has ME rather than having the diagnosis restricted by a specified time factor. Early diagnoses may elicit new insights into the early stages of pathogenesis; prompt treatment may lessen the severity and impact.
Using ‘fatigue’ as a name of a disease gives it exclusive emphasis and has been the most confusing and misused criterion. No other fatiguing disease has ‘chronic fatigue’ attached to its name – e.g. cancer/chronic fatigue, multiple sclerosis/chronic fatigue – except ME/CFS. Fatigue in other conditions is usually proportional to effort or duration with a quick recovery and will recur to the same extent with the same effort or duration that same or next day. The pathological low threshold of fatigability of ME described in the following criteria often occurs with minimal physical or mental exertion and with reduced ability to undertake the same activity within the same or several days.
The International Consensus Criteria (Table 1) identify the unique and distinctive characteristic patterns of symptom clusters of ME. The broad spectrum of symptoms alerts medical practitioners to areas of pathology and may identify critical symptoms more accurately [18–20]. Operational notes following each criterion provide guidance in symptom expression and contextual interpretation. This will assist the primary clinician in identifying and treating patients with ME in the primary care setting.
Table 1. Myalgic encephalomyelitis: international consensus criteriaAdult and paediatric ● clinical and research
Myalgic encephalomyelitis is an acquired neurological disease with complex global dysfunctions. Pathological dysregulation of the nervous, immune and endocrine systems, with impaired cellular energy metabolism and ion transport are prominent features. Although signs and symptoms are dynamically interactive and causally connected, the criteria are grouped by regions of pathophysiology to provide general focus.
A patient will meet the criteria for postexertional neuroimmune exhaustion (A), at least one symptom from three neurological impairment categories (B), at least one symptom from three immune/gastro-intestinal/genitourinary impairment categories (C), and at least one symptom from energy metabolism/transport impairments (D).
A. Postexertional neuroimmune exhaustion (PENE pen’-e): Compulsory
This cardinal feature is a pathological inability to produce sufficient energy on demand with prominent symptoms primarily in the neuroimmune regions. Characteristics are as follows:
1. Marked, rapid physical and/or cognitive fatigability in response to exertion, which may be minimal such as activities of daily living or simple mental tasks, can be debilitating and cause a relapse.
2. Postexertional symptom exacerbation:e.g.acute flu-like symptoms, pain and worsening of other symptoms.
3. Postexertional exhaustion may occur immediately after activity or be delayed by hours or days.
4. Recovery period is prolonged, usually taking 24 h or longer. A relapse can last days, weeks or longer.
5. Low threshold of physical and mental fatigability (lack of stamina) results in a substantial reduction in pre-illness activity level.
Operational notes:For a diagnosis of ME, symptom severity must result in a significant reduction of a patient’s premorbid activity level.Mild(an approximate 50% reduction in pre-illness activity level),moderate(mostly housebound),severe(mostly bedridden) orvery severe(totally bedridden and need help with basic functions). There may be marked fluctuation of symptom severity and hierarchy from day to day or hour to hour. Consider activity, context and interactive effects.Recovery time: e.g. Regardless of a patient’s recovery time from reading for ½ hour, it will take much longer to recover from grocery shopping for ½ hour and even longer if repeated the next day – if able. Those who rest before an activity or have adjusted their activity level to their limited energy may have shorter recovery periods than those who do not pace their activities adequately.Impact: e.g. An outstanding athlete could have a 50% reduction in his/her pre-illness activity level and is still more active than a sedentary person.
B. Neurological impairments
At least one symptom from three of the following four symptom categories
1. Neurocognitive impairments
a. Difficulty processing information: slowed thought, impaired concentration e.g. confusion, disorientation, cognitive overload, difficulty with making decisions, slowed speech, acquired or exertional dyslexia
b. Short-term memory loss:e.g. difficulty remembering what one wanted to say, what one was saying, retrieving words, recalling information, poor working memory
2. Pain
a. Headaches:e.g. chronic, generalized headaches often involve aching of the eyes, behind the eyes or back of the head that may be associated with cervical muscle tension; migraine; tension headaches
b. Significant pain can be experienced in muscles, muscle-tendon junctions, joints, abdomen or chest. It is noninflammatory in nature and often migrates. e.g. generalized hyperalgesia, widespread pain (may meet fibromyalgia criteria), myofascial or radiating pain
3. Sleep disturbance
a. Disturbed sleep patterns:e.g. insomnia, prolonged sleep including naps, sleeping most of the day and being awake most of the night, frequent awakenings, awaking much earlier than before illness onset, vivid dreams/nightmares
b. Unrefreshed sleep:e.g. awaken feeling exhausted regardless of duration of sleep, day-time sleepiness
4. Neurosensory, perceptual and motor disturbances
a. Neurosensory and perceptual:e.g. inability to focus vision, sensitivity to light, noise, vibration, odour, taste and touch; impaired depth perception
b. Motor:e.g. muscle weakness, twitching, poor coordination, feeling unsteady on feet, ataxia
Notes: Neurocognitive impairments, reported or observed, become more pronounced with fatigue.Overload phenomenamay be evident when two tasks are performed simultaneously. Abnormal accommodation responsesof the pupils are common.Sleep disturbancesare typically expressed by prolonged sleep, sometimes extreme, in the acute phase and often evolve into marked sleep reversal in the chronic stage.Motor disturbancesmay not be evident in mild or moderate cases but abnormal tandem gait and positive Romberg test may be observed in severe cases.
C. Immune, gastro-intestinal and genitourinary Impairments
At least one symptom from three of the following five symptom categories
1. Flu-like symptoms may be recurrent or chronic and typically activate or worsen with exertion.e.g. sore throat, sinusitis, cervical and/or axillary lymph nodes may enlarge or be tender on palpitation
2. Susceptibility to viral infections with prolonged recovery periods
3. Gastro-intestinal tract:e.g. nausea, abdominal pain, bloating, irritable bowel syndrome
4. Genitourinary: e.g. urinary urgency or frequency, nocturia
5. Sensitivities to food, medications, odours or chemicals
Notes:Sore throat, tender lymph nodes, and flu-like symptoms obviously are not specific to ME but their activation in reaction to exertion is abnormal. The throat may feel sore, dry and scratchy. Faucial injection and crimson crescents may be seen in the tonsillar fossae, which are an indication of immune activation.
D. Energy production/transportation impairments: At least one symptom
1. Cardiovascular:e.g. inability to tolerate an upright position - orthostatic intolerance, neurally mediated hypotension, postural orthostatic tachycardia syndrome, palpitations with or without cardiac arrhythmias, light-headedness/dizziness
2. Respiratory:e.g. air hunger, laboured breathing, fatigue of chest wall muscles
3. Loss of thermostatic stability:e.g. subnormal body temperature, marked diurnal fluctuations; sweating episodes, recurrent feelings of feverishness with or without low grade fever, cold extremities
4. Intolerance of extremes of temperature
Notes:Orthostatic intolerance may be delayed by several minutes. Patients who have orthostatic intolerance may exhibit mottling of extremities, extreme pallor or Raynaud’s Phenomenon. In the chronic phase, moons of finger nails may recede.
Paediatric considerations
Symptoms may progress more slowly in children than in teenagers or adults. In addition to postexertional neuroimmune exhaustion, the most prominent symptoms tend to be neurological: headaches, cognitive impairments, and sleep disturbances.
1. Headaches: Severe or chronic headaches are often debilitating. Migraine may be accompanied by a rapid drop in temperature, shaking, vomiting, diarrhoea and severe weakness.
2. Neurocognitive impairments: Difficulty focusing eyes and reading are common. Children may become dyslexic, which may only be evident when fatigued. Slow processing of information makes it difficult to follow auditory instructions or take notes. All cognitive impairments worsen with physical or mental exertion. Young people will not be able to maintain a full school programme.
3. Pain may seem erratic and migrate quickly. Joint hypermobility is common.
Notes:Fluctuation and severity hierarchy of numerous prominent symptoms tend to vary more rapidly and dramatically than in adults.
Classification
——— Myalgic encephalomyelitis
——— Atypical myalgic encephalomyelitis: meets criteria for postexertional neuroimmune exhaustion but has a limit of two less than required of the remaining criterial symptoms. Pain or sleep disturbance may be absent in rare cases.
Exclusions:As in all diagnoses, exclusion of alternate explanatory diagnoses is achieved by the patient’s history, physical examination, and laboratory/biomarker testing as indicated. It is possible to have more than one disease but it is important that each one is identified and treated.Primary psychiatric disorders, somatoform disorder and substance abuse are excluded. Paediatric:‘primary’ school phobia.
Comorbid entities: Fibromyalgia, myofascial pain syndrome, temporomandibular joint syndrome, irritable bowel syndrome, interstitial cystitis, Raynaud’s phenomenon, prolapsed mitral valve, migraines, allergies, multiple chemical sensitivities, Hashimoto’s thyroiditis, Sicca syndrome, reactive depression. Migraine and irritable bowel syndrome may precede ME but then become associated with it. Fibromyalgia overlaps.
~^+~~*~*~*~*~*~*~*~*~*~*~*~*~*~*~*
My mom (catnapper) pointed out your post to me and asked me if i might respond.
some of what you are describing sounds like myalgic encephalomeylitis (ME), as it's known through most of the world. In the US, it's more commonly referred to as "Chronic Fatigue Syndrome" -a poorly understood and wildly underfunded illness that affects an estimated million people in the US, 17 million world-wide. It is possible to have a diagnosis of ME co-morbid with OSA, though *untreated* OSA is considered an exclusionary diagnosis. Someone referred to you having high EBV titres, and the re-activation or chronic appearance of the ubiquitous herpes-viruses (HHV-6, cytomegalovirus, EBV, etc.) can be associated with the immune dysfunction commonly observed in ME. Having severe untreated OSA can be very hard on one's immune system, along with the overall systemic stress.
first of all, the sign (a symptom that is specific to a given illness) for ME is "post exertional neurological exhaustion" - (PENE) - which means that when you do things that were in the past trivial for you, and which didn't cause problems, now those same activities cause relapse or intensification of other symptoms (cognitive problems, pain, weakness, flu-like symptoms, dizziness, nausea, among others).
I would suggest that you read the ICC (International Consensus Criteria) and decide whether your symptoms fit with the description. The relevant part is just a few pages long. (I'll copy a link to the full article, as well as excerpting the criteria.) You may have to start and progress with your OSA treatment before you can really get help with the ME diagnosis. It's possible, though, given the symptoms you describe, that you could be doing significant damage to your system by pushing through. Please consider asking your employer for temporary medical leave. If you are at a large enough company, you should be eligible for FMLA without danger to your job. My doctor put me on orders not to work more than 10 hours per week, in 5 hours or less per day, with no field work, and primarily working from home, for the first 6 months. Because I had pushed so hard (like you, trying to retain function and fulfill my responsibilities), my condition continued to deteriorate for those 6 months, and eventually I became totally disabled. Please be careful and try to seriously curtail your activities and get as much rest as you can. I know it feels really impossible to do that, but it's important to try to salvage your health.
you're welcome to pm me if you want.
best regards,
Bast
links and excerpt below:
from this article: http://onlinelibrary.wiley.com/doi/10.1 ... 428.x/full
Here are the diagnostic criteria:
The Canadian Consensus Criteria were used as a starting point, but significant changes were made. The 6-month waiting period before diagnosis is no longer required. No other disease criteria require that diagnoses be withheld until after the patient has suffered with the affliction for 6 months. Notwithstanding periods of clinical investigation will vary and may be prolonged, diagnosis should be made when the clinician is satisfied that the patient has ME rather than having the diagnosis restricted by a specified time factor. Early diagnoses may elicit new insights into the early stages of pathogenesis; prompt treatment may lessen the severity and impact.
Using ‘fatigue’ as a name of a disease gives it exclusive emphasis and has been the most confusing and misused criterion. No other fatiguing disease has ‘chronic fatigue’ attached to its name – e.g. cancer/chronic fatigue, multiple sclerosis/chronic fatigue – except ME/CFS. Fatigue in other conditions is usually proportional to effort or duration with a quick recovery and will recur to the same extent with the same effort or duration that same or next day. The pathological low threshold of fatigability of ME described in the following criteria often occurs with minimal physical or mental exertion and with reduced ability to undertake the same activity within the same or several days.
The International Consensus Criteria (Table 1) identify the unique and distinctive characteristic patterns of symptom clusters of ME. The broad spectrum of symptoms alerts medical practitioners to areas of pathology and may identify critical symptoms more accurately [18–20]. Operational notes following each criterion provide guidance in symptom expression and contextual interpretation. This will assist the primary clinician in identifying and treating patients with ME in the primary care setting.
Table 1. Myalgic encephalomyelitis: international consensus criteriaAdult and paediatric ● clinical and research
Myalgic encephalomyelitis is an acquired neurological disease with complex global dysfunctions. Pathological dysregulation of the nervous, immune and endocrine systems, with impaired cellular energy metabolism and ion transport are prominent features. Although signs and symptoms are dynamically interactive and causally connected, the criteria are grouped by regions of pathophysiology to provide general focus.
A patient will meet the criteria for postexertional neuroimmune exhaustion (A), at least one symptom from three neurological impairment categories (B), at least one symptom from three immune/gastro-intestinal/genitourinary impairment categories (C), and at least one symptom from energy metabolism/transport impairments (D).
A. Postexertional neuroimmune exhaustion (PENE pen’-e): Compulsory
This cardinal feature is a pathological inability to produce sufficient energy on demand with prominent symptoms primarily in the neuroimmune regions. Characteristics are as follows:
1. Marked, rapid physical and/or cognitive fatigability in response to exertion, which may be minimal such as activities of daily living or simple mental tasks, can be debilitating and cause a relapse.
2. Postexertional symptom exacerbation:e.g.acute flu-like symptoms, pain and worsening of other symptoms.
3. Postexertional exhaustion may occur immediately after activity or be delayed by hours or days.
4. Recovery period is prolonged, usually taking 24 h or longer. A relapse can last days, weeks or longer.
5. Low threshold of physical and mental fatigability (lack of stamina) results in a substantial reduction in pre-illness activity level.
Operational notes:For a diagnosis of ME, symptom severity must result in a significant reduction of a patient’s premorbid activity level.Mild(an approximate 50% reduction in pre-illness activity level),moderate(mostly housebound),severe(mostly bedridden) orvery severe(totally bedridden and need help with basic functions). There may be marked fluctuation of symptom severity and hierarchy from day to day or hour to hour. Consider activity, context and interactive effects.Recovery time: e.g. Regardless of a patient’s recovery time from reading for ½ hour, it will take much longer to recover from grocery shopping for ½ hour and even longer if repeated the next day – if able. Those who rest before an activity or have adjusted their activity level to their limited energy may have shorter recovery periods than those who do not pace their activities adequately.Impact: e.g. An outstanding athlete could have a 50% reduction in his/her pre-illness activity level and is still more active than a sedentary person.
B. Neurological impairments
At least one symptom from three of the following four symptom categories
1. Neurocognitive impairments
a. Difficulty processing information: slowed thought, impaired concentration e.g. confusion, disorientation, cognitive overload, difficulty with making decisions, slowed speech, acquired or exertional dyslexia
b. Short-term memory loss:e.g. difficulty remembering what one wanted to say, what one was saying, retrieving words, recalling information, poor working memory
2. Pain
a. Headaches:e.g. chronic, generalized headaches often involve aching of the eyes, behind the eyes or back of the head that may be associated with cervical muscle tension; migraine; tension headaches
b. Significant pain can be experienced in muscles, muscle-tendon junctions, joints, abdomen or chest. It is noninflammatory in nature and often migrates. e.g. generalized hyperalgesia, widespread pain (may meet fibromyalgia criteria), myofascial or radiating pain
3. Sleep disturbance
a. Disturbed sleep patterns:e.g. insomnia, prolonged sleep including naps, sleeping most of the day and being awake most of the night, frequent awakenings, awaking much earlier than before illness onset, vivid dreams/nightmares
b. Unrefreshed sleep:e.g. awaken feeling exhausted regardless of duration of sleep, day-time sleepiness
4. Neurosensory, perceptual and motor disturbances
a. Neurosensory and perceptual:e.g. inability to focus vision, sensitivity to light, noise, vibration, odour, taste and touch; impaired depth perception
b. Motor:e.g. muscle weakness, twitching, poor coordination, feeling unsteady on feet, ataxia
Notes: Neurocognitive impairments, reported or observed, become more pronounced with fatigue.Overload phenomenamay be evident when two tasks are performed simultaneously. Abnormal accommodation responsesof the pupils are common.Sleep disturbancesare typically expressed by prolonged sleep, sometimes extreme, in the acute phase and often evolve into marked sleep reversal in the chronic stage.Motor disturbancesmay not be evident in mild or moderate cases but abnormal tandem gait and positive Romberg test may be observed in severe cases.
C. Immune, gastro-intestinal and genitourinary Impairments
At least one symptom from three of the following five symptom categories
1. Flu-like symptoms may be recurrent or chronic and typically activate or worsen with exertion.e.g. sore throat, sinusitis, cervical and/or axillary lymph nodes may enlarge or be tender on palpitation
2. Susceptibility to viral infections with prolonged recovery periods
3. Gastro-intestinal tract:e.g. nausea, abdominal pain, bloating, irritable bowel syndrome
4. Genitourinary: e.g. urinary urgency or frequency, nocturia
5. Sensitivities to food, medications, odours or chemicals
Notes:Sore throat, tender lymph nodes, and flu-like symptoms obviously are not specific to ME but their activation in reaction to exertion is abnormal. The throat may feel sore, dry and scratchy. Faucial injection and crimson crescents may be seen in the tonsillar fossae, which are an indication of immune activation.
D. Energy production/transportation impairments: At least one symptom
1. Cardiovascular:e.g. inability to tolerate an upright position - orthostatic intolerance, neurally mediated hypotension, postural orthostatic tachycardia syndrome, palpitations with or without cardiac arrhythmias, light-headedness/dizziness
2. Respiratory:e.g. air hunger, laboured breathing, fatigue of chest wall muscles
3. Loss of thermostatic stability:e.g. subnormal body temperature, marked diurnal fluctuations; sweating episodes, recurrent feelings of feverishness with or without low grade fever, cold extremities
4. Intolerance of extremes of temperature
Notes:Orthostatic intolerance may be delayed by several minutes. Patients who have orthostatic intolerance may exhibit mottling of extremities, extreme pallor or Raynaud’s Phenomenon. In the chronic phase, moons of finger nails may recede.
Paediatric considerations
Symptoms may progress more slowly in children than in teenagers or adults. In addition to postexertional neuroimmune exhaustion, the most prominent symptoms tend to be neurological: headaches, cognitive impairments, and sleep disturbances.
1. Headaches: Severe or chronic headaches are often debilitating. Migraine may be accompanied by a rapid drop in temperature, shaking, vomiting, diarrhoea and severe weakness.
2. Neurocognitive impairments: Difficulty focusing eyes and reading are common. Children may become dyslexic, which may only be evident when fatigued. Slow processing of information makes it difficult to follow auditory instructions or take notes. All cognitive impairments worsen with physical or mental exertion. Young people will not be able to maintain a full school programme.
3. Pain may seem erratic and migrate quickly. Joint hypermobility is common.
Notes:Fluctuation and severity hierarchy of numerous prominent symptoms tend to vary more rapidly and dramatically than in adults.
Classification
——— Myalgic encephalomyelitis
——— Atypical myalgic encephalomyelitis: meets criteria for postexertional neuroimmune exhaustion but has a limit of two less than required of the remaining criterial symptoms. Pain or sleep disturbance may be absent in rare cases.
Exclusions:As in all diagnoses, exclusion of alternate explanatory diagnoses is achieved by the patient’s history, physical examination, and laboratory/biomarker testing as indicated. It is possible to have more than one disease but it is important that each one is identified and treated.Primary psychiatric disorders, somatoform disorder and substance abuse are excluded. Paediatric:‘primary’ school phobia.
Comorbid entities: Fibromyalgia, myofascial pain syndrome, temporomandibular joint syndrome, irritable bowel syndrome, interstitial cystitis, Raynaud’s phenomenon, prolapsed mitral valve, migraines, allergies, multiple chemical sensitivities, Hashimoto’s thyroiditis, Sicca syndrome, reactive depression. Migraine and irritable bowel syndrome may precede ME but then become associated with it. Fibromyalgia overlaps.
~^+~~*~*~*~*~*~*~*~*~*~*~*~*~*~*~*
BreathFirst! No compromise in defense of high SA02!
Re: Disabling fatigue--have you ever been this down?
Hi - I don't want to rain on your parade Bast, but I believe it's dangerous (or at least confusing) to ask an already very tired person to match his symptoms to a list on the internet and decide if he has Chronic Fatigue or anything else... The symptoms are somewhat vague in many instances to begin with and can easily be cited in many other illnesses besides CFS. He needs to get tested for apnea and see what the results show, and for anything else, to see a doctor, if necessary a different one or ones, and not play the internet game... it's driving many people to think they have many problems - and very often the important symptoms or signs (signs are what doctors see that we don't necessarily appreciate) are missed entirely because they're not on the list or are simply not felt, seen or interpreted properly... do we all really know what the normal variants are for every symptom we think we have? Normal variants are the ranges of 'normal' for individual symptoms vs what's actually abnormal enough (depending on the patient, their other medical history and other parameters such as age, etc. etc.) to worry about.
And it's also important to understand the relative 'weight' of individual signs or symptoms to each other in different circumstances and patients, something we cannot possibly figure out on our own without lots of training or education.
And it's also important to understand the relative 'weight' of individual signs or symptoms to each other in different circumstances and patients, something we cannot possibly figure out on our own without lots of training or education.
Re: Disabling fatigue--have you ever been this down?
"rain on my parade" ?
i wasn't having a parade, Julie.
i did not say AHI15 should diagnose himself/herself with the illness. i think it's reasonable to give information. your mileage may vary.
people who have ME have enough trouble dealing with inconsistencies and outright ignorance in the medical community. I was offering a piece of information that could be very helpful. if AHI15 thinks none of it fits, then that's GREAT news.
i wasn't having a parade, Julie.
i did not say AHI15 should diagnose himself/herself with the illness. i think it's reasonable to give information. your mileage may vary.
people who have ME have enough trouble dealing with inconsistencies and outright ignorance in the medical community. I was offering a piece of information that could be very helpful. if AHI15 thinks none of it fits, then that's GREAT news.
BreathFirst! No compromise in defense of high SA02!
Re: Disabling fatigue--have you ever been this down?
I know your intentions were great, but it was maybe not such a great idea otherwise...
Btw 'raining on a parade' is a saying, I wasn't saying you were having a parade.
Btw 'raining on a parade' is a saying, I wasn't saying you were having a parade.
Re: Disabling fatigue--have you ever been this down?
I asked bast to reply to the original poster because he wanted to know if anyone had ever experienced his kind of fatigue. What he described reminded me of the devastating fatigue that people who have ME/CFS experience. Bast has studied this mysterious illness and I thought she could better answer his question than I could.
Peoople with OSA experience fatigue, but not to the extent and depth that sufferers of ME do. I have no intention of discounting what OSA does to someone, both with fatigue and other health consequences. I have experienced the fatigue of OSA myself for years before and even after diagnosis and successful treatment. I know how others with OSA suffer from reading cpaptalk for 6 years. Added to his fatigue was the EBS possibility which could also indicate ME/CFS. Everyone feels fatigued from time to time. Treating OSA successfully will not change the impact of ME.
AHI15 asked a question, bast answered with her knowledge and experience. He can take from it what he chooses or is able to do.
Catnapper - Joanie
Peoople with OSA experience fatigue, but not to the extent and depth that sufferers of ME do. I have no intention of discounting what OSA does to someone, both with fatigue and other health consequences. I have experienced the fatigue of OSA myself for years before and even after diagnosis and successful treatment. I know how others with OSA suffer from reading cpaptalk for 6 years. Added to his fatigue was the EBS possibility which could also indicate ME/CFS. Everyone feels fatigued from time to time. Treating OSA successfully will not change the impact of ME.
AHI15 asked a question, bast answered with her knowledge and experience. He can take from it what he chooses or is able to do.
Catnapper - Joanie
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
Last edited by Catnapper on Sun Jul 29, 2012 11:07 am, edited 1 time in total.
Re: Disabling fatigue--have you ever been this down?
Julie ~ yeah, i know "rain on your parade" is a saying, but your use of it implies that i was putting on a show of some sort that you were "raining on"- or that you were extinguishing some delight of mine - neither of those were applicable. might be good to be more careful with your use of cliches.
i get that you don't think it was a good idea for me to post the best overall criteria for a little-known illness based on AHI15 describing something that sounds very much like ME, a condition with which many, many doctors are unfamiliar, and most certainly don't know the recently-published ICC criteria. i didn't send some random blog post ranting about ME - I sent a peer-reviewed journal article with the collective perspective of numerous doctors who've been studying this illness for years.
your response makes me angry, actually. you seem so smug in your assertion that doctors know so much more than we possibly could, and that we need to give our power to them in terms of understanding what's going on. most of us know our bodies much better than any doctor ever could.
I sincerely hope AHI15 doesn't have ME. However, if it's the case, it's absolutely imperative to stop pushing. pushing in the recovery state of post-exertional-exaustion or relapse causes damage, as shown by test-retest exercise research. That was the only piece of advice i gave - to try to protect one's health by resting when one is too exhausted to move. Oh, i also suggested that FMLA might be appropriate - that's just basic Human Resources info.
If AHI15 is using information off the internet, that's his choice, not yours.
besides, what's up with you, on an internet forum, suggesting people NOT use the internet to get information?
you say AHI15 needs to have a sleep study - but given the nickname and presence on this forum, i'm guessing he/she already has. people like you are the reason i don't bother much with this forum anymore. instead of taking things in context, people are so ready to criticize others.
It was not "good intentions" that brought me to make my post - it was noticing a description that's unusually similar to the experience I have observed and heard about from others for years.
to AHI15, I apologize if my post offended you or overwhelmed you in any way. I hope you find answers to your health concerns, and that you have the support you need to regain your health and well-being.
i get that you don't think it was a good idea for me to post the best overall criteria for a little-known illness based on AHI15 describing something that sounds very much like ME, a condition with which many, many doctors are unfamiliar, and most certainly don't know the recently-published ICC criteria. i didn't send some random blog post ranting about ME - I sent a peer-reviewed journal article with the collective perspective of numerous doctors who've been studying this illness for years.
your response makes me angry, actually. you seem so smug in your assertion that doctors know so much more than we possibly could, and that we need to give our power to them in terms of understanding what's going on. most of us know our bodies much better than any doctor ever could.
I sincerely hope AHI15 doesn't have ME. However, if it's the case, it's absolutely imperative to stop pushing. pushing in the recovery state of post-exertional-exaustion or relapse causes damage, as shown by test-retest exercise research. That was the only piece of advice i gave - to try to protect one's health by resting when one is too exhausted to move. Oh, i also suggested that FMLA might be appropriate - that's just basic Human Resources info.
If AHI15 is using information off the internet, that's his choice, not yours.
besides, what's up with you, on an internet forum, suggesting people NOT use the internet to get information?
you say AHI15 needs to have a sleep study - but given the nickname and presence on this forum, i'm guessing he/she already has. people like you are the reason i don't bother much with this forum anymore. instead of taking things in context, people are so ready to criticize others.
It was not "good intentions" that brought me to make my post - it was noticing a description that's unusually similar to the experience I have observed and heard about from others for years.
to AHI15, I apologize if my post offended you or overwhelmed you in any way. I hope you find answers to your health concerns, and that you have the support you need to regain your health and well-being.
BreathFirst! No compromise in defense of high SA02!
Re: Disabling fatigue--have you ever been this down?
Well I have been that down, that's for sure.
I work in a mentally draining job (constant analyzing/problem solving while sitting in a cube in front of a computer all day long) I am here now because I reached the end of the road to my not being able to function. It was just getting worse.
My sleep doctor wanted to do a test for narcolepsy on me but the insurance will not approve that until there is some history with cpap treatment. I could not tolerate a cpap (constant pressure) and this when I learned about bipaps and asked for one (yep, I had to ask. no one suggested it) Honestly, my feeling, and this is just my feeling, is that because I was not compliant, I was deemed "not trying'. Since in my geographical area, drs are on overload with drg low reimbursment, there is a certain amt of piecework to make the numbers(ok, this alludes to back in the day factory workers got paid by the piece.) In a low reimbursement area (determined by insurance/government) thanks to 'the system" it is becoming about quantity and not quality.Swell
MY question, can this begin to skirt near a disability qualification? I already have been on fmla for 3 years when nuvigil and will power will not keep me upright in my chair at work.(and there is a limit to how nuvigil I am willing to pump into my body to be able to perform because I am knowledgable about addiction) It is what it is.
I know one wants to be careful about blanket statements, but I have watched my progression downward closely and I do begin to think we are just touching the tip of knowledge to what this apnea harms in us. mentally I am not what I was. Physically, I am lucky to work. Life after work is minimal. Even on the bipap. I have been tired too long and I think damage has been done. Can it repair? I don't know. Does anyone know,really?
I work in a mentally draining job (constant analyzing/problem solving while sitting in a cube in front of a computer all day long) I am here now because I reached the end of the road to my not being able to function. It was just getting worse.
My sleep doctor wanted to do a test for narcolepsy on me but the insurance will not approve that until there is some history with cpap treatment. I could not tolerate a cpap (constant pressure) and this when I learned about bipaps and asked for one (yep, I had to ask. no one suggested it) Honestly, my feeling, and this is just my feeling, is that because I was not compliant, I was deemed "not trying'. Since in my geographical area, drs are on overload with drg low reimbursment, there is a certain amt of piecework to make the numbers(ok, this alludes to back in the day factory workers got paid by the piece.) In a low reimbursement area (determined by insurance/government) thanks to 'the system" it is becoming about quantity and not quality.Swell
MY question, can this begin to skirt near a disability qualification? I already have been on fmla for 3 years when nuvigil and will power will not keep me upright in my chair at work.(and there is a limit to how nuvigil I am willing to pump into my body to be able to perform because I am knowledgable about addiction) It is what it is.
I know one wants to be careful about blanket statements, but I have watched my progression downward closely and I do begin to think we are just touching the tip of knowledge to what this apnea harms in us. mentally I am not what I was. Physically, I am lucky to work. Life after work is minimal. Even on the bipap. I have been tired too long and I think damage has been done. Can it repair? I don't know. Does anyone know,really?
_________________
| Mask: AirFit™ N20 Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleepyhead for Mac s9 auto settings 11-16 |
Re: Disabling fatigue--have you ever been this down?
Good luck AHI. I hope your CPAP works miracles, they often do. A few comments, though.
1) Even if you do have apnea, don't neglect the possibility that you have some other health problems. It sounds trite, but patients AND doctors tend to get tunnel vision.
2) A minority of people feel even more tired when starting CPAP. Work through it, it's worth it.
3) Commit to working through the problems with CPAP. Ask for help here.
4) I think you've been through the process of getting a good CPAP machine.
1) Even if you do have apnea, don't neglect the possibility that you have some other health problems. It sounds trite, but patients AND doctors tend to get tunnel vision.
2) A minority of people feel even more tired when starting CPAP. Work through it, it's worth it.
3) Commit to working through the problems with CPAP. Ask for help here.
4) I think you've been through the process of getting a good CPAP machine.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Also SleepyHead, PRS1 Auto, Respironics Auto M series, Legacy Auto, and Legacy Plus |
Please enter your equipment in your profile so we can help you.
Click here for information on the most common alternative to CPAP.
If it's midnight and a DME tells you it's dark outside, go and check for yourself.
Useful Links.
Click here for information on the most common alternative to CPAP.
If it's midnight and a DME tells you it's dark outside, go and check for yourself.
Useful Links.