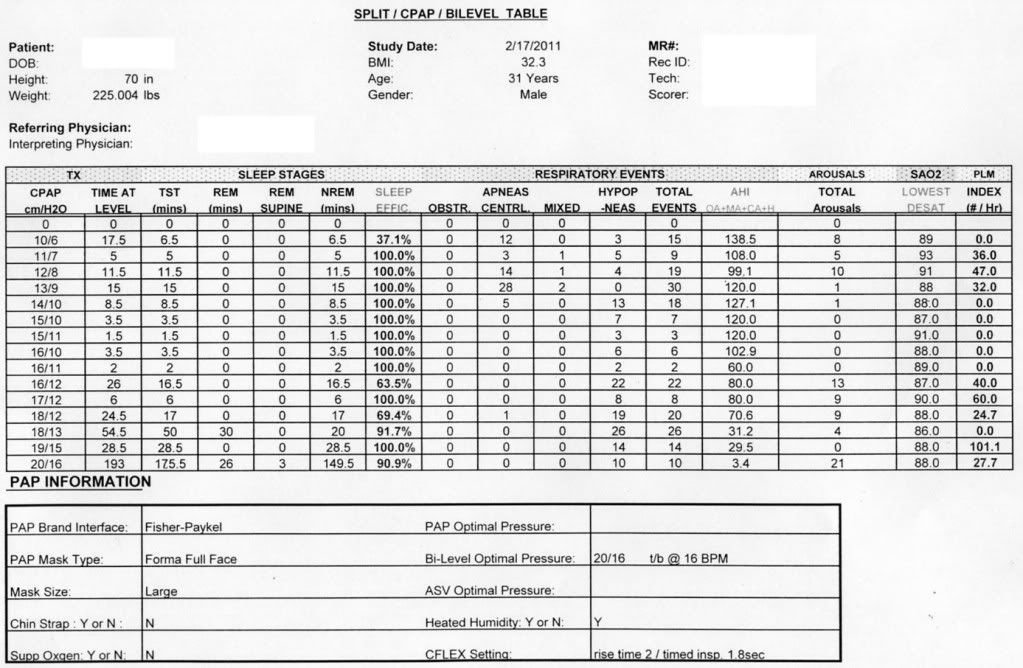
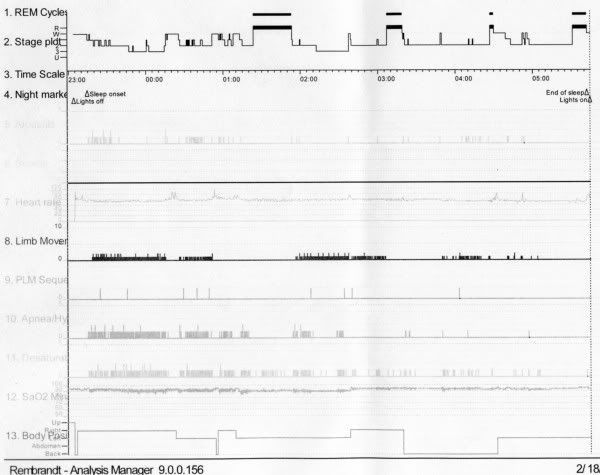
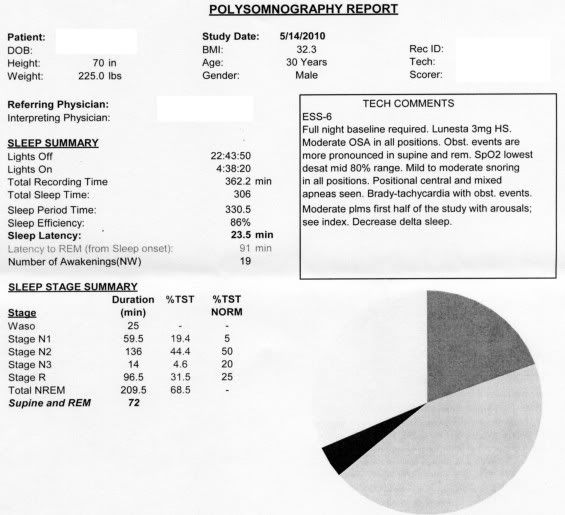
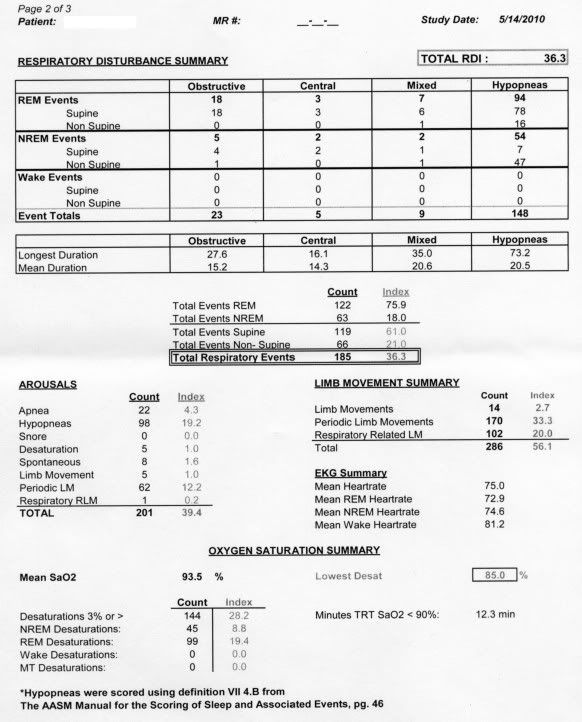
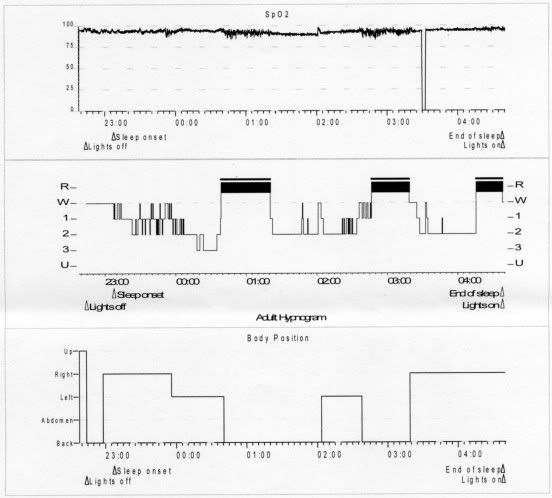
To summarize the past 13 months into a single paragraph: The diagnostic study was conducted in May of last year. Over 306 minutes, it revealed 148 hypopneas, 23 obstructive apneas, 5 central apneas, and 9 mixed apneas. The diagnosis was "moderate obstructive sleep apnea" and "moderate PLMD." CPAP titration a month later yielded a prescribed pressure of 13 cm/H2O. At home, the CPAP led to periodic breathing, many central apneas, and exhaustion, so I had a BiPAP S/T titration in February. The home experience here was even worse (extreme daytime sleepiness plus AHI in the mid 30s, comprised mostly of hypopneas), which led to my ASV titration in May. In contrast to what the CPAP and BiPAP titrations suggested, a very low EPAP on my ASV seems to address almost all obstructive apneas. However, I still don't feel great and I have residual hypopneas (nightly HI average is 8, but nights range from 4 to 18) which so far occur regardless of IPAP.
Generally speaking, I'm interested in what you all make of the two reports below. What stands out to you? Are there any areas of concern I should ask my docs about specifically? Most important, are there insights for what might make my ASV work better for me?
I also have some specific questions.
• I've read that mixed apneas are usually assumed to be predominantly obstructive in nature. Is this correct? If the answer is "it depends," what can we infer about my case?
• While I had significant treatment-emergent central apneas on the CPAP and at lower pressures on the BiPAP S/T, which I believe would be classified as traditional complex sleep apnea, does that have any bearing on the relatively few central apneas that appeared in my diagnostic? Or can we still generally write those off as mostly insignificant?
• As you can see from the diagnostic PSG results, hypopneas were dominant. Over at the binarysleep boards, the technicians have discussed how some of their labs attempt to classify hypopneas as obstructive or central, whereas others do not. Can we shed any light on the source of my hypopneas and the proper course of action to address them? Does it even matter? I know the general rule of thumb is that increasing IPAP addresses hypopneas and flow limitations, but so far my hyopneas exist even when IPAP approaches 20.
• What about the Brady-tachycardia that was observed? From what I've read it seems to be somewhat common in OSA patients, but I'm way out of my league here.
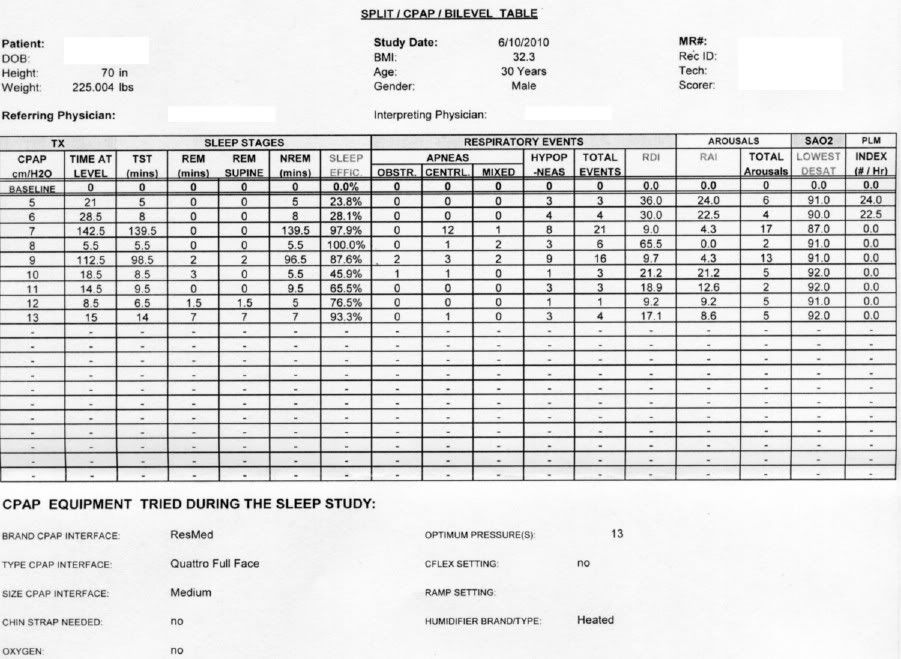
• In the CPAP titration, at least to my untrained eye, it looks like I never stabilized. What am I missing that led them to settle on a pressure of 13 and send me on my merry way with that?
• I've gathered that chasing apnea and PLMD can be a little bit of a chicken-and-egg exercise. Does seeing this data make anything stick out to you?
Thanks in advance.
DIAGNOSTIC PSG
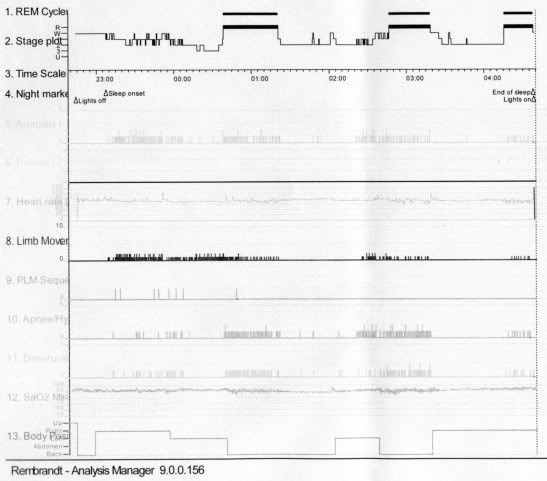
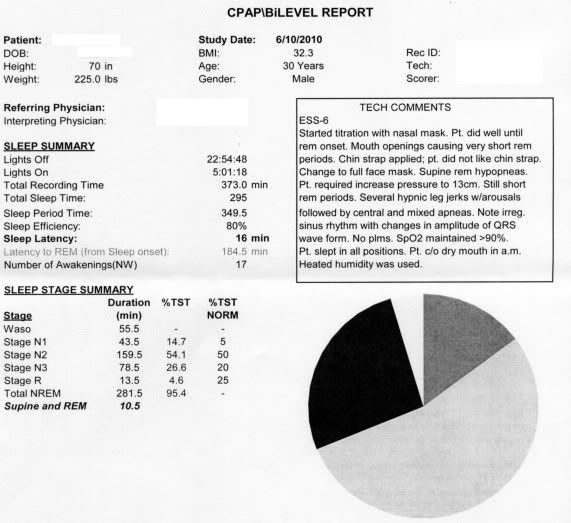
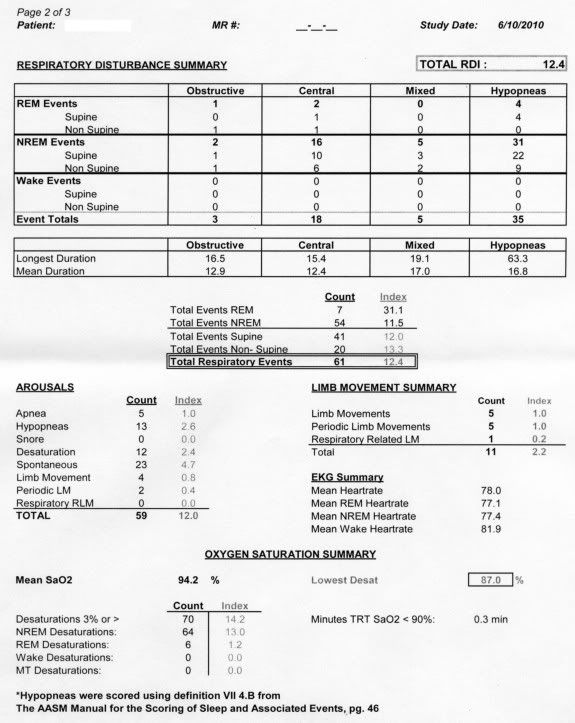
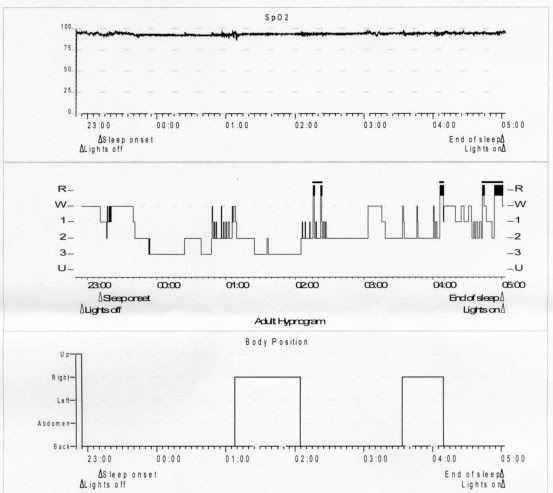
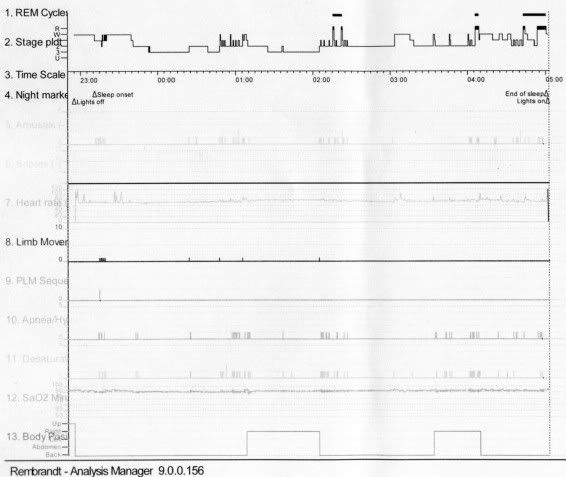
CPAP TITRATION PSG
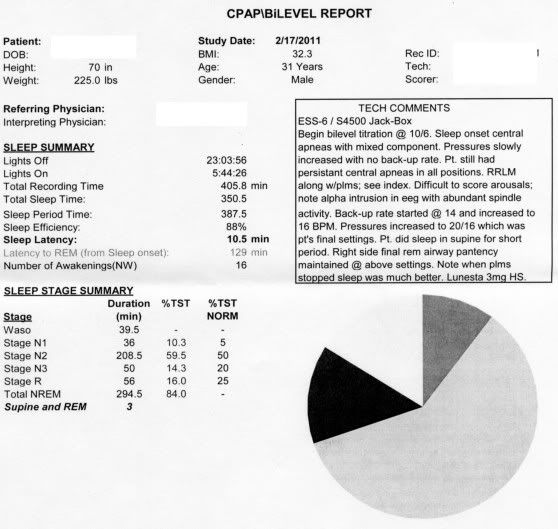
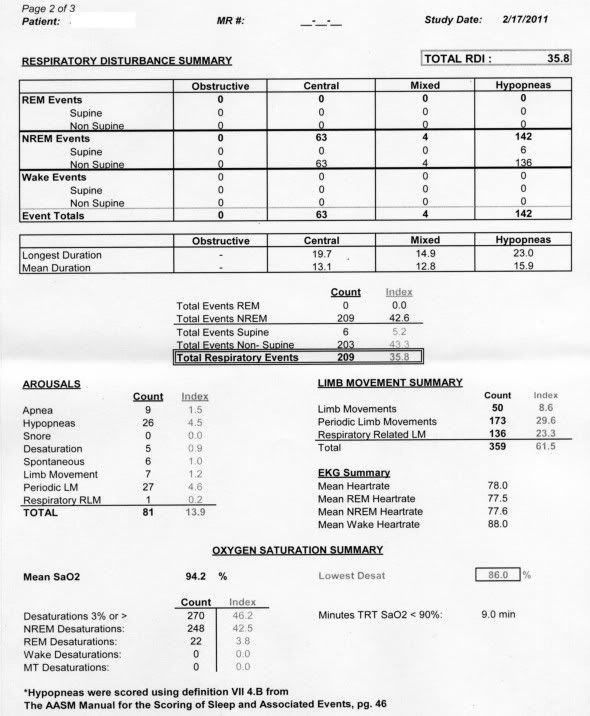
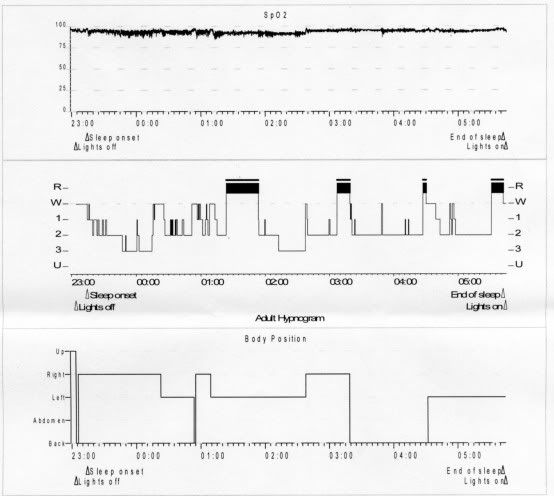
BIPAP ST TITRATION PSG