Links to Central Apnea
-
RDawkinsPhDMPH
- Posts: 77
- Joined: Fri Dec 03, 2010 7:15 pm
- Location: Pensacola, FL
- Contact:
Re: Links to Central Apnea
It is highly unlikely that CPAP (including flex/epr or auto) will drive the Pco2 low enough to induce a central apnea. It is very common for people (including docs sometimes) attribute CPAP emergent central apnea to this mechanism, however, it is more likely an example of the Hering-Breuer reflex, which limits the extend of chest expansion.
Re: Links to Central Apnea
RDawkinsPhDMPH, thanks for sharing that. Do you per chance know of recently-published citations attributing most CPAP-emergent central apnea to the Hering Breur reflex? At one point I also thought Hering-Breuer reflex was a likely explanation. However, today's CompSAS/CompSA/CSDB researchers seem to almost unanimously publish along the lines of CO2 homeostasis/sensitivity versus Hering-Breuer stretch. Again, thanks.RDawkinsPhDMPH wrote:It is highly unlikely that CPAP (including flex/epr or auto) will drive the Pco2 low enough to induce a central apnea. It is very common for people (including docs sometimes) attribute CPAP emergent central apnea to this mechanism, however, it is more likely an example of the Hering-Breuer reflex, which limits the extend of chest expansion.
- momofthree
- Posts: 24
- Joined: Mon Mar 01, 2010 10:43 pm
- Location: Michigan
Re: Links to Central Apnea
Great info everyone! Thanks.
John, question for you. Do you have any websites linking the kidney issue with the central sleep apnea? As you know our son's apneas are 100% Central in nature. The Neuro thinks that there might be an underlying condition and we have had the heart and brain tested thouroughly, and he just had a pulmonary assesment which showed what we had thought, comprimised breathing when sick and only when sick. I have never heard of a link to CSA and kidney issues. Our son also has an Iron Storage issue and a bleeding disorder. With the Iron Storage issue has not affected his blood cell counts, but he was severely deficient in his iron stores. When I researched it, all that I found was that Iron Storage issues are related to chronic underlying conditions. If you have any info please let me know. Thanks.
L. Mother of three angels.
John, question for you. Do you have any websites linking the kidney issue with the central sleep apnea? As you know our son's apneas are 100% Central in nature. The Neuro thinks that there might be an underlying condition and we have had the heart and brain tested thouroughly, and he just had a pulmonary assesment which showed what we had thought, comprimised breathing when sick and only when sick. I have never heard of a link to CSA and kidney issues. Our son also has an Iron Storage issue and a bleeding disorder. With the Iron Storage issue has not affected his blood cell counts, but he was severely deficient in his iron stores. When I researched it, all that I found was that Iron Storage issues are related to chronic underlying conditions. If you have any info please let me know. Thanks.
L. Mother of three angels.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: My son has CSA. |
- JohnBFisher
- Posts: 3821
- Joined: Wed Oct 14, 2009 6:33 am
Re: Links to Central Apnea
Hope it is a help. I know I did a lot of searching while trying to find something that worked for me. No doubt that was the case for many other posters. And if it helps the next person, it makes the effort worthwhile.momofthree wrote:... Great info everyone! Thanks. ...
I will hunt. However, my nephrologist seemed to imply kidneys are involved in breathing issues. Go figure. The more I learn about breathing, the more I wonder how we ever go about it! So much can go wrong. But most of the time, it just seems to work.momofthree wrote:... John, question for you. Do you have any websites linking the kidney issue with the central sleep apnea? ...
I will try to hunt down some resources. Those that seem appropriate I will post here.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: User of xPAP therapy for over 20 yrs. Resmed & Respironics ASV units with EEP=9cm-14cm H2O; PSmin=4cm H2O; PSmax=15cm H2O; Max=25cm H2O |
"I get up. I walk. I fall down. Meanwhile, I keep dancing” from Rabbi Hillel
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
- M.D.Hosehead
- Posts: 742
- Joined: Thu Jun 24, 2010 7:16 pm
- Location: Kansas
Re: Links to Central Apnea
JohnBFisher wrote:I will hunt. However, my nephrologist seemed to imply kidneys are involved in breathing issues. Go figure. The more I learn about breathing, the more I wonder how we ever go about it! So much can go wrong. But most of the time, it just seems to work.momofthree wrote:... John, question for you. Do you have any websites linking the kidney issue with the central sleep apnea? ...
FWIW, the only connection I'm aware of between kidney and respiration is the renal compensation for respiratory acidosis or alkalosis.
http://en.wikipedia.org/wiki/Acid-base_homeostasis
Renal disease could impair that compensatory mechanism, but I don't think it can cause CA. Conversely, any acidosis caused by CA would likely be compensated by hyperventilation before the renal mechanism could be effective.
_________________
| Mask: Forma Full Face CPAP Mask with Headgear |
| Additional Comments: MaxIPAP 15; MinEPAP 10; Also use Optilife nasal pillow mask with tape |
- JohnBFisher
- Posts: 3821
- Joined: Wed Oct 14, 2009 6:33 am
Re: Links to Central Apnea
Momofthree, if I remember correctly, M.D.Hosehead hit the nail on the head. My apologies that I did not remember clearly. At the time I was a bit overwhelmed by facing yet another diagnosis which I would rather not face. So, I did not fully remember the conversation with my nephrologist. However, once M.D.Hosehead stated the facts, it reminded me of the conversation. M.D.Hosehead, thank you for your input. I fear I have not slept well recently, so I am a bit more fuzzy headed than I would like.
In essense, M.D.Hosehead notes that the kidneys help compensate for impact of central apneas. But an imbalance or impairment of the kidneys would not cause the central apnea. I did find several articles that seemed to link severe renal failure to obstructive sleep apnea, but not to central sleep apnea.
Probably one of the most readable articles on cause and treatment of central sleep apnea is:
Central Sleep Apnea: Pathophysiology and Treatment
http://chestjournal.chestpubs.org/conte ... 5.full.pdf
Hope that helps.
In essense, M.D.Hosehead notes that the kidneys help compensate for impact of central apneas. But an imbalance or impairment of the kidneys would not cause the central apnea. I did find several articles that seemed to link severe renal failure to obstructive sleep apnea, but not to central sleep apnea.
Probably one of the most readable articles on cause and treatment of central sleep apnea is:
Central Sleep Apnea: Pathophysiology and Treatment
http://chestjournal.chestpubs.org/conte ... 5.full.pdf
Hope that helps.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: User of xPAP therapy for over 20 yrs. Resmed & Respironics ASV units with EEP=9cm-14cm H2O; PSmin=4cm H2O; PSmax=15cm H2O; Max=25cm H2O |
"I get up. I walk. I fall down. Meanwhile, I keep dancing” from Rabbi Hillel
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
Re: Links to Central Apnea
I'm certainly interested in this explanation as well.-SWS wrote:RDawkinsPhDMPH, thanks for sharing that. Do you per chance know of recently-published citations attributing most CPAP-emergent central apnea to the Hering Breur reflex? At one point I also thought Hering-Breuer reflex was a likely explanation. However, today's CompSAS/CompSA/CSDB researchers seem to almost unanimously publish along the lines of CO2 homeostasis/sensitivity versus Hering-Breuer stretch. Again, thanks.RDawkinsPhDMPH wrote:It is highly unlikely that CPAP (including flex/epr or auto) will drive the Pco2 low enough to induce a central apnea. It is very common for people (including docs sometimes) attribute CPAP emergent central apnea to this mechanism, however, it is more likely an example of the Hering-Breuer reflex, which limits the extend of chest expansion.
My understanding of Hering Breuer is that is that it's less of a force in adults vs. neonates, needs to be looked at in sleep a little more closely, elicitation of the response in adults only occurs with (relative to what we talk about here) VERY aggressive therapy, and even then, the response is not apnea but merely slowing of respiratory rate (bradypnea).
This is seen in the Laghi and Tobin work:
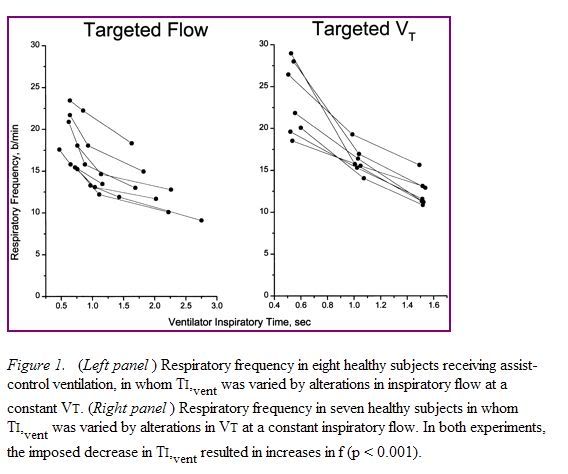
where in spite of huge changes in parameters, nothing even close to resembling central apnea is observed.
Interestingly, it appears that Time, and not Pressure, is the major culprit.
"Don't Blame Me...You Took the Red Pill..."
-
RDawkinsPhDMPH
- Posts: 77
- Joined: Fri Dec 03, 2010 7:15 pm
- Location: Pensacola, FL
- Contact:
Re: Links to Central Apnea
Basically, what I was referring, as far as Pco2 is concerned is related by SAG:
1. I specifically was referring to CPAP, not bilevel of any kind.
2. Though I didn't make it clear, I was also not referring to heart failure patients with CSR/CSA. In the case of a failing heart, CPAP can result in increased cardiac output and this can result in centrals caused by a decrease in Pco2.
3. The group I was referring to was the generally healthy person who exhibits random centrals at higher pressures on the titration night. Once set up on CPAP at home, a retitration a month or so later often does not exhibit centrals. Sometimes people also find themselves awakening abruptly on CPAP and they commonly complain of some minor chest wall discomfort.
There is a legitimate debate as to the cause of these centrals.
CPAP may result in increased inspiratory flow, shortened inspiratory time, and prolonged expiratory time. This could result in decreased Pco2 and ultimately to centrals. However, if this were the mechanism (a) why does it so often resolve after a month or two? Does the person learn to compensate with a lower tidal volume? and (b) why do they awaken suddenly rather than just resume breathing? Beyond that, it is hard to explain how CPAP drives the Pco2 low enough.
The overweight CPAP patient will likely have decreased chest wall compliance. The CPAP may result in a relative hyperinflation ("relative" to what they have been doing). They may pause because of a Hering-Breuer reflex, or (I give you, probably more likely.) a H-B "like" response to chest wall discomfort. Either way it is a simpler explanation for the observation that it often goes away in time, the abrupt awakenings, and complaints of chest wall pain. (Does the relative hyperinflation result in a physiologically significant increase in tidal volume? I Don't know.)
So it's a legitimate debate. It's just that for group 3, above, I find this a more parsimonious explanation of the observations. It is also probable that in the clinical setting we often don't adequately distinguish between those in group 2 above and in group 3 and, in fact, probably haven't in this thread.
But let's followup on the "pressure-induced" part of it.The phenomena of pressure-induced central apneas is tossed around far too freely. The vast majority of people do not get centrals because of ultra-therapeutic CPAP levels. BiLevel, Pressure Support (PSV) and Proportional Assist (PAV) Ventilation are another matter. You need some mechanism to drive the pCO2 below the sleeping apneic threshold, and plain old CPAP rarely is able to do that. OK, if you wanna argue that CPAP increases base lung volume (Functional Residual Capacity)(FRC), and since that increases gas exchange, some people can generate centrals that way, fine. But it's not as many as you might think.
SAG
1. I specifically was referring to CPAP, not bilevel of any kind.
2. Though I didn't make it clear, I was also not referring to heart failure patients with CSR/CSA. In the case of a failing heart, CPAP can result in increased cardiac output and this can result in centrals caused by a decrease in Pco2.
3. The group I was referring to was the generally healthy person who exhibits random centrals at higher pressures on the titration night. Once set up on CPAP at home, a retitration a month or so later often does not exhibit centrals. Sometimes people also find themselves awakening abruptly on CPAP and they commonly complain of some minor chest wall discomfort.
There is a legitimate debate as to the cause of these centrals.
CPAP may result in increased inspiratory flow, shortened inspiratory time, and prolonged expiratory time. This could result in decreased Pco2 and ultimately to centrals. However, if this were the mechanism (a) why does it so often resolve after a month or two? Does the person learn to compensate with a lower tidal volume? and (b) why do they awaken suddenly rather than just resume breathing? Beyond that, it is hard to explain how CPAP drives the Pco2 low enough.
The overweight CPAP patient will likely have decreased chest wall compliance. The CPAP may result in a relative hyperinflation ("relative" to what they have been doing). They may pause because of a Hering-Breuer reflex, or (I give you, probably more likely.) a H-B "like" response to chest wall discomfort. Either way it is a simpler explanation for the observation that it often goes away in time, the abrupt awakenings, and complaints of chest wall pain. (Does the relative hyperinflation result in a physiologically significant increase in tidal volume? I Don't know.)
So it's a legitimate debate. It's just that for group 3, above, I find this a more parsimonious explanation of the observations. It is also probable that in the clinical setting we often don't adequately distinguish between those in group 2 above and in group 3 and, in fact, probably haven't in this thread.
-
RDawkinsPhDMPH
- Posts: 77
- Joined: Fri Dec 03, 2010 7:15 pm
- Location: Pensacola, FL
- Contact:
Re: Links to Central Apnea
Oh and I often hear the argument that the OSAS has led to chronic CO2 retention, with compensatory bicarbonate shift, and that control of the OSAS with CPAP normalizes that and results in centrals. This makes no sense in a normal, healthy individual.
Re: Links to Central Apnea
Here is an example of what might be considered to be Hering-Breuer Inhibitory Response. A pressure increase results in an immediate and significant decrease in respiratory rate:
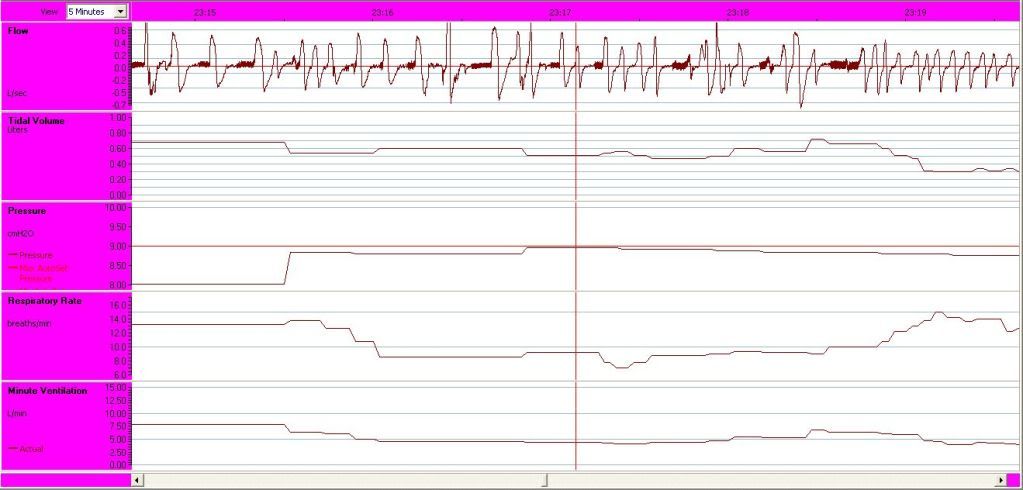
While this certainly looks impressive, the likelihood that a single cmH2O pressure increase could generate HBIR races past "highly unlikely" to "virtually impossible", and and this syllogistic relationship is not likely to hold up to vigorous scientific method.
While this certainly looks impressive, the likelihood that a single cmH2O pressure increase could generate HBIR races past "highly unlikely" to "virtually impossible", and and this syllogistic relationship is not likely to hold up to vigorous scientific method.
"Don't Blame Me...You Took the Red Pill..."
Re: Links to Central Apnea
My sleep study showed more than half of my apnea events were centrals prior to titration, ocurring mostly at sleep onset and awakening. My sleep doctor said centrals are normal and he wasn't concerned about that. I was put on CPAP where I continue to have about 10 centrals or more an hour (the obstructive events are down to about 1 or 2 an hour). It appears there are two thoughts on this--some doctors think they are normal and some do not. I do have sleep fragmentation 35 times an hour, so maybe that is why I have so many centrals. After reading extensively on centrals, I am confused on whether they are normal or not. Is it based on where in the sleep cycle you are?
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: I also use a Swift LT as a backup mask |
- JohnBFisher
- Posts: 3821
- Joined: Wed Oct 14, 2009 6:33 am
Re: Links to Central Apnea
I suspect what your doctor left out was that at sleep onset and while awakening, central sleep apneas are considered normal. If they do not disturb your sleep and your AHI with therapy is 5 or less, then it is considered normal.
Why at the transition between wakefullness and sleep (either falling asleep or awakening)? The mechanism used by the body to regulate shifts from one set of controls to another. This causes brief instability in your breathing during this period. Here's an excellent article that explains this:
Ventilation is unstable during drowsiness before sleep onset
http://jap.physiology.org/cgi/reprint/99/5/2036
Hope that helps explain why it might appear that some doctors ignore central sleep apneas. In fact, they know that at sleep onset and while awakening this is perfectly normal.
Why at the transition between wakefullness and sleep (either falling asleep or awakening)? The mechanism used by the body to regulate shifts from one set of controls to another. This causes brief instability in your breathing during this period. Here's an excellent article that explains this:
Ventilation is unstable during drowsiness before sleep onset
http://jap.physiology.org/cgi/reprint/99/5/2036
Hope that helps explain why it might appear that some doctors ignore central sleep apneas. In fact, they know that at sleep onset and while awakening this is perfectly normal.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: User of xPAP therapy for over 20 yrs. Resmed & Respironics ASV units with EEP=9cm-14cm H2O; PSmin=4cm H2O; PSmax=15cm H2O; Max=25cm H2O |
"I get up. I walk. I fall down. Meanwhile, I keep dancing” from Rabbi Hillel
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
Re: Links to Central Apnea
Thank you John, I guess that is where the confusion is for me. My AHI is around 13 (treated) with about 11of those AHI being centrals per hour. I still suffer from sleep fragmentation. Maybe he thinks they will just go away with time. That is an interesting article at the link you gave. Thank you.JohnBFisher wrote:I suspect what your doctor left out was that at sleep onset and while awakening, central sleep apneas are considered normal. If they do not disturb your sleep and your AHI with therapy is 5 or less, then it is considered normal.
Why at the transition between wakefullness and sleep (either falling asleep or awakening)? The mechanism used by the body to regulate shifts from one set of controls to another. This causes brief instability in your breathing during this period. Here's an excellent article that explains this:
Ventilation is unstable during drowsiness before sleep onset
http://jap.physiology.org/cgi/reprint/99/5/2036
Hope that helps explain why it might appear that some doctors ignore central sleep apneas. In fact, they know that at sleep onset and while awakening this is perfectly normal.
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: I also use a Swift LT as a backup mask |
- JohnBFisher
- Posts: 3821
- Joined: Wed Oct 14, 2009 6:33 am
Re: Links to Central Apnea
KimberlyM, please don't get me wrong. If your AHI score remains 13 per hour (excluding those transition events), then it should be addressed. Remember if you have a current machine that reports "Central Apneas", you can only really know that they APPEAR to be central apneas. You might have awaken just enough to toss and turn. And then you fell back asleep. Since they are transitional (between wakefulness and sleep), they would not be included in a sleep study.KimberlyM wrote:... Thank you John, I guess that is where the confusion is for me. My AHI is around 13 (treated) with about 11of those AHI being centrals per hour. I still suffer from sleep fragmentation. Maybe he thinks they will just go away with time. That is an interesting article at the link you gave. Thank you. ...
Still, an AHI over 5 should be addressed. And trust me, I know how dismissive doctors can be.
I heard from one doctor that central sleep apnea is very rare, so you can not have it. I then asked him if the sleep study showed that I had central sleep apneas. He answered yes. I asked if it was above 5 per hour, so should be treated. He said yes, but it did not need to be treated. Stupid, circular logic. Also, please understand that I used to work as a problem solver for a computer company for years. Though I might not know the medical industry, I am very, very good at solving complex issues. And rule number one of solving complex issues is to be certain you do NOT ignore unusual data.
I found another doctor, with whom I worked a couple years before he decided the traditional therapy would not make a difference. He also had the chance to see the progression of my neurological symptoms, so decided that my cause may well be neurological. I pushed him to try an ASV titration. It was a true godsend for me.
So, if you continue to have problems and your current doctor is unwilling to address continued AHI above 5, then you should find another doctor, who will work with you, your sleep lab and DME to find an answer that helps you resolve your sleep problems.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: User of xPAP therapy for over 20 yrs. Resmed & Respironics ASV units with EEP=9cm-14cm H2O; PSmin=4cm H2O; PSmax=15cm H2O; Max=25cm H2O |
"I get up. I walk. I fall down. Meanwhile, I keep dancing” from Rabbi Hillel
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
Re: Links to Central Apnea
Thanks John, the doctor put me on auto mode so I guess I will see how that works out. CPAP mode hasn't brought down what the machine views as centrals. I did have numerous centrals in the sleep study, so I am thinking they may be actual centrals on the CPAP, but who knows. I guess I will see if I do any better on autopap. I appreciate your help!JohnBFisher wrote:KimberlyM, please don't get me wrong. If your AHI score remains 13 per hour (excluding those transition events), then it should be addressed. Remember if you have a current machine that reports "Central Apneas", you can only really know that they APPEAR to be central apneas. You might have awaken just enough to toss and turn. And then you fell back asleep. Since they are transitional (between wakefulness and sleep), they would not be included in a sleep study.KimberlyM wrote:... Thank you John, I guess that is where the confusion is for me. My AHI is around 13 (treated) with about 11of those AHI being centrals per hour. I still suffer from sleep fragmentation. Maybe he thinks they will just go away with time. That is an interesting article at the link you gave. Thank you. ...
Still, an AHI over 5 should be addressed. And trust me, I know how dismissive doctors can be.
I heard from one doctor that central sleep apnea is very rare, so you can not have it. I then asked him if the sleep study showed that I had central sleep apneas. He answered yes. I asked if it was above 5 per hour, so should be treated. He said yes, but it did not need to be treated. Stupid, circular logic. Also, please understand that I used to work as a problem solver for a computer company for years. Though I might not know the medical industry, I am very, very good at solving complex issues. And rule number one of solving complex issues is to be certain you do NOT ignore unusual data.
I found another doctor, with whom I worked a couple years before he decided the traditional therapy would not make a difference. He also had the chance to see the progression of my neurological symptoms, so decided that my cause may well be neurological. I pushed him to try an ASV titration. It was a true godsend for me.
So, if you continue to have problems and your current doctor is unwilling to address continued AHI above 5, then you should find another doctor, who will work with you, your sleep lab and DME to find an answer that helps you resolve your sleep problems.
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: I also use a Swift LT as a backup mask |












