Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
The adapter can be found at cpap.com in the 02 supplies. Or for that matter at most any online DME provider's site under 02 supplies.
I have my concentrator, an Invacare Platinum XL (and before that a DeVilbiss), in the computer room NEXT to our bedroom. Hubby drilled a small hole in the adjacent wall just above the baseboard and we fed the 25" 02 tubing thru the hole to my VPAP Auto. And we've placed the concentrator on a carpet remnant. Voila! Cuts down on the noise AND the heat those concentrators throw.
I have my concentrator, an Invacare Platinum XL (and before that a DeVilbiss), in the computer room NEXT to our bedroom. Hubby drilled a small hole in the adjacent wall just above the baseboard and we fed the 25" 02 tubing thru the hole to my VPAP Auto. And we've placed the concentrator on a carpet remnant. Voila! Cuts down on the noise AND the heat those concentrators throw.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: PR SystemOne BPAP Auto w/Bi-Flex & Humidifier - EncorePro 2.2 Software - Contec CMS-50D+ Oximeter - Respironics EverFlo Q Concentrator |
Women are Angels. And when someone breaks our wings, we simply continue to fly.....on a broomstick. We are flexible like that.
My computer says I need to upgrade my brain to be compatible with its new software.
My computer says I need to upgrade my brain to be compatible with its new software.
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
Good thread. I am glad you got the pulseox and are following it up. I hope the O2 helps!
Btw can you remind us, do you or did you have any limb movements? Not that it would explain all the desats, but some of those graphs really seem to be spiking around a bit, I'm wondering how much of that is due to motion artifact? Just a thought, I am NOT discounting your recent experiences which are probably the cause of the low SPO2. Good luck! I don't have anything else to add so will lurk some more.
Btw can you remind us, do you or did you have any limb movements? Not that it would explain all the desats, but some of those graphs really seem to be spiking around a bit, I'm wondering how much of that is due to motion artifact? Just a thought, I am NOT discounting your recent experiences which are probably the cause of the low SPO2. Good luck! I don't have anything else to add so will lurk some more.
PR System One APAP, 10cm
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
Toronto, I sure am glad that you noticed the oxygen desaturations, so you can discuss this further with your doctor.
I've had my oximeter since about December, and I use it occasionally to spot-check that therapy's effective. I don't want to distract from the current discussion, but I thought that my own situation may be interesting to someone, so here are my results using the oximeter last night.
A quick background.... I have mild sleep apnea (moderate in supine position). There were obstructive apneas and hypopneas during my sleep study; no centrals were mentioned. My oxygen desaturation during the diagnostic study was 89%, so no big deal. Right now I'm using the S9 Autoset at set CPAP pressure of 7.4 with no EPR. My machine can report if apneas are centrals or obstructive. My average AHI is 0.4 (I've had three zero-AHI nights too), and I very rarely have any obstructive apneas or hypopneas. The few events I do have are usually centrals. My Leak Rate is usually zero.
I took the charts from the oximeter report and put those together with my ResScan events graph, using a graphics program. The green graph is Oxygen Saturation, and the blue graph is Pulse Rate. The apnea events are sandwiched in between those two graphs. The red event is an obstructive apnea, and the others are centrals. Here are last night's results (AHI was 0.6), with a brief explanation of the areas outlined in red below the charts:

1. Desaturation associated with the 10-second central apnea. Notice the sudden pulse rate drop at the same time. My pulse rate drops like this every night at about the same time. I believe this is a sleep state transition.
2. Desaturation to 87 (lower than my sleep study), associated with another 10-second central apnea.
3. Several desaturations, associated with a central and an obstructive apnea.
Although I know my own situation isn't of great concern, I thought that someone may learn from it. It's something I'm going to keep a closer eye on. There's not really anything I can do about the central apneas, since there are few and they can't be treated with pressure as obstructive apneas can. I don't think they're being caused by CPAP pressure, as my pressure's quite low (at 7.4). My titrated pressure was 6, so I may try that again soon and see how it affects results.
I've had my oximeter since about December, and I use it occasionally to spot-check that therapy's effective. I don't want to distract from the current discussion, but I thought that my own situation may be interesting to someone, so here are my results using the oximeter last night.
A quick background.... I have mild sleep apnea (moderate in supine position). There were obstructive apneas and hypopneas during my sleep study; no centrals were mentioned. My oxygen desaturation during the diagnostic study was 89%, so no big deal. Right now I'm using the S9 Autoset at set CPAP pressure of 7.4 with no EPR. My machine can report if apneas are centrals or obstructive. My average AHI is 0.4 (I've had three zero-AHI nights too), and I very rarely have any obstructive apneas or hypopneas. The few events I do have are usually centrals. My Leak Rate is usually zero.
I took the charts from the oximeter report and put those together with my ResScan events graph, using a graphics program. The green graph is Oxygen Saturation, and the blue graph is Pulse Rate. The apnea events are sandwiched in between those two graphs. The red event is an obstructive apnea, and the others are centrals. Here are last night's results (AHI was 0.6), with a brief explanation of the areas outlined in red below the charts:

1. Desaturation associated with the 10-second central apnea. Notice the sudden pulse rate drop at the same time. My pulse rate drops like this every night at about the same time. I believe this is a sleep state transition.
2. Desaturation to 87 (lower than my sleep study), associated with another 10-second central apnea.
3. Several desaturations, associated with a central and an obstructive apnea.
Although I know my own situation isn't of great concern, I thought that someone may learn from it. It's something I'm going to keep a closer eye on. There's not really anything I can do about the central apneas, since there are few and they can't be treated with pressure as obstructive apneas can. I don't think they're being caused by CPAP pressure, as my pressure's quite low (at 7.4). My titrated pressure was 6, so I may try that again soon and see how it affects results.
- M.D.Hosehead
- Posts: 742
- Joined: Thu Jun 24, 2010 7:16 pm
- Location: Kansas
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
DreamOn,
I love the way you constructed that chart. I've been trying to accomplish something similar, but doing it by hand (cutting up the printouts and trying to align them). It's hard to align the clock times since the graphs don't print at exactly the same scale.
Please consider starting a thread explaining how you created your chart.
I love the way you constructed that chart. I've been trying to accomplish something similar, but doing it by hand (cutting up the printouts and trying to align them). It's hard to align the clock times since the graphs don't print at exactly the same scale.
Please consider starting a thread explaining how you created your chart.
_________________
| Mask: Forma Full Face CPAP Mask with Headgear |
| Additional Comments: MaxIPAP 15; MinEPAP 10; Also use Optilife nasal pillow mask with tape |
- torontoCPAPguy
- Posts: 1015
- Joined: Mon Dec 28, 2009 11:27 am
- Location: Toronto Ontario/Buffalo NY
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
Hi all:
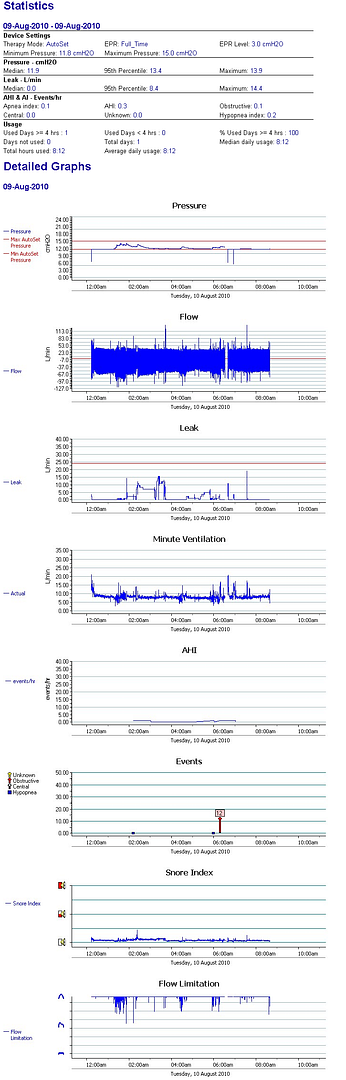
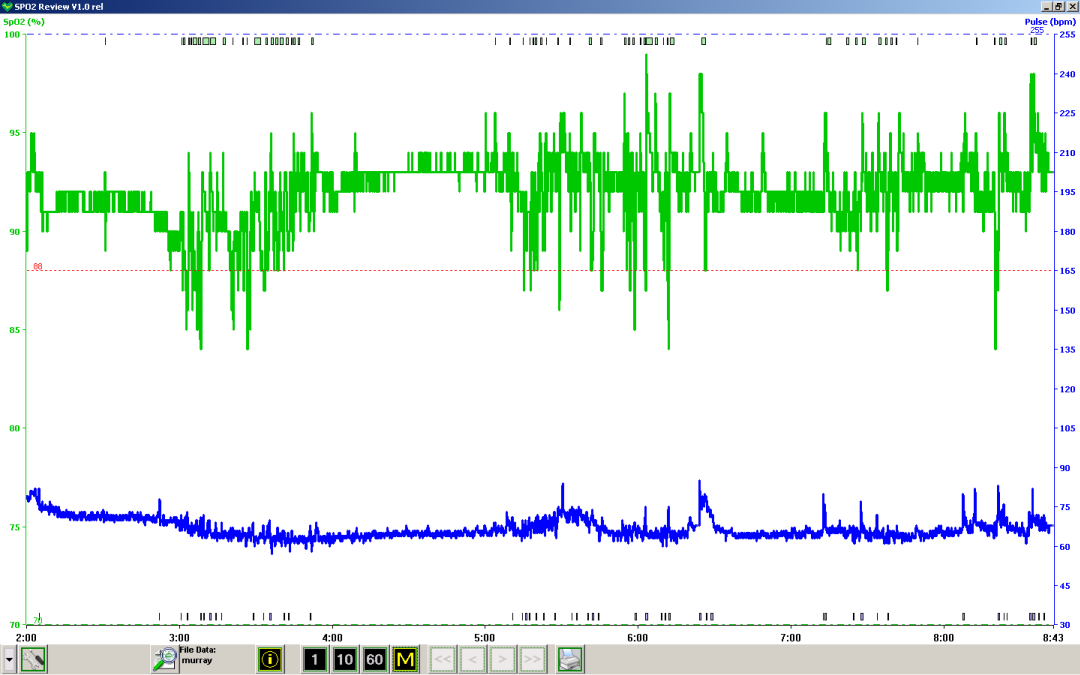
Today's data. Seems not as bad as that first day when I was dipping into the seventies with my blood oxygen saturation. I have been reading and discussing the benefits of bleeding in a small amount of O2 into the air tube to maintain SO2 levels in the mid nineties while sleeping and I am going to be discussing with my MD's this week. I picked up the only used oxygen concentrator I see advertised within 200 miles last night; a Mobilaire V with some 30K hours on it that is purportedly a refurbished unit. If my MD's think I am up for an oxygen concentrator I think my insurance and Ontario Assistive Devices program may pick up the tab for a new one (I'm going for a portable job - this thing is has to travel with me). My issue is that regardless of having pretty good numbers showing from my S9 my SO2 is erratic and at times drops into the 70ish % range. Not a good thing at all. But one wonders if even having So2 dropping into the mid 80's is disturbing one's sleep as I awaken as of late with feelings of mild anxiety and still somewhat tired, although once I get going, I'm good for the day. Anyway, here's my data from last night for any commentary and for the newbies to have a look at. And a picture of the Mobilaire V oxygen concentrator. I don't even know if it's working and blowing oxygen or plain air..... I suppose I could light a match and see if things explode!
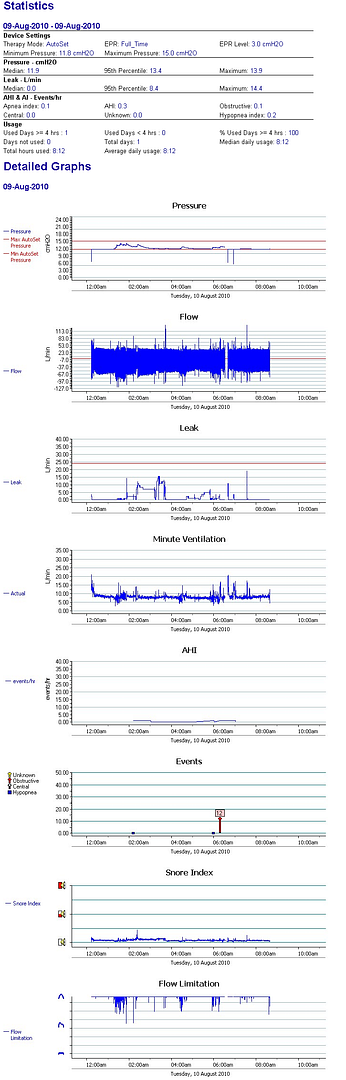
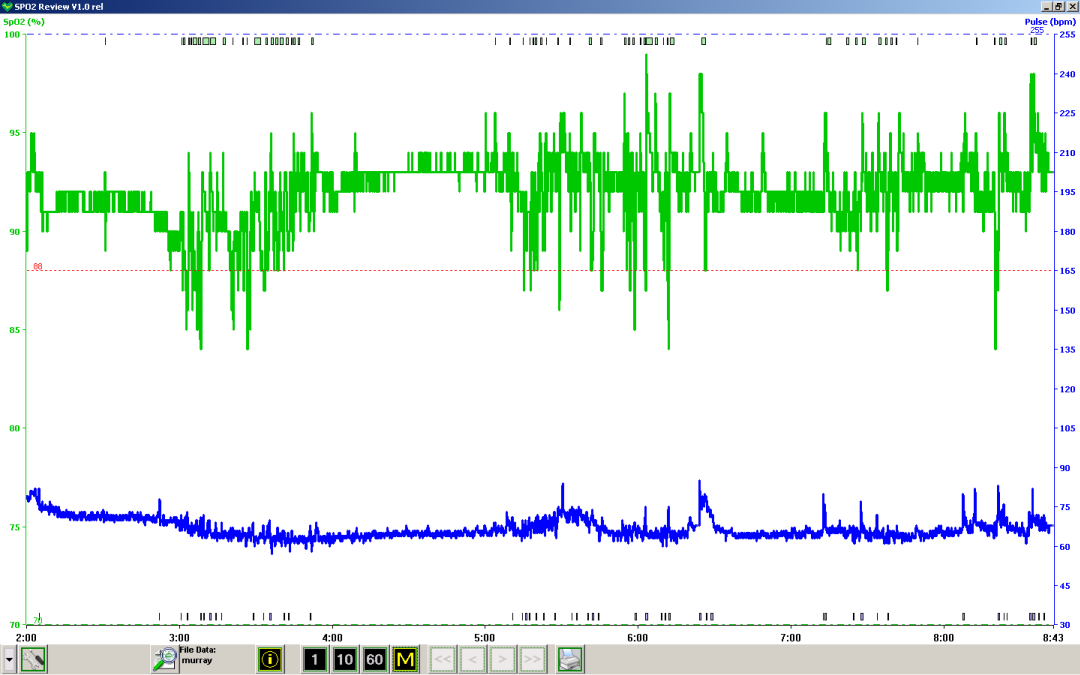

Today's data. Seems not as bad as that first day when I was dipping into the seventies with my blood oxygen saturation. I have been reading and discussing the benefits of bleeding in a small amount of O2 into the air tube to maintain SO2 levels in the mid nineties while sleeping and I am going to be discussing with my MD's this week. I picked up the only used oxygen concentrator I see advertised within 200 miles last night; a Mobilaire V with some 30K hours on it that is purportedly a refurbished unit. If my MD's think I am up for an oxygen concentrator I think my insurance and Ontario Assistive Devices program may pick up the tab for a new one (I'm going for a portable job - this thing is has to travel with me). My issue is that regardless of having pretty good numbers showing from my S9 my SO2 is erratic and at times drops into the 70ish % range. Not a good thing at all. But one wonders if even having So2 dropping into the mid 80's is disturbing one's sleep as I awaken as of late with feelings of mild anxiety and still somewhat tired, although once I get going, I'm good for the day. Anyway, here's my data from last night for any commentary and for the newbies to have a look at. And a picture of the Mobilaire V oxygen concentrator. I don't even know if it's working and blowing oxygen or plain air..... I suppose I could light a match and see if things explode!

_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Respironics Everflo Q infusing O2 into APAP line to maintain 95% SaO2; MaxTec Maxflo2 Oxygen Analyzer; Contec CMS50E Recording Pulse Oxymeter |
Fall colours. One of God's gifts. Life is fragile and short, savour every moment no matter what your problems may be. These stunning fall colours from my first outing after surviving a month on life support due to H1N1.
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
I know you will hate me for my post!!! please don't ok
I have COPD.......I don't feel the air coming into my mask. I have trouble breathing or getting what I feel is enough air. I know you will never understand why I have so much trouble don't worry your not here to explain it. I just tell you I wear my oxygen hose so I can breath!!!!!!
I have sleep apnea........but I just can't get use to my mask yes I am new here. But I can't tell you how hard it is to wear. Except I have one of the smallest heads and it is hard to keep on. I have to have my oxygen for my COPD.
When I read about your oxygen problem is simular to mind. They tested me over night with one of those oxymeters on my finger which was tape on so it wouldn't come off.
I went very low I think it went down to 69....I stay around in the 70's during the night.
Usually I will be around 86 to 88 without my oxygen if I am walking around or excerising.
I with my oxygen on will go around 90 to 94.
It is dangous to let your body go low like you were talking about it is hard on your heart! which I know you are all smarter then me know this.
But it could be cause from different reasons......do you smoke? It could be your brain, your heart, you really need to have some testing done no matter how young you are or old.
YOU might have sleep apean......but you might have other things wrong too.
Thank God you found you have a problem now.
I had mind low for some time without knowing it.....10/2008 they found a stint after 3 heart doctors poo poo me off for being a women. But I went in and they found 3 blockages and fix me.
But I still had my breathing problems after that. I found out that I had COPD during that time too. But what they didn't see I still had an oxygen problem.
So I by chance found another lung doctor who was into sleep study's.....and I never heard of sleep.
I have COPD.......I don't feel the air coming into my mask. I have trouble breathing or getting what I feel is enough air. I know you will never understand why I have so much trouble don't worry your not here to explain it. I just tell you I wear my oxygen hose so I can breath!!!!!!
I have sleep apnea........but I just can't get use to my mask yes I am new here. But I can't tell you how hard it is to wear. Except I have one of the smallest heads and it is hard to keep on. I have to have my oxygen for my COPD.
When I read about your oxygen problem is simular to mind. They tested me over night with one of those oxymeters on my finger which was tape on so it wouldn't come off.
I went very low I think it went down to 69....I stay around in the 70's during the night.
Usually I will be around 86 to 88 without my oxygen if I am walking around or excerising.
I with my oxygen on will go around 90 to 94.
It is dangous to let your body go low like you were talking about it is hard on your heart! which I know you are all smarter then me know this.
But it could be cause from different reasons......do you smoke? It could be your brain, your heart, you really need to have some testing done no matter how young you are or old.
YOU might have sleep apean......but you might have other things wrong too.
Thank God you found you have a problem now.
I had mind low for some time without knowing it.....10/2008 they found a stint after 3 heart doctors poo poo me off for being a women. But I went in and they found 3 blockages and fix me.
But I still had my breathing problems after that. I found out that I had COPD during that time too. But what they didn't see I still had an oxygen problem.
So I by chance found another lung doctor who was into sleep study's.....and I never heard of sleep.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
sorry I ran out of room //
I just wanted to say I never heard of sleep apnea or sleep study's.
Anyway it's been hard on me to use the machine....and mostly the masks even tho mind is the least ofensive you can buy as I know.
Thank you for letting me post........this is the most informative site I have found.
I just wanted to say I never heard of sleep apnea or sleep study's.
Anyway it's been hard on me to use the machine....and mostly the masks even tho mind is the least ofensive you can buy as I know.
Thank you for letting me post........this is the most informative site I have found.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
Last edited by mergh on Wed Aug 11, 2010 3:16 pm, edited 1 time in total.
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
Toronto, if you want to display all the oximeter sleep session data on the screen in the SpO2 program, click on the "M" icon and then check "AllData."
It doesn't appear that your oxygen desaturations are only associated with the apnea/hypopnea events. It is my impression from what you said earlier that you do plan to discuss this with your doctor. I think that's a good idea, as further testing may be necessary in order to determine exactly what's causing the desats during sleep. It may be that you're having a problem during the day too, perhaps due to the lung damage you suffered last summer?
I hope you'll let us know what you discover. And I hope that your difficulties resolve.
It doesn't appear that your oxygen desaturations are only associated with the apnea/hypopnea events. It is my impression from what you said earlier that you do plan to discuss this with your doctor. I think that's a good idea, as further testing may be necessary in order to determine exactly what's causing the desats during sleep. It may be that you're having a problem during the day too, perhaps due to the lung damage you suffered last summer?
I hope you'll let us know what you discover. And I hope that your difficulties resolve.
- torontoCPAPguy
- Posts: 1015
- Joined: Mon Dec 28, 2009 11:27 am
- Location: Toronto Ontario/Buffalo NY
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
This is indeed a great forum and thank you for your kind words, everyone.DreamOn wrote:Toronto, if you want to display all the oximeter sleep session data on the screen in the SpO2 program, click on the "M" icon and then check "AllData."
It doesn't appear that your oxygen desaturations are only associated with the apnea/hypopnea events. It is my impression from what you said earlier that you do plan to discuss this with your doctor. I think that's a good idea, as further testing may be necessary in order to determine exactly what's causing the desats during sleep. It may be that you're having a problem during the day too, perhaps due to the lung damage you suffered last summer?
I hope you'll let us know what you discover. And I hope that your difficulties resolve.
Yes, I was just saying in a PM that I have no doubt that my SaO2 issues are to do not only with apnea/hypopnea (it becomes more and more apparent) but also as a result of lung damage from being on life support with horrific pneumonia last summer as a result of H1N1. The bottoms of my lungs are hardened and the insides are all torn to ratpoop from being suctioned in an attempt to save my life (seems to have worked). Last tests at the hospital via the Respirologist (best in the country I am told) showed 70% lung capacity at best and remember that these measurements are taken after the technician tells you to inhale and exhale like your life depended on it as opposed to just going about your business and breathing normally. At sleep I am certain that my breathing becomes very shallow, especially if I am very tired or exhausted as I was during that first graph. It still looks like my SaO2 drops regularly into the mid to low 80's though (and not the 70's like that first night) which is still unacceptable to me although it may be alright with the MD's. I was also just saying that since we have the technology wouldn't it be a great thing to have an oxygen concentrator connected to a fingertip oximeter like that Contec 50E via a computer that would make minor adjustments in oxygen insertion into the nosebag to keep one at 95% all the time while sleeping? I'd bet money that would improve one's night of sleep because the body would not continuously be hollering "Attention Will Robinson! Emergency! Wake up and Breathe Deeply! Low SaO2! Low SaO2!) My gut feeling is that my body is arousing me multiple times throught the night as it notes my SaO2 falling in order to get me to breather more deeply and killing my sleep patterns. I am going to try and get TWO more sleep studies done if I can. One with just the APAP S9 Auto running as I have it presently set up. And a second with a bleed of 2 or 3 L of O2 into the feedpipe to the mask. Might be a very very interesting reslut and of significant clinical value to all on the forum to discover the difference in sleep patterns between the two based on EEG, EKG, BP, SaO2, etc. Very interesting indeed. All I need to do now is convince either my MD's or the sleep clinic proprieter that this is a worthwhile venture. Is there anyone out there that has a device that tracks SaO2 during sleep and adjusts the infusion of O2 based on oximetry? If not, I think I am going to talk to my respirologist who would love a cushy pension to retire on early... this is a business venture that just might be worth pursuing. Beats wearing that nose canula all night in hospital and having tons of O2 rammed up your nose based on best guess as to what you might need while asleep. Interesting thought? Comments? I can do this thing; all I need to do is find an oxygen concentrator that is adjustable based on electronic input and not the turning of a knob. Better half is making me an appointment to see the Respirologist(s) asap to get this venture underway but I may not wait and infuse some O2 into the line sooner than later. At 2L or 3L the amount being presented to one's nose is so minor as to be almost insignificant. I was set at 5L when I started hanging up the oxygen line in the hospital as it was such a pain and dried out my nose. Jeez, I had forgotten what a nasty experience THAT was. Fortunately I was in a coma when I was intubated and on the ventilator.
My friends, YOU are ALL compromised and I strongly recommend to your earnest consideration getting your flu shots as early as you possibly can. They may not eliminate the risk of the new strain of H1N1 that is on its way but it will improve your odds of keeping out of the hospital.
In closing I share with you the words of my respirologist to make my point , after he stared at me for a full minute or two. "I'm sorry to stare, but the only X-Rays (of lungs) that I have ever seen that were this solidly white were on corpses from autopsy". Bedside manner was not his strong point but when you are the best in the country you can pretty much say what the heck you want, right?
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Respironics Everflo Q infusing O2 into APAP line to maintain 95% SaO2; MaxTec Maxflo2 Oxygen Analyzer; Contec CMS50E Recording Pulse Oxymeter |
Fall colours. One of God's gifts. Life is fragile and short, savour every moment no matter what your problems may be. These stunning fall colours from my first outing after surviving a month on life support due to H1N1.
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
Well ..... since you weren't a corpse and you were breathing on your own ... I guess you could take that comment as a compliment and an accomplishment.
"Look Doc!! All white and still breathing! Nyah, nyah!"
"Look Doc!! All white and still breathing! Nyah, nyah!"
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: PR SystemOne BPAP Auto w/Bi-Flex & Humidifier - EncorePro 2.2 Software - Contec CMS-50D+ Oximeter - Respironics EverFlo Q Concentrator |
Women are Angels. And when someone breaks our wings, we simply continue to fly.....on a broomstick. We are flexible like that.
My computer says I need to upgrade my brain to be compatible with its new software.
My computer says I need to upgrade my brain to be compatible with its new software.
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
In my experience, this situation could easily cause anxiety and fatique. The good news is you may now be on a path to great improvement thanks to your oximetry studies.torontoCPAPguy wrote: But one wonders if even having So2 dropping into the mid 80's is disturbing one's sleep as I awaken as of late with feelings of mild anxiety and still somewhat tired, although once I get going, I'm good for the day.
Rooster
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
mergh wrote:
What are your CPAP pressure settings?
Rooster
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
- torontoCPAPguy
- Posts: 1015
- Joined: Mon Dec 28, 2009 11:27 am
- Location: Toronto Ontario/Buffalo NY
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
Rooster: After much playing around with minute pressure changes (don't ask me why the minute changes make such a difference) I have landed at 11.8 to 15 cmH2O. I have been thinking of shifting the whole shebang up by 1 cm to see, again, what it will do. I know, already, that shifting it down by 1 cm only (to 10.8 to 14) causes all heck to break loose with tons of events all night. I HAVE gone from a nose mask to a full face mask about ten days ago and I am wondering if the effect of the positive airway pressure is as efficient. With the nose mask, if I opened my mouth it was like a train whistle of air coming out. Of course, with the full face mask, the pressure on my mouth and nose are equal so any pressure being exerted pushes air directly into my lungs. I generally get a pretty good seal with either the Mirage Activa nose mask or the Mirage Quattro Pro full face mask which allows me to breathe through my mouth on days when my allergies stuff up my nose during the night. So, I am pretty certain that my issues relate to my hospital stay last summer; the hardening of the bottom of my lungs (I can hardly take a walk with anything in my stomache pushing up on my lungs as they are not pliable like they once were). Also, they physically suctioned out the fluid and 'crap' (pardon) from my lungs several times chewing them up a bit. THIS is what I believe is the cause of my SaO2 problem (which is not huge but needs attention) combined with my OSA apneas and hypopneas. In the end, I think that only a sleep study without the O2 and a sleep study WITH the O2 is going to determine the final efficacy with/without; and I fall asleep so easily at night that it could, in fact, be a split study. I feel that I should be having another sleep study at this time anyway since I have taken the time and effort to titrate myself and monkey around until my numbers are as good as they can be (they originally prescribed my CPAP, no data, 9cm H2O and goodbye forever). This is NOT a goodbye forever condition - not by a long shot. I believe that if you are not running your own numbers by your doctor at least once every few months that you should be having a sleep study done at least once or twice a year to ensure that your numbers are what they once were. AND if despite the fact that you can get your OSA numbers low (AHI, apneas, hypopneas, leakage, etc.) your SaO2 keeps knocking the "Danger Will Robinson" line and below, that it is likely the best treatment to infuse a small amount of O2 into your air line during the night. My SaO2 during the day at rest runs 90-93 say... and when active actually rises to around 96-97. But put me to bed and asleep and it plummets and as you can see sometimes knocks the mid 70% range if I am really tired and sleeping deeply. And THAT is dangerous - exactly as dangerous as the OSA untreated itself as, according to my MD's, low SaO2 results directly in poor function of the organs (including the brain and the liver) which messes up your medications and interactions and even more urgently, it results directly in the body pumping up the blood pressure to try and get oxygen to the organs. If you are diabetic, you are in double trouble as the oxygenation of your wee extremities is going to go down the tube as well, resulting in tingling fingers and toes and you will eventually have them lopped off by a surgeon.
So, yes, despite the OSA being 'under control' if you are still suffering from low SaO2 when you are deep asleep, you (me) have a serious issue that will eventually result in serious problems. It has to be addressed and as early as possible. Hence my desire to infuse 2 or 3L of oxygen into the air line while monitoring my SaO2 during the night to see if it brings me up to 95% across the board through the night. At that point I can safely say to my MDs that THIS is what I need unless you have a better suggestion. I have, by the way, every puffer known to mankind... Ventolin, Atrovent, and two steroidal puffers. They are to be used as needed and I have not used them all year long until allergy season. And now I find myself wheezing if I spend a day in the great outdoors up north in the hinterland. They help but are not a cure-all. I have to take a water pill (Furosemide) from time to time to get the fluid out of my lungs that has been brought on by pollen and other allergens. If I stay in the air conditioned house, with the electronic air cleaner going, no problems. But that's not me. My home will never be my prison.
In any event, I appreciate the good suggestions and discussion. This is how we all learn and improve. Keep it up please. I am ordering the plumbing for the oxygen concentrator tonight and hope to have it online in the next few days. When I do get it online, you will have seen the bad side of my SaO2 and hopefully, with infusion of O2 you will see the good side of my SaO2. Fingers crossed. Waking up groggy and having it take 2-3 hours to clear my head is no fun. The headaches are no fun. Hopefully this is a potential solution and as they say "any port in a storm".
So, yes, despite the OSA being 'under control' if you are still suffering from low SaO2 when you are deep asleep, you (me) have a serious issue that will eventually result in serious problems. It has to be addressed and as early as possible. Hence my desire to infuse 2 or 3L of oxygen into the air line while monitoring my SaO2 during the night to see if it brings me up to 95% across the board through the night. At that point I can safely say to my MDs that THIS is what I need unless you have a better suggestion. I have, by the way, every puffer known to mankind... Ventolin, Atrovent, and two steroidal puffers. They are to be used as needed and I have not used them all year long until allergy season. And now I find myself wheezing if I spend a day in the great outdoors up north in the hinterland. They help but are not a cure-all. I have to take a water pill (Furosemide) from time to time to get the fluid out of my lungs that has been brought on by pollen and other allergens. If I stay in the air conditioned house, with the electronic air cleaner going, no problems. But that's not me. My home will never be my prison.
In any event, I appreciate the good suggestions and discussion. This is how we all learn and improve. Keep it up please. I am ordering the plumbing for the oxygen concentrator tonight and hope to have it online in the next few days. When I do get it online, you will have seen the bad side of my SaO2 and hopefully, with infusion of O2 you will see the good side of my SaO2. Fingers crossed. Waking up groggy and having it take 2-3 hours to clear my head is no fun. The headaches are no fun. Hopefully this is a potential solution and as they say "any port in a storm".
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Respironics Everflo Q infusing O2 into APAP line to maintain 95% SaO2; MaxTec Maxflo2 Oxygen Analyzer; Contec CMS50E Recording Pulse Oxymeter |
Fall colours. One of God's gifts. Life is fragile and short, savour every moment no matter what your problems may be. These stunning fall colours from my first outing after surviving a month on life support due to H1N1.
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
Toronto, I really hope the O2 helps. It is a great idea to push for a new study with o2, or at least discuss it with the sleep doctor (that listens). Your situation is too unique/important not to let these important pulse ox observations go by without being addressed.
For fun I played around with my pulse ox a bit, movements of the arm don't really seem to make any difference in my spo2 levels or the HR it registers, even if I swing my arms around wildly. So motion artifact should not be an issue. If that happens, perhaps you have a defective unit or maybe you need to use a finger that's smaller. (not that you mentioned this problem, was just thinking out loud). Fwiw!
White lungs indeed If you are into the herbal thing, there are some herbs that are supposed to help the lungs, but I don't know how much they might help in your case.
For fun I played around with my pulse ox a bit, movements of the arm don't really seem to make any difference in my spo2 levels or the HR it registers, even if I swing my arms around wildly. So motion artifact should not be an issue. If that happens, perhaps you have a defective unit or maybe you need to use a finger that's smaller. (not that you mentioned this problem, was just thinking out loud). Fwiw!
White lungs indeed If you are into the herbal thing, there are some herbs that are supposed to help the lungs, but I don't know how much they might help in your case.
PR System One APAP, 10cm
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Re: Low SO2: Attention Will Robinson! Low SO2! Seek Shelter!
I just got caught up on this thread. I'm sorry you're having these issues, but am thrilled that you are doing everything you can to address the low oxygen levels.
One of the things I did a while back was to watch the pulse ox monitor before going to sleep -- while I was laying in bed. I had the ventilator on WITHOUT the oxygen for 15-30 minutes. My levels were mid to low 90's and pretty much stayed there. I turned the oxygen on and within a minute or two, my oxygen level jumped into the upper 90's (definitely above 95). I've also gone a whole night without the oxygen to see if it made any difference in how easy it was to breathe, how well I slept and how I felt the next day. It is definitely easier for me to breathe WITH the added oxygen and I slept better with it as opposed to without it.
For those that have asked about how to pipe the oxygen in, my configuration pipes the oxygen directly into the ventilator through a port in the back. I can feel the difference in the air within a minute or so of turning the oxygen on.
Just a reminder for those that are new at this and/or have never been told (as I was not) -- you should make sure your xpap is turned ON first, then the oxygen -- then turn them off in reverse order. You don't want the oxygen on without the xpap being on. The reason for this is that you don't want oxygen being pumped into the machine that isn't working itself.
Words to the wise -- benefit of my experience -- etc.
One of the things I did a while back was to watch the pulse ox monitor before going to sleep -- while I was laying in bed. I had the ventilator on WITHOUT the oxygen for 15-30 minutes. My levels were mid to low 90's and pretty much stayed there. I turned the oxygen on and within a minute or two, my oxygen level jumped into the upper 90's (definitely above 95). I've also gone a whole night without the oxygen to see if it made any difference in how easy it was to breathe, how well I slept and how I felt the next day. It is definitely easier for me to breathe WITH the added oxygen and I slept better with it as opposed to without it.
For those that have asked about how to pipe the oxygen in, my configuration pipes the oxygen directly into the ventilator through a port in the back. I can feel the difference in the air within a minute or so of turning the oxygen on.
Just a reminder for those that are new at this and/or have never been told (as I was not) -- you should make sure your xpap is turned ON first, then the oxygen -- then turn them off in reverse order. You don't want the oxygen on without the xpap being on. The reason for this is that you don't want oxygen being pumped into the machine that isn't working itself.
Words to the wise -- benefit of my experience -- etc.
_________________
| Mask: FlexiFit HC431 Full Face CPAP Mask with Headgear |
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Trilogy EVO. S/T AVAPS, IPAP 18-23, EPAP 10, BPM 7 |












