1. You are a CPAP survivor and a good Samaritan and are willing to help others through a difficult adjustment.
2. You are new to CPAP, going for a sleep study, seeing your Dr after a study and don't know what to expect.
3. You are having problems or someone you love/know is having problems with Sleep Apnea or therapy.
I guess you could be a combination of any or all of the above 3 or even be a vendor but I think those 3 categories cover most people.
The majority of folks likely to belong to the 3rd group or the 2nd group, I'm one myself being new, and having problems with a some of 1st thrown in which is why I'm writing this post.
As important as a the CPAP/APAP statistics that you get from your data capable machines are they are just part of the Sleep Apnea therapy puzzle for many people. There is a reason that during your sleep study they had you hooked up to an Oximeter all night long, your O2 Saturation is a major indicator of general health and a specific indicator of pulmonary function and sleep apnea.
From my observations and discussions in person and on line with Sleep Apnea patients there appears to be a general failure by many sleep therapists (Drs, Respriatory Therapists etc.) to validate effectiveness of Sleep Apnea therapy through the use of a follow up overnight Oximetery study. Of course a follow up sleep study while on your own machine would be even better, but that is a lot of expense when a relatively inexpensive Oximetery study will at least validate that you are at least getting enough O2.
I discussed with my doctor when he wrote the APAP prescription that I wanted a follow up Oximetery study to verify that the low O2 saturation observed during the initial over night Oximetery study and during the two Sleep studies were now gone, he agreed and we decided to do one after the first month of therapy.
Since I'm a firm believer that no two nights of sleep are the same I decided to purchase my own Oximeter to evaluate my on going sleep therapy over time rather than having to wait for the Dr. to order one. At least with my Sleep lab an overnight Oximetery study is only $50 so if you don't want to buy an Oximeter getting a study is still reasonable.
While we can make sure we use our equipment, control our leaks, and monitor our AHI and other statistics, which is the important first line of attack in treating our disease, but validating the effectiveness of Sleep Therapy should rely on something more then just how we feel each morning, since that can be influenced by many factors.
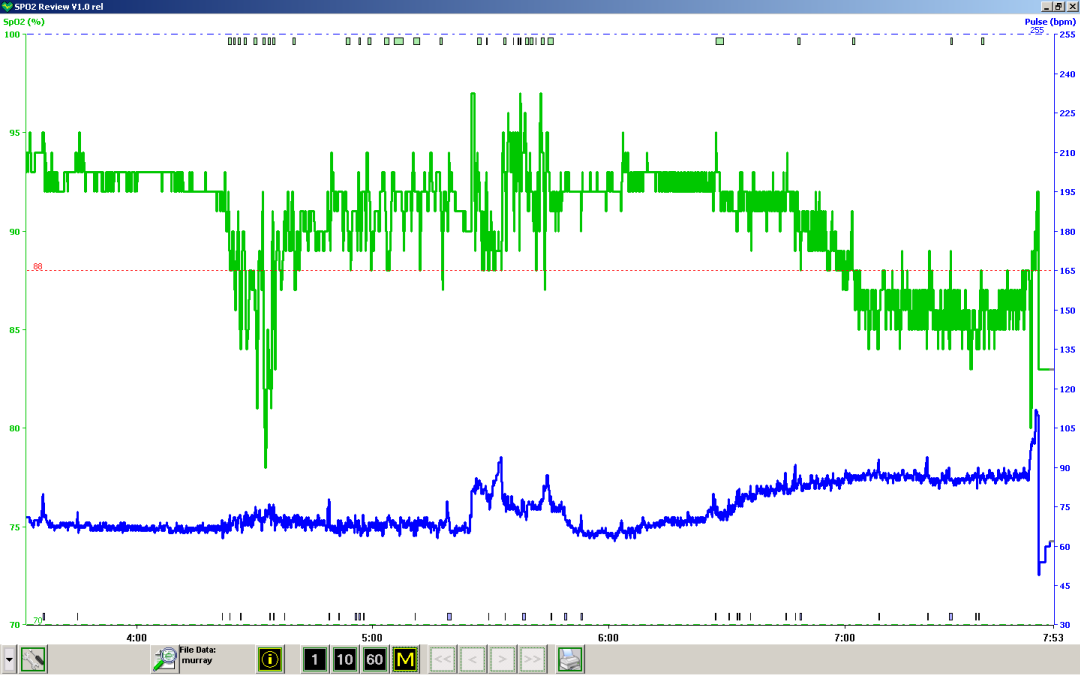
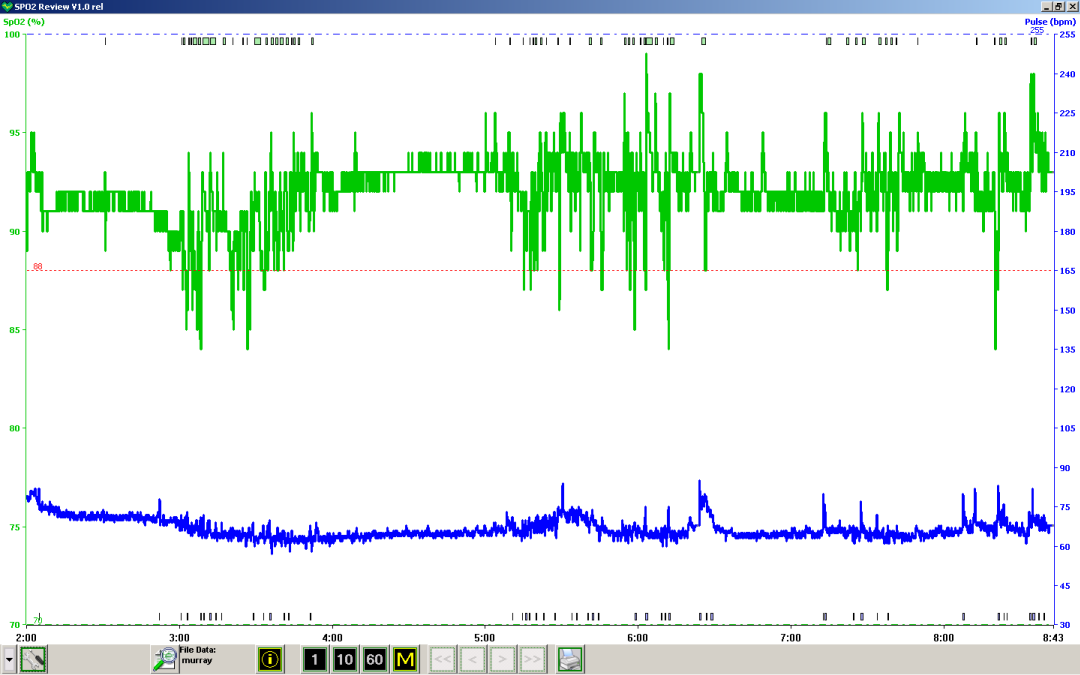
With my leaks under control and an AHI of less then 2, here is what my Oximeter showed

It is a good thing I followed up with Oximetery, since it was necessary to add supplemental O2 to my Sleep Therapy. Had I relied just on the statistics from my APAP I would have continued to suffer from nightly O2 deprivation.
If you are happy with your sleep therapy and feel great you probably aren't reading this, if you aren't happy or feeling better after sleep therapy I recommend getting an overnight Oximetery study done or purchase your own Oximeter so that you can monitor your O2 saturation levels while sleeping.
Now if I can get my other problems, RLS, PLMD, Pain and waking up because my mask bothers me under control maybe I can get some decent sleep again but at least I know I'm not starving my body for oxygen every night.
Besides checking the stats in my APAP weekly, I will continue to do twice monthly Oximetery to verify that I'm getting the O2 that I need from my Sleep Therapy.
Good Luck Everyone.
John