AHI and blood oxgen saturation
AHI and blood oxgen saturation
dug out my first sleep study (Kaiser, sleep in) done 10 years ago:
- 6 hour of sleep during study
- 50 obstructive apneas
- 102 hyponeas and numerous mixed and central apneic events
- Apnea Index measurs 25.9, with a total respiratory disturbance index of 40.7
- minimum blood oxygen saturation recorded was 63%, with 14% of the sleep time spend with O2 sat below 90%.
Question:
1) Is my AHI 25.9?
2) several years later, I showed this report to another doctor with a different insurance, the primary Dr. did not believe the report.
and ordered another one. He said you are so young ( 37 at the time) and if your blood oxygen is so low, you should be dead.
Of course, the 2nd sleep study came back similar. Does other people who had in clinic study also suffer from low oxgen saturation due to OSA?
just wondering.
It's wonderful to find this community of fellow suffers to compare notes!
- 6 hour of sleep during study
- 50 obstructive apneas
- 102 hyponeas and numerous mixed and central apneic events
- Apnea Index measurs 25.9, with a total respiratory disturbance index of 40.7
- minimum blood oxygen saturation recorded was 63%, with 14% of the sleep time spend with O2 sat below 90%.
Question:
1) Is my AHI 25.9?
2) several years later, I showed this report to another doctor with a different insurance, the primary Dr. did not believe the report.
and ordered another one. He said you are so young ( 37 at the time) and if your blood oxygen is so low, you should be dead.
Of course, the 2nd sleep study came back similar. Does other people who had in clinic study also suffer from low oxgen saturation due to OSA?
just wondering.
It's wonderful to find this community of fellow suffers to compare notes!
Re: AHI and blood oxgen saturation
At my study I had:
78 events; 1 apnea and 77 hypopneas
AHI was 16
O2 saturation: minimum was 76% (my study doesn't show a % of time below 90%)
So, even though I have hypopnea syndrome, my AHI still puts me into the moderate category, and my O2 bottomed out pretty low although not nearly as low as your 63%. Doc said I spent significant time below 88% which is the threshold for serious issues.
78 events; 1 apnea and 77 hypopneas
AHI was 16
O2 saturation: minimum was 76% (my study doesn't show a % of time below 90%)
So, even though I have hypopnea syndrome, my AHI still puts me into the moderate category, and my O2 bottomed out pretty low although not nearly as low as your 63%. Doc said I spent significant time below 88% which is the threshold for serious issues.
Yes, that blue eyed beauty is my cat! He is a seal point, bi-color Ragdoll. I adopted him in '08 from folks who could no longer care for him. He is a joy and makes me smile each and every day.
- torontoCPAPguy
- Posts: 1015
- Joined: Mon Dec 28, 2009 11:27 am
- Location: Toronto Ontario/Buffalo NY
Re: AHI and blood oxgen saturation
With a blood oxygen saturation of 63% you are indeed fortunate to be with us as it would have shot your blood pressure through the roof. Your AHI will vary from day to day and was 25.9 at the time that the sleep study was done. You should find out what your AHI was during the second sleep study. In fact, you should have copies of both sleep studies for your records. With such severe OSA you should be using, in my humble opinion, a data recording APAP machine like the ResMed S8 Autoset II or the S9 Auto (take the data with a grain of salt but it is very valuable data and should be kept on record daily). Your target for your AHI should be to get it under 1.0 if you can.... I have actually got mine down to 0.0 on several nights, but it will vary from night to night. More importantly, you want to keep an eye on your apnea events, hypopnea events, leak rates, etc., and learn to put all of that information together in order to proactively, with or without the help of your MD, get the best overall results that you can. I would also humbly suggest that you look at getting a recording pulse oximeter like the Contec 50E and recording your own blood oxygen saturation during the night on a regular basis to ensure that your CPAP machine is doing its job. You NEVER EVER want that SO2 to go down to 63% again - it will kill you dead as a doornail. In hospital they used to wake me at night by taking my blood oxygen and if it was below 90% they would fully awaken me and get me to take deep breaths to get it up above 90%.... fortunately it was generally not far below 90% when they took it but then again I was never really deep, deep asleep. My sleep study showed I went down into the 70% range and I was on a CPAP machine days later. My SO2 now never goes down below 90% at night and my night sweats, headaches, beating heartbeats, etc., have disappeared. So has my feeling of 'lack of air' at night.kelingdun wrote:dug out my first sleep study (Kaiser, sleep in) done 10 years ago:
- 6 hour of sleep during study
- 50 obstructive apneas
- 102 hyponeas and numerous mixed and central apneic events
- Apnea Index measurs 25.9, with a total respiratory disturbance index of 40.7
- minimum blood oxygen saturation recorded was 63%, with 14% of the sleep time spend with O2 sat below 90%.
Question:
1) Is my AHI 25.9?
2) several years later, I showed this report to another doctor with a different insurance, the primary Dr. did not believe the report.
and ordered another one. He said you are so young ( 37 at the time) and if your blood oxygen is so low, you should be dead.
Of course, the 2nd sleep study came back similar. Does other people who had in clinic study also suffer from low oxgen saturation due to OSA?
just wondering.
It's wonderful to find this community of fellow suffers to compare notes!
It sounds unbelievable to me that your MD's are not taking a far, far more aggressive approach to your treatment and if that is the case indeed, I would change MD's right now and I would become very proactive in my own health. I can tell you that as sure as the nose on your face that your life is at risk if your blood oxygen is going that low at night and you need to pay attention to this issue right now. Today. "Whatever it takes" needs to be your motto. And you need to become your own advocate for better medical attention. I know that I have not been bothered by any of my MD's since my last sleep study during which I was prescribed a pressure of 9.8 cmH2O and wished the best of luck. No recalls, NOTHING. It took me six months of experimenting with minor changes in my pressure range (and I bought my own APAP machines as they prescribed CPAP at 9. and it took my own efforts at getting a proper fitting mask and education on OSA (and I do not profess to be an expert by a long stretch) and the help of friends on this forum in order to get to where I am... decent SO2 levels, AHI generally under 1.0, a pressure range that works well for me (minute changes make a huge difference) and so on. Take everything you hear or read on here with a grain of salt, of course, but you are hearing from those that have the T shirt and have been where you are right now.
The choice, of course, is ultimately yours, but IMHO, with some of the finest MD's in the world, it was still up to ME and ME alone to take responsibility for my health.
Good luck to you. Welcome aboard and now it is time to make some life decisions and get going.
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Respironics Everflo Q infusing O2 into APAP line to maintain 95% SaO2; MaxTec Maxflo2 Oxygen Analyzer; Contec CMS50E Recording Pulse Oxymeter |
Fall colours. One of God's gifts. Life is fragile and short, savour every moment no matter what your problems may be. These stunning fall colours from my first outing after surviving a month on life support due to H1N1.
- torontoCPAPguy
- Posts: 1015
- Joined: Mon Dec 28, 2009 11:27 am
- Location: Toronto Ontario/Buffalo NY
Re: AHI and blood oxgen saturation
BTW, as a matter of interest, when I was on life support and then when I was on oxygen to maintain my SO2 levels, the alarms were set to go off at 89% or below. When I was more or less 'conscious' and still on oxygen, they would poke me and tell me to breathe deeply if it fell below 89%. Of course, when on a ventilator/respirator you have no choice in how deeply you are breathing as it is the machines doing the breathing for you... so they just tweak the oxygen concentration and how much is getting pushed into you and sucked back out.
Funny thing is that they sent me home without a word about sleep apnea.... it was after discharge from hospital without so much as a handshake that we took the rounds of cardiologist, respirologists, etc., in an attempt to be my own advocate for my own life and health. And even then they were getting it wrong and not really being aggressive in my diagnosis and treatment. It was the mention of the snoring and night sweats REPEATEDLY (REPEATEDLY!!!) that finally got them interested in doing a sleep study and bingo, bongo, bonzo... severe sleep apnea with multiple apnea events and so many hypopnea events that I never really got to L4 or REM sleep in 40 years. I am one of the lucky ones. I live to tell the tale. I just wish I had demanded a copy of my sleep study... I do remember that it was very colourful though. And then the idiot prescribes me a CPAP with a pressure of 4.0.... ooops, calls me two weeks later and says that should be 9.8 and I have to go back to MediGas to have it changed (today of course, we can change the pressure ourselves on most machines if we know the secret handshake and have the clinician manual).
Once you suspect OSA (snoring is a great indicator as are night sweats if you are not menopausal) it is time to get things into high gear and become very proactive in your own health care; ditto if you suspect heart or other issues. Was at a seminar Thursday and one of the women was having a heart attack a year ago and the only symptoms were severe pains in the hands, incredibly. Her daughter, a nurse, just picked up the phone and dialled 911 against her mother's protests, likely saving her life. Know the signs of stroke and heart attack as that is what is likely to kill you. Of course, if you sleep through your own passing they will write on your headstone "Died peacefully in his sleep". Little did they know. OSA kills.
Funny thing is that they sent me home without a word about sleep apnea.... it was after discharge from hospital without so much as a handshake that we took the rounds of cardiologist, respirologists, etc., in an attempt to be my own advocate for my own life and health. And even then they were getting it wrong and not really being aggressive in my diagnosis and treatment. It was the mention of the snoring and night sweats REPEATEDLY (REPEATEDLY!!!) that finally got them interested in doing a sleep study and bingo, bongo, bonzo... severe sleep apnea with multiple apnea events and so many hypopnea events that I never really got to L4 or REM sleep in 40 years. I am one of the lucky ones. I live to tell the tale. I just wish I had demanded a copy of my sleep study... I do remember that it was very colourful though. And then the idiot prescribes me a CPAP with a pressure of 4.0.... ooops, calls me two weeks later and says that should be 9.8 and I have to go back to MediGas to have it changed (today of course, we can change the pressure ourselves on most machines if we know the secret handshake and have the clinician manual).
Once you suspect OSA (snoring is a great indicator as are night sweats if you are not menopausal) it is time to get things into high gear and become very proactive in your own health care; ditto if you suspect heart or other issues. Was at a seminar Thursday and one of the women was having a heart attack a year ago and the only symptoms were severe pains in the hands, incredibly. Her daughter, a nurse, just picked up the phone and dialled 911 against her mother's protests, likely saving her life. Know the signs of stroke and heart attack as that is what is likely to kill you. Of course, if you sleep through your own passing they will write on your headstone "Died peacefully in his sleep". Little did they know. OSA kills.
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Respironics Everflo Q infusing O2 into APAP line to maintain 95% SaO2; MaxTec Maxflo2 Oxygen Analyzer; Contec CMS50E Recording Pulse Oxymeter |
Fall colours. One of God's gifts. Life is fragile and short, savour every moment no matter what your problems may be. These stunning fall colours from my first outing after surviving a month on life support due to H1N1.
Re: AHI and blood oxgen saturation
Kelingdun.........
It helps if you keep in mind that OSA is simply "on-going suffocation". Suffocation is O2 blood saturation levels not sufficient to sustain life.
The O2 saturation level most people believe to be sufficient is 93%. My wife and I are both hoseheads....and we find that our AHI has to be below 2.5 or we have trouble maintaining a 93% O2 saturation level. Our experience contradicts the opinion (in the medical field) that an AHI below 5.0 is OK. We believe it should be below 2.5.
It helps to have a data capable CPAP machine with good reporting software....along with a recording Oximeter with good reporting software. By watching your AHI daily....and periodically wearing a recording Oximeter all night (just to double-check your CPAP effectiveness), you can do an excellent job of managing your condition.
What I am suggesting is FAR, FAR better than depending on a sleep doctor to tell you what to do. No one can manage your care better than you can do for yourself.
Gerald
It helps if you keep in mind that OSA is simply "on-going suffocation". Suffocation is O2 blood saturation levels not sufficient to sustain life.
The O2 saturation level most people believe to be sufficient is 93%. My wife and I are both hoseheads....and we find that our AHI has to be below 2.5 or we have trouble maintaining a 93% O2 saturation level. Our experience contradicts the opinion (in the medical field) that an AHI below 5.0 is OK. We believe it should be below 2.5.
It helps to have a data capable CPAP machine with good reporting software....along with a recording Oximeter with good reporting software. By watching your AHI daily....and periodically wearing a recording Oximeter all night (just to double-check your CPAP effectiveness), you can do an excellent job of managing your condition.
What I am suggesting is FAR, FAR better than depending on a sleep doctor to tell you what to do. No one can manage your care better than you can do for yourself.
Gerald
Re: AHI and blood oxgen saturation
This is not in any way a scientific observation. I have used supplimental O2 for 9 days following my turbinate reduction surgery (11 days ago). In the hospital they put me on 3 liters of O2. My wife has a spare oxygen concentrator so I started bleeding O2 into my mask. I started to feel like I finally found the silver bullet. I was beginning to function throughout the day without feeling brain dead or like I was out of energy.
Two nights ago I forgot to turn the oxygen concentrator on. One night without it and my short term memory already started to go. I left a bag of groceries in the shopping cart yesterday. Last night I forgot I did not turn it on. I know that doesn't make sense, but I went to bed thinking I remembered turning it on. I got up this morning to read my card and the oxygen concentrator was turned off. (And I don't think the dog did it.)
I have been waking-up sleepy for the last 2 days, with no energy throughout the day. This afternoon I spent almost 2 hours looking for a tube of silicone glue that was on my desk, 18" in front of me. My short-term memory is shot. I turned the oxygen concentrator on around 4 pm, fearing I would forget to turn it on again tonight.
It just happened that I had a follow-up appointment with the sleep doc 2 days after my surgery (after 2 nights on O2). He scheduled a sleep study to see if I really need supplimental oxygen. In the meantime, I have been studying my original sleep study and ResScan reports in an attempt to find the reason the O2 is making me feel so much better. In the Therapy PSG Results section it indicates my Mean Sleep SaO2 was 93% and my Lowest Sleep SaO2 was 90%. And I am totally freaking out the new sleep study will indicate I do not need supplimental O2.
Two nights ago I forgot to turn the oxygen concentrator on. One night without it and my short term memory already started to go. I left a bag of groceries in the shopping cart yesterday. Last night I forgot I did not turn it on. I know that doesn't make sense, but I went to bed thinking I remembered turning it on. I got up this morning to read my card and the oxygen concentrator was turned off. (And I don't think the dog did it.)
I have been waking-up sleepy for the last 2 days, with no energy throughout the day. This afternoon I spent almost 2 hours looking for a tube of silicone glue that was on my desk, 18" in front of me. My short-term memory is shot. I turned the oxygen concentrator on around 4 pm, fearing I would forget to turn it on again tonight.
It just happened that I had a follow-up appointment with the sleep doc 2 days after my surgery (after 2 nights on O2). He scheduled a sleep study to see if I really need supplimental oxygen. In the meantime, I have been studying my original sleep study and ResScan reports in an attempt to find the reason the O2 is making me feel so much better. In the Therapy PSG Results section it indicates my Mean Sleep SaO2 was 93% and my Lowest Sleep SaO2 was 90%. And I am totally freaking out the new sleep study will indicate I do not need supplimental O2.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleep Study 3/16/2010, AHI 25.3, Pressure 6, ResScan 3.10 software |
-
slaaplekker
- Posts: 86
- Joined: Thu May 27, 2010 9:10 pm
Need to buy an Oximeter
You need to get an Oximeter and use it a couple of times a month to see what your O2 sats are doing. My doctor and I discussed doing a follow up overnight Oximetery study at the time he wrote the Rx for APAP. With out a follow up either with an official Oximtery study or with your own Oximeter you really don't know what your O2 levels are doing at night. With and AHI of <1.0 on APAP my O2 sats still were dropping in to the upper 70's.
Because I didn't wait for the Dr. to order the overnight Oximetery study ( bought my own with in a week of starting therap) I was prepared to talk to him about options with in two weeks instead of a month. He had to order and official overnight Oximetery through the sleep lab which came back with recommendation to add 2 liters of O2 bled in to my mask. Now my O2 sats stay >90% all night long. Also noted my heart rate is nice and steady all night long too. No more spikes that correspond to desats.
Here is an example with out additional O2

Here is one after adding the O2

Good luck
John
Because I didn't wait for the Dr. to order the overnight Oximetery study ( bought my own with in a week of starting therap) I was prepared to talk to him about options with in two weeks instead of a month. He had to order and official overnight Oximetery through the sleep lab which came back with recommendation to add 2 liters of O2 bled in to my mask. Now my O2 sats stay >90% all night long. Also noted my heart rate is nice and steady all night long too. No more spikes that correspond to desats.
Here is an example with out additional O2

Here is one after adding the O2

Good luck
John
- torontoCPAPguy
- Posts: 1015
- Joined: Mon Dec 28, 2009 11:27 am
- Location: Toronto Ontario/Buffalo NY
Re: AHI and blood oxgen saturation
Fascinating. One person asks a question and we all learn. I am going to charge up that recording oximeter and see where my SO2 sits during the night these days as I have been having a bit of a rough time in the mornings as of late.
I can tell you this... and I am repeating myself I am sure. In hospital... when I was hooked up to a recording oximeter ALL THE TIME, the alarms were set to go off at 89%. In other words, when I dropped below 89% the doctors and nurses came running! In my fervent desire to get off the damn machines and then the oxygen full face mask I begged and pleaded to have them crank me down. And down. And down. And then I removed the nasal canula's and hung them up. Their response at that point was simply to take my SO2 during the night and if it was under 90ish to poke me and tell me to breathe deeply a few times and up it went.
HOWEVER, like I have said, my main issue today is not so much OSA events (apneas) but more so hypopneas, where my breathing gets so shallow that my SO2 drops and my BP skyrockets putting my heart into rapid beating and my body into a sweat as it works to get oxygen to all the vital parts so my toes don't drop off. I am great during the day... my SO2 is always in the high 90's when I am moving. But as soon as I fall asleep. Bango. Down it goes and now I wonder if some minor supplemental oxygen 'bled' into my mask would not be a good clinical move. I am going to see if I can get my GP or my respirologist on the phone this week and give it a try. It cannot hurt.
At the hospital, by the way, the general feeling I got was that at 3 L. of O2 I was using so little that it was almost negligible. Perhaps this is not true? Well, tonight we start a new project (remember what I said about being your own health care advocate?) ... nightly SO2 graphs on the recording oximeter.
If anyone up here in Canada is in need of a Contec 50E by the way, I ordered two of them by accident and the second one cost me about $170 landed (with the taxes and the handling charge at customs). I would part with it for the same and you save yourself the hassle of bringing it in from Hong Kong or stateside (same difference).
One thing is for certain and that is that a decent recording oximeter is absolutely essential for managing your own treatment. When I walk into my respirologist's office with my graphs and data I can tell you that he is impressed and I get the distinct feeling that my level of care from him is a notch above what Joe Blow walking in totally dumbed out gets. No BS - he knows that I know. And I get the whole works in terms of tests and treatment. It's lovely. Now if I could just do my own EEG and EKG for my cardiologist. (Not an issue with me as long as I take care of everything else).
Thanks for bringing supplemental oxygen to the table. I have no idea what an oxygen concentrator is or if I qualify for one under assitive devices in Ontario or under my insurance but I am going to find out if it might help and if I qualify. Thanks.
I can tell you this... and I am repeating myself I am sure. In hospital... when I was hooked up to a recording oximeter ALL THE TIME, the alarms were set to go off at 89%. In other words, when I dropped below 89% the doctors and nurses came running! In my fervent desire to get off the damn machines and then the oxygen full face mask I begged and pleaded to have them crank me down. And down. And down. And then I removed the nasal canula's and hung them up. Their response at that point was simply to take my SO2 during the night and if it was under 90ish to poke me and tell me to breathe deeply a few times and up it went.
HOWEVER, like I have said, my main issue today is not so much OSA events (apneas) but more so hypopneas, where my breathing gets so shallow that my SO2 drops and my BP skyrockets putting my heart into rapid beating and my body into a sweat as it works to get oxygen to all the vital parts so my toes don't drop off. I am great during the day... my SO2 is always in the high 90's when I am moving. But as soon as I fall asleep. Bango. Down it goes and now I wonder if some minor supplemental oxygen 'bled' into my mask would not be a good clinical move. I am going to see if I can get my GP or my respirologist on the phone this week and give it a try. It cannot hurt.
At the hospital, by the way, the general feeling I got was that at 3 L. of O2 I was using so little that it was almost negligible. Perhaps this is not true? Well, tonight we start a new project (remember what I said about being your own health care advocate?) ... nightly SO2 graphs on the recording oximeter.
If anyone up here in Canada is in need of a Contec 50E by the way, I ordered two of them by accident and the second one cost me about $170 landed (with the taxes and the handling charge at customs). I would part with it for the same and you save yourself the hassle of bringing it in from Hong Kong or stateside (same difference).
One thing is for certain and that is that a decent recording oximeter is absolutely essential for managing your own treatment. When I walk into my respirologist's office with my graphs and data I can tell you that he is impressed and I get the distinct feeling that my level of care from him is a notch above what Joe Blow walking in totally dumbed out gets. No BS - he knows that I know. And I get the whole works in terms of tests and treatment. It's lovely. Now if I could just do my own EEG and EKG for my cardiologist. (Not an issue with me as long as I take care of everything else).
Thanks for bringing supplemental oxygen to the table. I have no idea what an oxygen concentrator is or if I qualify for one under assitive devices in Ontario or under my insurance but I am going to find out if it might help and if I qualify. Thanks.
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Respironics Everflo Q infusing O2 into APAP line to maintain 95% SaO2; MaxTec Maxflo2 Oxygen Analyzer; Contec CMS50E Recording Pulse Oxymeter |
Fall colours. One of God's gifts. Life is fragile and short, savour every moment no matter what your problems may be. These stunning fall colours from my first outing after surviving a month on life support due to H1N1.
- mimi7grands
- Posts: 32
- Joined: Sat Feb 20, 2010 3:34 pm
Re: AHI and blood oxgen saturation
Good info on here. My heart rate has been getting pretty low (48 this morning) so I'm wondering if my O2 has been low at night (or in the daytime!) I'll check it out with a pulse oximeter. And keep this info to check back with. Thanks.
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Additional Comments: Couldn't get Windows to run on my Intel Mac. Software on hold until I can. Thanks to all the helpful people on CPAPTalk.com! |
Re: AHI and blood oxgen saturation
thanks slaaplekker and all. I have learned alot and from the experience you all shared in the thread. Yes, I hope we all learned.
You are right. I should invest in a oximeter and monitor that on top of the APAP. I am looking on the internet already.
Will definitely buy one.
You are right. I should invest in a oximeter and monitor that on top of the APAP. I am looking on the internet already.
Will definitely buy one.
Re: AHI and blood oxgen saturation
torontoCPAPguy and others, oxygen concentrators are easy to come by here in the land of snowbirds. You can easily find one for $100 to $200 on Craigslist. The guy I got mine from found it in a Goodwill store. He paid $40 for it and sold it to me for $200.
Repeating yourself does not bother me. I am doing it too. Your experiences are helping me. I asked the nurse to put me on an oximeter in the hospital just because I was afraid of bleeding out in the CPAP mask. The alarms went off before I even dozed-off. I knew about the slow heart rate. The heart doc said it was slow at night, but not slow enough to be bradycardia. So I asked them to turn the alarm set point down to 50 bpm. Then they wound up giving me 3 liters of O2 to keep my oxygen saturation over 90.
I bought a CMS 50D a couple of months ago, but have not installed the software. I'm not sure why, other than I have just not been up to fighting with a computer software installation if I don't absolutely have to.
As I posted, I just haven't had short term memory the last two days. I was sure I remembered to take my medications last night, and was afraid to take them twice. By the time I figured out I didn't take it, it was pretty late and I decided to see what would happen without it. As always, arousals actually arouse me without ambien. I don't know if that makes sense, but without it I wake-up every time I roll over or if my wife turns on her netbook computer. (I do not understand how she functions with only a few hours sleep every night - but that's a subject I dare not bring up with her.) Regardless, after looking at a couple of ResScan reports on "without it" nights, the sleep doc told me not to stop taking it.
The good news is that my leak rate is always zero when I don't take ambien. The bad news is my AHI is always in the 6 to 8 range when I don't take it. So I wound-up not getting much sleep last night. The darned thing is I feel better and more alert this morning with O2, very little sleep and a high AHI than I did the last two mornings with 7 to 8 hours sleep, a low AHI and no O2. I guess I will not be able to find out if the Ambien is affecting my heart rate and O2 levels if I don't install the software...
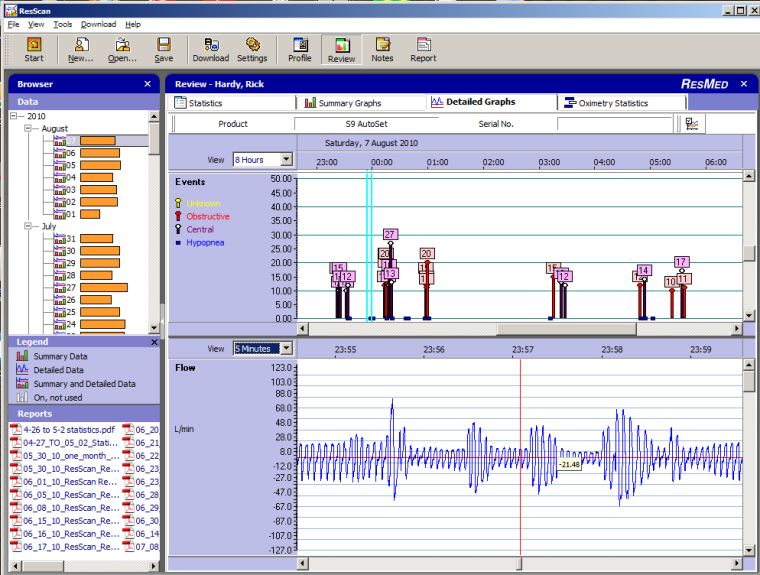
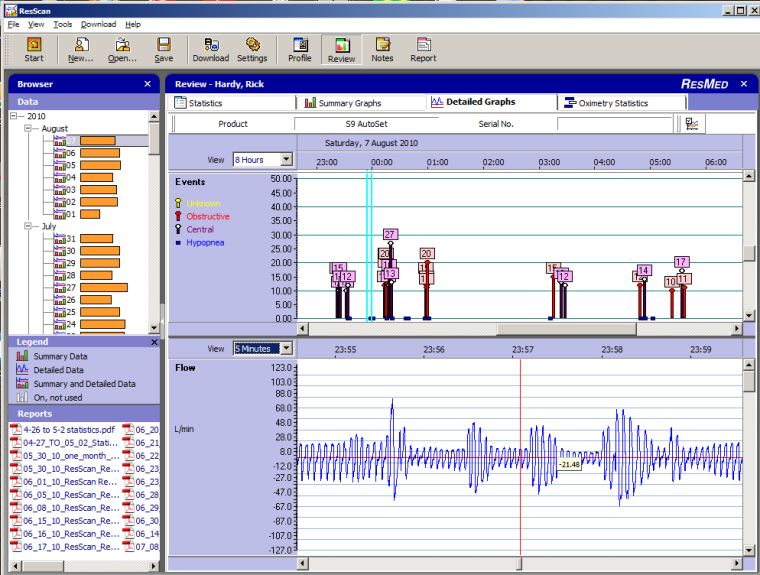
If I am interpeting the Flow graph correctly, the attached photo is showing shallow breathing during a hypopnea. But I seem to have a dozen shallow breathing episodes every night that are not quite shallow enough to register an event. It kind of makes me wonder if CPAP is even the right machine for me.
Unfortunately, everytime I try to turn my pressure up (the last time at the doc's suggestion), I start having centrals and more hypopneas. At my last visit he didn't seem to get that. He got a little mad and told me to stop experimenting when I tried to show him the ResScan reports. Then he said my obsession with the data is not normal and he wants to do another sleep study. I thought I had found a great doc that would work with me. Now I'm kind of afraid the data won't support what I think I am seeing. I do not want to go back to being non-functional just as I am beginning to see some mental clarity returning. Anyway, here's the screenshot:
Repeating yourself does not bother me. I am doing it too. Your experiences are helping me. I asked the nurse to put me on an oximeter in the hospital just because I was afraid of bleeding out in the CPAP mask. The alarms went off before I even dozed-off. I knew about the slow heart rate. The heart doc said it was slow at night, but not slow enough to be bradycardia. So I asked them to turn the alarm set point down to 50 bpm. Then they wound up giving me 3 liters of O2 to keep my oxygen saturation over 90.
I bought a CMS 50D a couple of months ago, but have not installed the software. I'm not sure why, other than I have just not been up to fighting with a computer software installation if I don't absolutely have to.
As I posted, I just haven't had short term memory the last two days. I was sure I remembered to take my medications last night, and was afraid to take them twice. By the time I figured out I didn't take it, it was pretty late and I decided to see what would happen without it. As always, arousals actually arouse me without ambien. I don't know if that makes sense, but without it I wake-up every time I roll over or if my wife turns on her netbook computer. (I do not understand how she functions with only a few hours sleep every night - but that's a subject I dare not bring up with her.) Regardless, after looking at a couple of ResScan reports on "without it" nights, the sleep doc told me not to stop taking it.
The good news is that my leak rate is always zero when I don't take ambien. The bad news is my AHI is always in the 6 to 8 range when I don't take it. So I wound-up not getting much sleep last night. The darned thing is I feel better and more alert this morning with O2, very little sleep and a high AHI than I did the last two mornings with 7 to 8 hours sleep, a low AHI and no O2. I guess I will not be able to find out if the Ambien is affecting my heart rate and O2 levels if I don't install the software...
If I am interpeting the Flow graph correctly, the attached photo is showing shallow breathing during a hypopnea. But I seem to have a dozen shallow breathing episodes every night that are not quite shallow enough to register an event. It kind of makes me wonder if CPAP is even the right machine for me.
Unfortunately, everytime I try to turn my pressure up (the last time at the doc's suggestion), I start having centrals and more hypopneas. At my last visit he didn't seem to get that. He got a little mad and told me to stop experimenting when I tried to show him the ResScan reports. Then he said my obsession with the data is not normal and he wants to do another sleep study. I thought I had found a great doc that would work with me. Now I'm kind of afraid the data won't support what I think I am seeing. I do not want to go back to being non-functional just as I am beginning to see some mental clarity returning. Anyway, here's the screenshot:
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleep Study 3/16/2010, AHI 25.3, Pressure 6, ResScan 3.10 software |
Last edited by frh on Sun Aug 08, 2010 2:08 pm, edited 3 times in total.
- torontoCPAPguy
- Posts: 1015
- Joined: Mon Dec 28, 2009 11:27 am
- Location: Toronto Ontario/Buffalo NY
Re: AHI and blood oxgen saturation
Wow, that's a LOT of events compared to what I am generally getting, which is perhaps one OSA event (apnea) during the night and at most a half dozen hypopnea events (usually two or three) while under therapy with my S9 Auto set to 11.8 - 15 cmH2O. I am puzzled that my S8 Autoset II and my S9 Auto may be reading differently and that the lower numbers are a result of ResMed's attempt to battle the rest of the loosey goosey machines on the market - do they read differently?
I am going to post last night's oximetry recording with an explanation of how poorly the night went in a few minutes.
I am going to post last night's oximetry recording with an explanation of how poorly the night went in a few minutes.
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Respironics Everflo Q infusing O2 into APAP line to maintain 95% SaO2; MaxTec Maxflo2 Oxygen Analyzer; Contec CMS50E Recording Pulse Oxymeter |
Fall colours. One of God's gifts. Life is fragile and short, savour every moment no matter what your problems may be. These stunning fall colours from my first outing after surviving a month on life support due to H1N1.
Re: AHI and blood oxgen saturation
Guys
I have a question.....
When I went for my first pulmanory test last Nov. the tech said my oxygen levels were at 76. When I had my overnight sleep lab tests in Feb. the tech said my levels went down to 72 at one point. About a month later I was at my doctors office and I was at 96, again a few weeks later and I was at 93. He said those numbers (the 90's) were good and my cpap machine has leveled me off. Was he right?
Nan
I have a question.....
When I went for my first pulmanory test last Nov. the tech said my oxygen levels were at 76. When I had my overnight sleep lab tests in Feb. the tech said my levels went down to 72 at one point. About a month later I was at my doctors office and I was at 96, again a few weeks later and I was at 93. He said those numbers (the 90's) were good and my cpap machine has leveled me off. Was he right?
Nan
_________________
| Machine: ResMed AirSense™ 10 AutoSet™ CPAP Machine with HumidAir™ Heated Humidifier |
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
Started cpap in 2010.. still at it with great results.
Re: AHI and blood oxgen saturation
Nan.......
Your "doctor" measured your O2 in his office...during the daytime....while you were awake?
And your sleep tech measured your O2 while you were asleep?
And your "doctor" says that you're just fine?.......and that your CPAP machine is doing its job?
Sounds to me like your "doctor" is a poor mechanic....and he has no common sense.
You need to measure your O2 during the night....while you're asleep....not during the day while you're sitting in your "doctor's" office.
Purchase your own Oximeter....take charge of your own therapy....before your "doctor" kills you.....or, at least, shortens your life.
Gerald
Your "doctor" measured your O2 in his office...during the daytime....while you were awake?
And your sleep tech measured your O2 while you were asleep?
And your "doctor" says that you're just fine?.......and that your CPAP machine is doing its job?
Sounds to me like your "doctor" is a poor mechanic....and he has no common sense.
You need to measure your O2 during the night....while you're asleep....not during the day while you're sitting in your "doctor's" office.
Purchase your own Oximeter....take charge of your own therapy....before your "doctor" kills you.....or, at least, shortens your life.
Gerald
-
slaaplekker
- Posts: 86
- Joined: Thu May 27, 2010 9:10 pm
Over Night Oximetery
Sometimes I can't believe some of the things that I hear that Drs have told people. Totally amazing that anyone with at least a bit of knowledge and supposedly a logical thinker since they survived a lot of schooling and passed a lot of tests would say that a single reading during the day in a Drs office was at all useful information about how CPAP therapy was working. That single reading is useful for screening for COPD, Pneumonia and those types of chronic or acute problems, but even then it is a screening test, if it is positive (in this case I mean low O2) it is useful information if it is negative (meaning normal O2) it doesn't mean that you don't have a problem since it is a single point in time. Your O2 saturation could be come abnormal when you exercise, watch TV and yes when you sleep even on CPAP/APAP/BiPAP therapy. Sitting in the Dr's office in an upright position, probably a little anxious means that your O2 saturation better be normal because if it isn't you most likely have a serious condition other than Sleep Apnea, but it is not going to give you the least bit of information about your serious Sleep Apena condition.nanwilson wrote: He said those numbers (the 90's) were good and my cpap machine has leveled me off. Was he right?
My son in law is in his 3rd year of medical school, and if he said anything as silly as what your doctor told you I would tell him to quit now and become an accountant
I'm starting a new thread on the importance of Overnight Oximetery this since this is likely to end up being buried you can see the rest of my thoughts in that thread.
Good Luck
John












