Question for those who had Inferior Turbinate Reduction surg
Question for those who had Inferior Turbinate Reduction surg
My surgery will be Monday morning (July 26th) in the hospital. They plan to keep me overnight because of my OSA. The doctor said I will not be using CPAP for a few days (or was it a week?). But in my pre-surgery interview, they told me to bring the machine and my Mirage Quattro mask.
A video of the surgery I will be having is at http://www.youtube.com/watch?v=WNb_w1sv8sA, although the doctor told me she would be removing tissue from both sides of the bone.
I stopped taking Nasonex a couple of days ago because I thought if the turbinates were a little swollen, she would be able to see what she is doing a little better. (I should have asked the doctor about this, but didn't.)
I feel like I am starting to be a little more congested, but it might just be morning rebound from the CPAP machine's humidity. (After all, It took over a week for the Nasonex to start working in the first place.) Now I am also having 2nd thoughts about discontinuing the nasal steroids (or perhaps it is just a little pre-surgery paranoia).
Would it be better to have the surgery when the turbinates are a little swollen (if that's what they are doing?)? Or should I resume the Nasonex today and tomorrow?
A video of the surgery I will be having is at http://www.youtube.com/watch?v=WNb_w1sv8sA, although the doctor told me she would be removing tissue from both sides of the bone.
I stopped taking Nasonex a couple of days ago because I thought if the turbinates were a little swollen, she would be able to see what she is doing a little better. (I should have asked the doctor about this, but didn't.)
I feel like I am starting to be a little more congested, but it might just be morning rebound from the CPAP machine's humidity. (After all, It took over a week for the Nasonex to start working in the first place.) Now I am also having 2nd thoughts about discontinuing the nasal steroids (or perhaps it is just a little pre-surgery paranoia).
Would it be better to have the surgery when the turbinates are a little swollen (if that's what they are doing?)? Or should I resume the Nasonex today and tomorrow?
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleep Study 3/16/2010, AHI 25.3, Pressure 6, ResScan 3.10 software |
Re: Question for those who had Inferior Turbinate Reduction surg
I can't answer the question. The subject never came up with my surgeon and he knew I was, from time to time, using the sprays he had prescribed.
If it were me, I would continue using them because, intuitively, it sounds better to be cutting on healthy tissue instead of inflamed tissue.
BTW, I never missed a night of CPAP. I switched to my traditional FFM because the nasal pillows of the Hybrid mask seemed problematic until the surgery healed.
I had two hours of intense throat pain in the recovery room that was only relieved after a shot of morphine. I assumed the pain was from rough handling of the intubation tube and so questioned the anesthesiologist when he came to check on me. He denied it and said it was from blood dripping into the throat. Whatever.
In any case, the techniques they now use for this surgery are excellent and you will likely do very well. In some weeks, you will be enjoying the new freeway through your nostils.
Maybe this is what happened to my throat:
If it were me, I would continue using them because, intuitively, it sounds better to be cutting on healthy tissue instead of inflamed tissue.
BTW, I never missed a night of CPAP. I switched to my traditional FFM because the nasal pillows of the Hybrid mask seemed problematic until the surgery healed.
I had two hours of intense throat pain in the recovery room that was only relieved after a shot of morphine. I assumed the pain was from rough handling of the intubation tube and so questioned the anesthesiologist when he came to check on me. He denied it and said it was from blood dripping into the throat. Whatever.
In any case, the techniques they now use for this surgery are excellent and you will likely do very well. In some weeks, you will be enjoying the new freeway through your nostils.
Maybe this is what happened to my throat:
I any case it was all worth it. My freeway should be good for life.What the anesthesiologists will tell you is: Open the mouth. If you're using the Macintosh (curved) blade, sweep the tongue out of the way, stick the tip of the blade into the vallecula, lift the structures up and toward the far corner of the room, visualize the cords and stick the tube between the cords (seeFigure 1 at the top of the page).
What you'll actually do is: Open the mouth, stick the blade in, lift up and not see a darn thing except a bunch of useless, confusing, pink tissue. In my case, I thought,Maybe I should lift harder. So you'll strain and strain and strain, giving some poor patient a whopping soar throat and not end up any closer to the cords.
The anesthesiologist will also say, ˙All right, come out.Ó He'll take one peek and snake it down there while you stand around like an idiot (and the surgeon might even say something like, ˙What an idiot!Ó).
http://www.jems.com/article/patient-car ... do-what-ca
Rooster
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
Re: Question for those who had Inferior Turbinate Reduction surg
roster wrote:I any case it was all worth it. My freeway should be good for life.
Thanks for your response and encouragement Roster. I really hope it opens up my "nasal freeway", and I don't wind-up being sorry I had it done. You touched on the idea of healthy tissue vs inflamed tissue. One of the things that concerned me is the possibility the nasal steroids dry out and shrink the tissue in a way that is not natural, and that might adversely affect the outcome.
I am also concerned about CPAP not working for me until my nose is completely healed. Truth is, I am not sure wearing a full face mask is much better than just not using the CPAP machine (at least for me). Don't get me wrong, I haven't missed a night since I got the machine at the end of March. But every time I wear the Mirage Quattro mask I wake-up tired, have a high AHI, and the reports (and my wife) tell me I snore when wearing it.
I am sorry to hear that you woke with a sore throat. Last month I had an endoscopy and had absolutely no soreness from it. My wife had the same procedure a couple of weeks later. They had a hard time getting the IV in her and were running aout an hour late. She woke-up with a swollen upper lip and her throat was really sore for a couple of weeks. If I could have been in the room when she had it done, I probably would have wanted to beat the hell out of the doc for being so brutal with her.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleep Study 3/16/2010, AHI 25.3, Pressure 6, ResScan 3.10 software |
-
giving up
Re: Question for those who had Inferior Turbinate Reduction surg
I had the surgery in march of this year and never missed a night of c-pap. I just switched to FFM because i couldn't breathe through my nose. no other problems.
Re: Question for those who had Inferior Turbinate Reduction surg
frh wrote:
I am also concerned about CPAP not working for me until my nose is completely healed. Truth is, I am not sure wearing a full face mask is much better than just not using the CPAP machine (at least for me).
Have you evaluated yourself for positional sleep apnea (PSA = condition is much less severe when sleeping on sides or tummy)? What did your sleep studies say about PSA?
frh wrote:
Don't get me wrong, I haven't missed a night since I got the machine at the end of March. But every time I wear the Mirage Quattro mask I wake-up tired, have a high AHI, and the reports (and my wife) tell me I snore when wearing it.
What is the leak rate? What was your titrated pressure?
Your profile shows 6 cm which is a very low pressure. Are you running straight CPAP?
Snoring, fatigue and high AHI point to significant leaks and/or pressure too low.
Rooster
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
Re: Question for those who had Inferior Turbinate Reduction surg
Roster, I sent a PM with a link to my sleep study.
My sleep study said I slept in a "supine" position. If you take a look at the times / amount of sleep reported on the study, it doesn't really add up. Regardless, I usually fall asleep and wake-up on my side. I tape the mask to my face and would really have to tug / push on it to make it leak when I am awake. The ResScan graphs show leaks about an hour apart while I am sleeping that could only be caused by flopping over / burying the mask in my pillow in my sleep.
Last month I turned my machine to my titrated pressure of 6 for about 2 weeks prior to an appointment with my new sleep doc. He told me to turn my pressure to 10 with EPR at 3, but I started having centrals so I turned it back down to 8 with EPR at 2. Last night I turned the pressure down from 8 to 7, and EPR down from 2 to 1 and slept for 8.01 hours. Truth is, I feel like my numbers are better at 6.
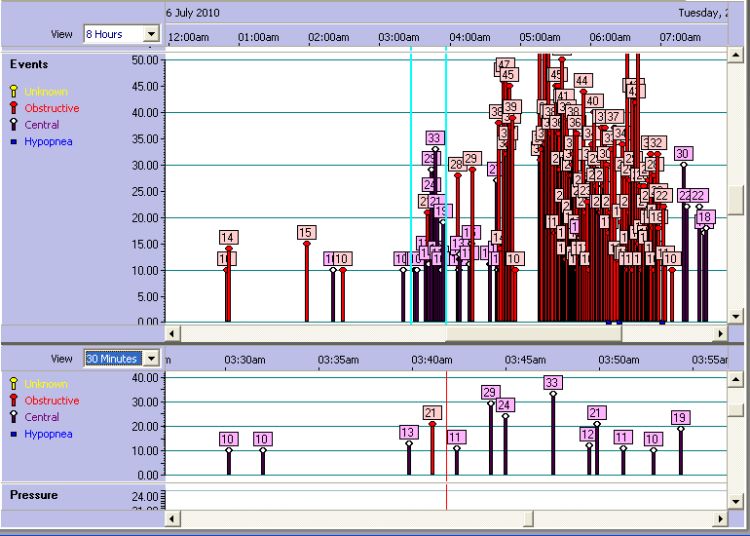
Normally I don't wake-up in my sleep, but last night I drank a 32 ounce glass of iced tea about an hour before I went to bed. I woke to use the bathroom about 3 am. Then my wife woke me again around 5 am when she turned the TV on. After that I drifted in and out of sleep and finally got up at 7 am.
Last night my median leak (with the Swift FX mask) was 0.0, my 95th Percentile leak was 16.8 and my Maximum leak was 22.8. My AHI was 5.1, and Centrals were reported at 2.8. A manual count shows 6 leaks over 10, roughly an hour apart, with the last one occurring between 5:30 and 6 am I had relatively few events before 6 am, but a manual count of the events on the graph between 6 and 7 am showed I had 4 Obstructive events, 17 Centrals, and 4 Hypopneas. That doesn't really seem strange to me, because I often find myself forgetting to inhale during the day.
My sleep study said I slept in a "supine" position. If you take a look at the times / amount of sleep reported on the study, it doesn't really add up. Regardless, I usually fall asleep and wake-up on my side. I tape the mask to my face and would really have to tug / push on it to make it leak when I am awake. The ResScan graphs show leaks about an hour apart while I am sleeping that could only be caused by flopping over / burying the mask in my pillow in my sleep.
Last month I turned my machine to my titrated pressure of 6 for about 2 weeks prior to an appointment with my new sleep doc. He told me to turn my pressure to 10 with EPR at 3, but I started having centrals so I turned it back down to 8 with EPR at 2. Last night I turned the pressure down from 8 to 7, and EPR down from 2 to 1 and slept for 8.01 hours. Truth is, I feel like my numbers are better at 6.
Normally I don't wake-up in my sleep, but last night I drank a 32 ounce glass of iced tea about an hour before I went to bed. I woke to use the bathroom about 3 am. Then my wife woke me again around 5 am when she turned the TV on. After that I drifted in and out of sleep and finally got up at 7 am.
Last night my median leak (with the Swift FX mask) was 0.0, my 95th Percentile leak was 16.8 and my Maximum leak was 22.8. My AHI was 5.1, and Centrals were reported at 2.8. A manual count shows 6 leaks over 10, roughly an hour apart, with the last one occurring between 5:30 and 6 am I had relatively few events before 6 am, but a manual count of the events on the graph between 6 and 7 am showed I had 4 Obstructive events, 17 Centrals, and 4 Hypopneas. That doesn't really seem strange to me, because I often find myself forgetting to inhale during the day.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleep Study 3/16/2010, AHI 25.3, Pressure 6, ResScan 3.10 software |
Last edited by frh on Sat Jul 24, 2010 9:20 pm, edited 2 times in total.
Re: Question for those who had Inferior Turbinate Reduction surg
I had turbinate reduction (among other things) last april. Prior to that I knew I had OSA but wasn't official diagnosed, nor on CPAP...in any event...both of my nostrils where packed with gauze and dissolvable packing (aka silly string). For me there wasn't any air coming in or out of my nose.
Re: Question for those who had Inferior Turbinate Reduction surg
frh wrote:Roster, I sent a PM with a link to my sleep study.
My sleep study said I slept in a "supine" position. If you take a look at the times / amount of sleep reported on the study, it doesn't really add up. Regardless, I usually fall asleep and wake-up on my side. I tape the mask to my face and would really have to tug / push on it to make it leak when I am awake. The ResScan graphs show leaks about an hour apart while I am sleeping that could only be caused by flopping over / burying the mask in my pillow in my sleep.
Last month I turned my machine to my titrated pressure of 6 for about 2 weeks prior to an appointment with my new sleep doc. He told me to turn my pressure to 10 with EPR at 3, but I started having centrals so I turned it back down to 8 with EPR at 2. Last night I turned the pressure down from 8 to 7, and EPR down from 2 to 1 and slept for 8.01 hours. Truth is, I feel like my numbers are better at 6.
Normally I don't wake-up in my sleep, but last night I drank a 32 ounce glass of iced tea about an hour before I went to bed. I woke to use the bathroom about 3 am. Then my wife woke me again around 5 am when she turned the TV on. After that I drifted in and out of sleep and finally got up at 7 am.
Last night my median leak (with the Swift FX mask) was 0.0, my 95th Percentile leak was 16.8 and my Maximum leak was 22.8. My AHI was 5.1, and Centrals were reported at 2.8. A manual count shows 6 leaks over 10, roughly an hour apart, with the last one occurring between 5:30 and 6 am I had relatively few events before 6 am, but a manual count of the events on the graph between 6 and 7 am showed I had 4 Obstructive events, 17 Centrals, and 4 Hypopneas. That doesn't really seem strange to me, because I often find myself forgetting to inhale during the day.
One thing you need to do is quit caffeine entirely. This includes chocolate and decaffeinated tea and coffee.
Recent studies on college students illustrate the importance of this. Students were interviewed before undergoing PSGs. Some said caffeine bothered their sleep and others said it had no effect and they could sleep soundly all night with caffeine in their system. The PSGs for the second group showed something different. Caffeine had a pronounced negative effect on their sleep architecture despite their reports the next morning saying they slept well.
If you are used to drinking a lot of caffeine, it is best to taper off gradually to avoid withdrawal effects which are primarily headaches.
Your sleep study postings are difficult to read.
Rooster
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
Re: Question for those who had Inferior Turbinate Reduction surg
If you're having turbinate reduction, your turbinates are too big even when not swollen, so the doc won't have any trouble seeing them. Also, they're putting magnifying/TV lenses up there.
I agree with Rooster that healthy tissue is better to operate on. They actually use Afrin before surgery to reduce bleeding, too. Good luck! I'll be having this surgery in September.
I agree with Rooster that healthy tissue is better to operate on. They actually use Afrin before surgery to reduce bleeding, too. Good luck! I'll be having this surgery in September.
Re: Question for those who had Inferior Turbinate Reduction surg
roster wrote:One thing you need to do is quit caffeine entirely. This includes chocolate and decaffeinated tea and coffee.
Rooster, I have to admit I order iced tea if I am not eating at home (like at lunch today). Since my wife keeps it in the fridge, every few days I drink about a half can of coke. As far as coffee goes, I don't even like the smell of it. Oh, and I prefer root beer to real beer. Instead of eating candy bars, I often give myself permission to eat 4 hershey kisses (I like the cherry filled ones) or a small handful of peanut m&m's before bed.
Unfortunately, my wife nags me about putting salt on my food, but I make up for it by occasionally eating salted peanuts or sunflower seeds.
I could be putting a lot of worse things in my body.
Back to the original subject. After 3 or 4 days of not using Nasonex, I am still breathing through my nose OK.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleep Study 3/16/2010, AHI 25.3, Pressure 6, ResScan 3.10 software |
Re: Question for those who had Inferior Turbinate Reduction surg
I had turbinate reduction 8 weeks ago among other surgeries and was advised to stop the Nasonex pre-op. Post-op I restarted the Nasonex at week 7 when mostly healed due to allergies. When I restarted it, I was told to do a nasal rinse first and it's working well for me. I can breathe much better out of my nose now. Key for my healing was regular saline rinses (hourly at times) followed by antibiotic ointment. And no nose blowing! Ask your Dr. if it's ok to use a Neti Pot - it really helped me.
BTW: You get much more salt/sodium from processed, packaged, and restaurant foods (read labels and see restaurant websites for sodium content) than you get from an occasional salted nut or sunflower seed
BTW: You get much more salt/sodium from processed, packaged, and restaurant foods (read labels and see restaurant websites for sodium content) than you get from an occasional salted nut or sunflower seed
Re: Question for those who had Inferior Turbinate Reduction surg
frh wrote:
Rooster, I have to admit I order iced tea if I am not eating at home (like at lunch today).
Also don't get too excited about decaffeinated tea or coffee. One of my kayaking buddies/fellow CPAPer and I have discovered the small amount of caffeine in these beverages has a significant deleterious effects on our sleep.
Damn, this southerner misses iced tea!
Rooster
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
Re: Question for those who had Inferior Turbinate Reduction surg
My surgery was done yesterday morning. I woke with a bit of a sore throat. The Anesthesiologist was in his mid 50's and looked like he has done it many thousands of times. After I woke in the recovery room, the nurse apologized for the sore throat and told me she did it with the suction tube. The ENT put a little tubes about 3/8" up inside my nostrils. They were annoying, but did not prevent drainage. She pulled them out out just before she discharged me this morning.
I woke wearing a surgical mask that had been jury rigged as a holder for a large folded gauze pad under my nose. It was more annoying than the sore throat and seemed like massive overkill. They out compression stockings some kind of pressure cuffs on my legs before surgery. After surgery they kept filling with air and releasing. The day shift nurse was totally opposed to allowing me take them off. After I used the rest room he forgot to plug them back in, so I ripped them off. I don't believe I got the pulmonary embolism he warned me about. Same thing with the surgical mask gauze holder. After I took it off, I went through 4 boxes of kleenex in 6 hours.
The bleeding seemed to slow down just before midnight. The night shift nurse helped me fashion a pad out of a small gauze square folded into thirds with a strip of waterproof tape holding it under my nose. After 1/2 hour it seemed to be working OK. I sat in a chair wearing the Mirage Quattro mask for about 1/2 hour. The pressure helped control the drainage pretty well, but I was still concerned about waking (or not waking) with a bloody mess inside the mask. I asked them to hook me up to an oximeter before going to bed. I figured if anything went wrong, the alarm would go off.
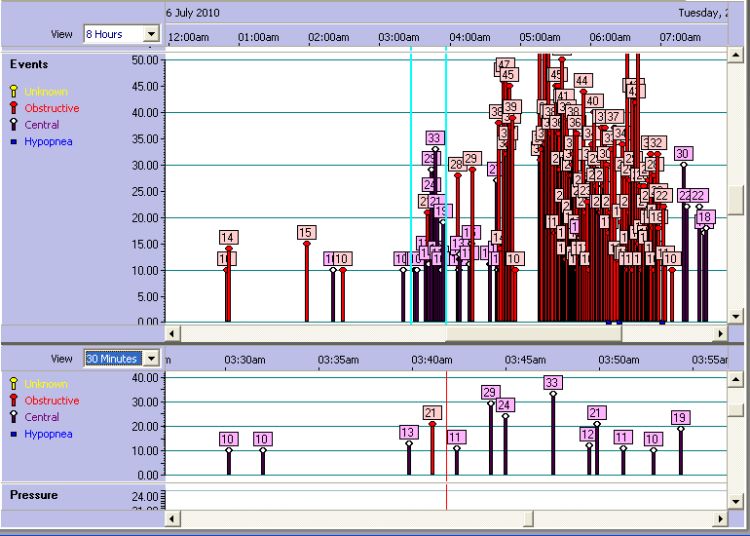
I took half of an ambien sleeping pill because I didn't want to be so asleep I couldn't wake if something went wrong. Sure enough, the alarm went-off as soon as I got to sleep. My heart rate had dropped to 54 and my oxygen level dropped to 86. The nurse had the hospital RT bring an oxygen adapter for my hose and hooked me up to 2 litres of 02. And the alarm kept going off until they finally raised it to 3 litres and lowered the heart rate alarm set point to 50. The detail graph shows I disconnected the hose 12 times between 12:30 and 7:30 am (mostly to alert the nurse when the alarm went off). So I got very little sleep.
The back of my throat is still a little sore and feels swollen when I swallow. I can breathe through my nose, but it's making gurgling sounds. The ENT warned me not to try to blow it, even gently. She told me to gently rinse with a saline spray or netti pot to get some of the dried blood out over the weekend and she wants me to see her on Monday.
Here's the weird part. I had 5.4 hours mask time and my AHI was 29.6 (Central: 7.5), but I feel reasonably rested. I plan to raise my pressure from 7 to 8, turn EPR from 1 to 0, and hook my Quattro mask to my wife's spare oxygen concentrator tonight (at 2.5 litres). And if I can get the software installed on the laptop, I plan to wear the CMS 50D recording oximeter tonight.
Oh, and I have a follow-up appointment with the sleep doc tomorrow.
Here's a screenshot of last night:
I woke wearing a surgical mask that had been jury rigged as a holder for a large folded gauze pad under my nose. It was more annoying than the sore throat and seemed like massive overkill. They out compression stockings some kind of pressure cuffs on my legs before surgery. After surgery they kept filling with air and releasing. The day shift nurse was totally opposed to allowing me take them off. After I used the rest room he forgot to plug them back in, so I ripped them off. I don't believe I got the pulmonary embolism he warned me about. Same thing with the surgical mask gauze holder. After I took it off, I went through 4 boxes of kleenex in 6 hours.
The bleeding seemed to slow down just before midnight. The night shift nurse helped me fashion a pad out of a small gauze square folded into thirds with a strip of waterproof tape holding it under my nose. After 1/2 hour it seemed to be working OK. I sat in a chair wearing the Mirage Quattro mask for about 1/2 hour. The pressure helped control the drainage pretty well, but I was still concerned about waking (or not waking) with a bloody mess inside the mask. I asked them to hook me up to an oximeter before going to bed. I figured if anything went wrong, the alarm would go off.
I took half of an ambien sleeping pill because I didn't want to be so asleep I couldn't wake if something went wrong. Sure enough, the alarm went-off as soon as I got to sleep. My heart rate had dropped to 54 and my oxygen level dropped to 86. The nurse had the hospital RT bring an oxygen adapter for my hose and hooked me up to 2 litres of 02. And the alarm kept going off until they finally raised it to 3 litres and lowered the heart rate alarm set point to 50. The detail graph shows I disconnected the hose 12 times between 12:30 and 7:30 am (mostly to alert the nurse when the alarm went off). So I got very little sleep.
The back of my throat is still a little sore and feels swollen when I swallow. I can breathe through my nose, but it's making gurgling sounds. The ENT warned me not to try to blow it, even gently. She told me to gently rinse with a saline spray or netti pot to get some of the dried blood out over the weekend and she wants me to see her on Monday.
Here's the weird part. I had 5.4 hours mask time and my AHI was 29.6 (Central: 7.5), but I feel reasonably rested. I plan to raise my pressure from 7 to 8, turn EPR from 1 to 0, and hook my Quattro mask to my wife's spare oxygen concentrator tonight (at 2.5 litres). And if I can get the software installed on the laptop, I plan to wear the CMS 50D recording oximeter tonight.
Oh, and I have a follow-up appointment with the sleep doc tomorrow.
Here's a screenshot of last night:
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleep Study 3/16/2010, AHI 25.3, Pressure 6, ResScan 3.10 software |
Re: Question for those who had Inferior Turbinate Reduction surg
Hopefully the worst is behind you. We forgot to tell you about that "mustache" bandage to catch the dripping blood. I wore one for three days but it was more for my wife's benefit than mine.
For a couple of mornings I woke with a little pool of dried blood in my mask. Just washed it out and kept on going.
Despite all the apneas, you may feel good due to the supplemental O2. When you discontinue it at home, how about letting us know how you feel the next morning?
Sounds like as soon as they take the tubes out of your nostrils you will be set. i imagine they will take them out later this week.
For a couple of mornings I woke with a little pool of dried blood in my mask. Just washed it out and kept on going.
Despite all the apneas, you may feel good due to the supplemental O2. When you discontinue it at home, how about letting us know how you feel the next morning?
Sounds like as soon as they take the tubes out of your nostrils you will be set. i imagine they will take them out later this week.
Rooster
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
I have a vision that we will figure out an easy way to ensure that children develop wide, deep, healthy and attractive jaws and then obstructive sleep apnea becomes an obscure bit of history.https://www.youtube.com/watch?v=0ycw4uaX ... re=related
Re: Question for those who had Inferior Turbinate Reduction surg
Rooster, the doc took the tubes out this morning before they discharged me from the hospital. I was surprised that it did not start a lot of blood flow or hurt when she stuck the tweezers in and pulled them out. I am encouraged that the discharge from my nose and throat is already starting to look a bit more like snot than blood. I took the bandage off about a half hour ago and probably won't need a new one until it's time to put on the mask.
I know from wearing the heart monitor for 3 weeks that my heart rate slows down at night. It really surprised me that my O2 went so low it took 3 liters to keep the alarm from going off. We found the oxygen concentrator on craigslist really cheap and bought it as a backup for my wife. Right now it's just sitting there.
I have a bad night every time I wear the FFM anyway. Since the hospital gave me the fitting, I will use it tonight, but I will ask the sleep doc what he thinks about it tomorrow. At my last visit, he pretty much told me he wants to do another sleep study if my ResScan reports don't show a big improvement.
I have also come to suspect that my 4 or 5 leak episodes a night are most likely mouth leaks instead of dislodging the mask as I had thought. The nurse at the hospital gave me a roll of tape that I think might work as soon as I can get back to the nasal mask. (The doc told me not to use the nasal mask until I see her on Monday.)
If you are willing to look at it, I could email you a high resolution pdf of my original sleep study document. Thanks
I know from wearing the heart monitor for 3 weeks that my heart rate slows down at night. It really surprised me that my O2 went so low it took 3 liters to keep the alarm from going off. We found the oxygen concentrator on craigslist really cheap and bought it as a backup for my wife. Right now it's just sitting there.
I have a bad night every time I wear the FFM anyway. Since the hospital gave me the fitting, I will use it tonight, but I will ask the sleep doc what he thinks about it tomorrow. At my last visit, he pretty much told me he wants to do another sleep study if my ResScan reports don't show a big improvement.
I have also come to suspect that my 4 or 5 leak episodes a night are most likely mouth leaks instead of dislodging the mask as I had thought. The nurse at the hospital gave me a roll of tape that I think might work as soon as I can get back to the nasal mask. (The doc told me not to use the nasal mask until I see her on Monday.)
If you are willing to look at it, I could email you a high resolution pdf of my original sleep study document. Thanks
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Sleep Study 3/16/2010, AHI 25.3, Pressure 6, ResScan 3.10 software |









