Rebecca R wrote:I was going to suggest that since it's your thread, you should say a few words, since you've made forum history. You know, something meaningful.
Let's take stock of how things have progressed to this point in time:
1. The original problem that I wanted to fix is EDS and fatigue; I am being treated with 20mg fluoxetine for mild depression and anxiety; I am hypersensitive to touch and sound.
2. After a home PSG I was diagnosed with moderate OSA and assigned to use an Auto-titrating Continuous Positive Airway Pressure (CPAP) machine.
2a. Lacking confidence in the OSA diagnosis, I organised a hospital PSG and took myself off fluoxetine 2 weeks prior to the diagnostic PSG and 4 weeks prior to the titration PSG.
3. After the hospital PSG I was diagnosed with CompSA and PLMs (450/night) and recommended CPAP+/-ASV.
4. I purchased an Adapt SV and commenced treatment with Dr recommending another 6 months on ASV until my breathing stabilised
5. After 6 months already on CPAP I still suffered from mild EDS and fatigue
6. I noticed that I also tended to have hyperventilation (under breathing), bradycardia (slow heart rate) and hypotension (low blood pressure)
7. Hence I posed the question to this forum: "CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?"
7a. Forum members thought that I might have a good case to test for hypothyroidism.
7b. As seen in my daily CPAP logs (DLs), my respiration when asleep under ASV/fixed CPAP is seen to been disordered, unstable, chaotic and minute ventilation under par.
7c. I have unresolved air flow limitation during CPAP use according to my CPAP DLs (-SWS; DSM).
7d. -SWS suggested that my hypersensitivity and anxiety fitted well with Dabrowski's "five overexcitabilities" phenotype (I can relate very much to this).
8. Following an appointment with my (2nd) sleep doctor (D-day) I was told that I was an unusual case (being on ASV at a young age) and that "instability begets instability". Dr thought that my lungs and heart were fine (not interested in tests) and that I could have a blood test if I really wanted to test for hypothyroidism, but he didn't seem too interested in this explanation.
9. My bloods were taken and returned normal values according to the GP (inc. thyroid, iron, RBC, magnesium)
10. I developed joint pain during the course of CPAP use.
11. Since being on CPAP my energy levels and EDS have improved to the point I now better support my wife, play with my kids, and do my job.
12. I obtained my detailed PSG data from the Sleep Centre.
13. On seeing my PSG data, Muffy observed Alpha Wave Intrusion (AWI) in the delta waves of my deeper sleep levels. AWI is not the reason for my respiration instability, but possibly reduces the restorative benefits provided to me during deep sleep.
14. Muffy also pointed out that the centrals seen in my PSG were a normal feature of the transition back to sleep following arousal. So no CSA problem for me.
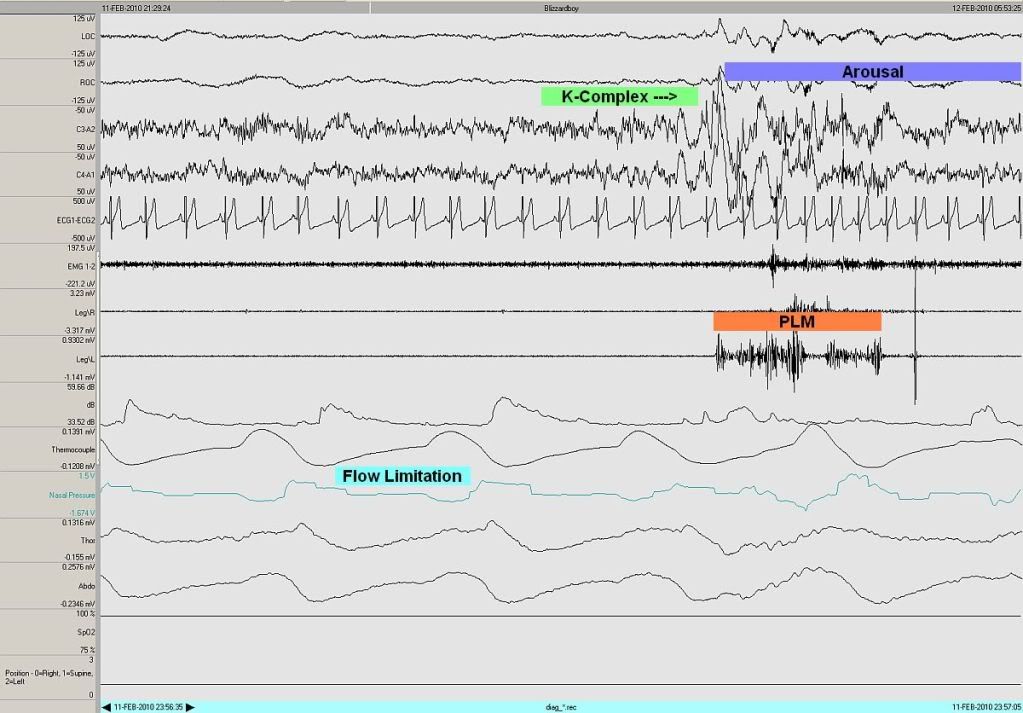
14a. Muffy (kindly) showed us an example of my chaotic breathing during stage 2 NREM from the diagnostic PSG.
14b. Muffy suggested that my PLMs are severe enough to warrant treatment (a point also suspected by kteague).
14c. Muffy saw no evidence for OSA and suggested that I could possibly be a candidate for UARS.
15. The cause of my arousals needs to be ascertained.
15b. No settings on the ASV or fixed CPAP used to date have produced a quick fix (e.g. over a period of one week) to my breathing instability
15c. I also suffer from aerophagia when CPAP gets above about 10cmH2O.
16. Fluoxetine, joint pain, mental illness, higher BMI (currently 26kg/m2), alcohol, caffeine, poor sleep hygiene, UARS, GERD, fibromyalgia (whatever that is ), lowered pCO2 arousal threshold, childhood meningitis and CO2 retention (my idea only ) are possible causes of my arousals
17. I am currently maintaining fluoxetine, getting fit, improving my sleep hygiene, reducing caffeine and alcohol, sleeping on a bed wedge and using ASV (EEP=10, PS=3.8->8.8; my most comfortable settings to date; fairly stable RR). I will stay with these ASV settings for now (no more dial whingin' ).
17a. I aim to wean off fluoxetine once I am physically fit (i.e. good aerobic fitness, increased exercise level, hopefully reduced BMI).
17b. My GP preferred I take Proton Pump Inhibitor (PPI) medication rather than have a GERD diagnostic. I am not currently taking this medication.
17c. I score 18/18 on a fibromyalgia pressure point test and continue to awaken with joint pain in the morning (esp. hands, feet, neck and shoulders)
18. On 23 June I have another appointment with my (3rd, and probably final) sleep doctor during which I will provide my PSG data for review, request (insist on, if I'm brave) a complete PFT, talk about the latest techniques to keep one in deep sleep discussed at the 2010 ATS meeting in New Orleans, PLM treatment, AWI, etc. At the end of the last appointment this Dr concluded that my problems were probably related to mental health issues. I find this explanation hard to accept as I am light years away from where I was a few years ago - my family say I am a new man. Let's see what comes of the next appointment.
19. The journey (battle?) continues...giddy up!
Cheers,
p.s. please let me know any improvements to this list and I will sort it out. Its a fair bit to keep in my mind so I may well have made a whoopsy.