I couldn't agree more. As a physicist I try to look beyond the square to solve complex problems, akin to multidisciplinary medical teams discussing patient cases. I think embracing treatment diversity, if managed well, can provide synergistic benefit in reducing the number of factors that contribute to increased sleep disorder.-SWS wrote:many practitioners...should consider...potential loop-gain catalyst events with diverse proactive management techniques.
CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I'm all for living, so I think that I will adopt the +\- 0.2 cmH2O strategy when the time comes, and only once at a time!dsm wrote:The Resmed ASV allows 0.2 CMs changes & doing just one 0.2 change is normally not any major comfort or life threatening issue.
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
blizzardboy wrote:I'm all for living, so I think that I will adopt the +\- 0.2 cmH2O strategy when the time comes, and only once at a time!dsm wrote:The Resmed ASV allows 0.2 CMs changes & doing just one 0.2 change is normally not any major comfort or life threatening issue.
Good strategy
You appear to be learning very quickly - but isn't it worth every bit.
Cheers
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I see you left off the Feedback component (perhaps the most important contributor to CompSAS):blizzardboy wrote:From the literature and comments provided in this thread by Muffy and -SWS and others, I think I currently suspect my self as having the following physiological sleep characteristics underlying my CSA:
1. Overall hypoventilation (under breathing; increases blood CO2) with periodic hyperventilation (over breathing; reduces blood CO2) and subsequent ceasing of respiration (i.e. CSA) due the blood CO2 dropping below the level required to stimulate the central control system to initiate breathing
2. Hypercapnia (CO2 level in blood higher than normal) resulting from overall hypoventilation
3. High plant gain - i.e. only a small increase in resp rate is required to rapidly lower blood CO2 from hypercapnic levels to the level of eupnea (normal breathing) resulting from hypercapnia
4. High control gain - i.e. small difference in blood CO2 between hypercapnic and eucapnic levels as a result of my brain setup
5. Unstable respiration due to continuous oscillation between hypo- and hyper-ventilation due to these states being too close to eucapnic state in terms of resp rate and blood CO2.
Any thoughts or comments?

Was that by design?
Since your pCO2 could be anywhere from 30 mmHg to 50 mmHg (significantly + or - normal) I think we need to get a better grip on that before we can figure out where you sit in the "Loop".
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Hi Muffy, No, not by design by ignorance. Thank you for the enlightenment grasshopper - I have much to learn. Feedback gain obviously hadn't soaked into me yet! But, yes, I do understand now that determining my PCO2 is of central import.Muffy wrote:I see you left off the Feedback component (perhaps the most important contributor to CompSAS):
Was that by design?
Since your pCO2 could be anywhere from 30 mmHg to 50 mmHg (significantly + or - normal) I think we need to get a better grip on that before we can figure out where you sit in the "Loop".
So the following extract would support what you have pointed out, right?
and hence why you commented?Am J Respir Crit Care Med Vol 163. pp 1181–1190, 2001 wrote:The total delay (i.e., circulation time plus phase shifts related
to mixing and diffusion) determines the cycle duration at
which the ventilatory response (Delta V(dot)E_response) will be 180 degrees
out of phase with the original perturbation in V(dot)E. This is
of critical importance in determining overall LG...
I think I might be having another Neo moment...Muffy wrote:And you're cycling at 120...Lemme think about this...
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Well, I was admittedly a tad surprised to hear your doctor take a purist stance regarding CO2 measurement (or perhaps even a somewhat politely dismissive stance if he happens to view diurnal CO2 measurements as unnecessary). Invasive arterial blood gas analysis is considered the gold standard for accurate measurement of CO2. But the word "trustworthy" is only relative to any methodology's objective...blizzardboy wrote:Thought it futile to try and measure CO2 day and night due to the inaccuracy of EtCO2 measured through a nasal cannula. Only trustworthy measurement would be via intravenous cannula, as in intensive care.
If the objective is to spot highly granular CO2 deltas then I think direct, continuous measurement of arterial blood gas is preferred. However, I don't think that's practical or necessary in this case----and I could be very wrong about that. However, if the objective is to simply spot trends or coarse changes in basal CO2 ---in order to compare day CO2 trending versus night CO2 trending---then noninvasive measurement of EtCO2 via a portable capnometer should do just fine IMO.
And if cannula-based EtCO2 measurements were entirely unsuitable, I don't think they would be clinically employed in practice and research as often as they are. Case-in-point: which CO2 methodology did your clinicians find suitable for PSG?
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
By contrast, blizzardboy, you pointed out a different kind of cycling characteristic that I personally wouldn't dismiss in this confounded SDB mystery. What you had pointed out just might turn out to be an epiphenomenon of some intervening/underlying layer of influence that can ultimately be resolved for the better in your case.blizzardboy wrote:So the following extract would support what you have pointed out, right?and hence why you commented?Am J Respir Crit Care Med Vol 163. pp 1181–1190, 2001 wrote:The total delay (i.e., circulation time plus phase shifts related
to mixing and diffusion) determines the cycle duration at
which the ventilatory response (Delta V(dot)E_response) will be 180 degrees
out of phase with the original perturbation in V(dot)E. This is
of critical importance in determining overall LG...I think I might be having another Neo moment...Muffy wrote:And you're cycling at 120...Lemme think about this...
Some central control/dyscontrol scenarios, unfortunately, are not readily discernible with simple loop-gain modeling. Etiology, pathophysiology, and even degree/complexity of layered dyscontrol are still all unknown IMHO. Not to detract from loop-gain modeling's general usefulness.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
One comment I would add re the Loop gain discussion, is that from what I have read and seen (BB's charts), is that that type of CO2 under/over shoot shows up more as a cyclic 'pattern' whereas the data from BB's charts tends to show erratic patterns. I don't recall seeing any regular pattern of hypo/hyper ventilation ?
DSM
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Aha, I see you already said this ! - I came in late on this thread but it seems we are seeing & saying same re style of pattern.
Tks
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
No. While your phase rate suggests that you have short cycle central dysregulation, I don't think you can definitively say it's due to SDB, and if so, your dial wingin' is a total waste of time. Indeed, the ventilatory instability in your DLs continues unabated no matter what you have selected.blizzardboy wrote:Hi Muffy, No, not by design by ignorance. Thank you for the enlightenment grasshopper - I have much to learn. Feedback gain obviously hadn't soaked into me yet! But, yes, I do understand now that determining my PCO2 is of central import.Muffy wrote:I see you left off the Feedback component (perhaps the most important contributor to CompSAS):
Was that by design?
Since your pCO2 could be anywhere from 30 mmHg to 50 mmHg (significantly + or - normal) I think we need to get a better grip on that before we can figure out where you sit in the "Loop".
So the following extract would support what you have pointed out, right?and hence why you commented?Am J Respir Crit Care Med Vol 163. pp 1181–1190, 2001 wrote:(bunch of complicated stuff)Muffy wrote:And you're cycling at 120...Lemme think about this...
So if you try to plot your case on one of the graphs from your reference:
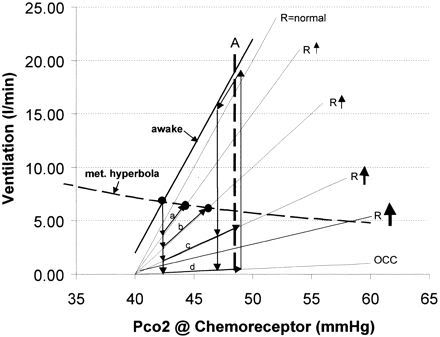
If your CO2 is low, you're off the scale, and if it's high, and since your $4000 machine and dial wingin' must have at some point (if not all points - don't forget, ASV cures everything) given you an R-isopleth that is normal or near-normal, then what you have now is a situation where your VE and pCO2 make it nearly impossible to say that SBD is the thing that is generating your current problem.
[Holding finger on checker] On the other hand, one might argue that if your ABG is compensated, then that whole graph could shift, but while central response might change, the reasonably well-addressed obstructive component would keep you above metabolic hyperbole.
So, "IMHO", and if we ever find out what your real pCO2 is, besides some degree of SBD, you may have at least two other things: an underlying metabolic disorder that causes CO2 retention and sleep instability.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Hi Muffy, Just while I remember, did you have any comment about the nature of my respiration variation during the thirty minute example period of instability during my recent night on fixed CPAP: http://users.adam.com.au/sixsome/ASV/05 ... 10_02b.JPG? I was wondering if the rapid switching between baseline resp rate and the higher values (with a corresponding drop in tidal volume) revealed any useful information to a trained observer, in particular with respect to contributing factors within my LG circuit.Muffy wrote:While your phase rate suggests that you have short cycle central dysregulation, I don't think you can definitively say it's due to SDB, and if so, your dial wingin' is a total waste of time. Indeed, the ventilatory instability in your DLs continues unabated no matter what you have selected.
BTW, if I could sit with you face-to-face now Muffy, and you had any diagnostic currently available to you to use, what would you choose to set me up with to try and gain insight into my sleep disorder?
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
One potentially useful experiment, blizzardboy, might be to eventually use your ASV data set to compare week-long data runs of each modality: 1) your optimal ASV settings, versus 2) fixed pressure set at your optimal obstructive-addressing EEP.
If that latter CPAP modality significantly deteriorated either sleep or daytime symptoms, then you would have to bail out of the experiment early IMO.
If that latter CPAP modality significantly deteriorated either sleep or daytime symptoms, then you would have to bail out of the experiment early IMO.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I don't know how much of that data is really valid for crisp analysis. One can't be sure that you're even asleep. In the case of tidal volumes, it's attempting to measure volumes in the neighborhood of 200 - 500 ml in the face of a background leak of ~30 LPM (when you have a good seal). And it's only pulling out trend points. In a magnified view, it appears to be posting data about every 6 seconds:blizzardboy wrote:Hi Muffy, Just while I remember, did you have any comment about the nature of my respiration variation during the thirty minute example period of instability during my recent night on fixed CPAP: http://users.adam.com.au/sixsome/ASV/05 ... 10_02b.JPG? I was wondering if the rapid switching between baseline resp rate and the higher values (with a corresponding drop in tidal volume) revealed any useful information to a trained observer, in particular with respect to contributing factors within my LG circuit.Muffy wrote:While your phase rate suggests that you have short cycle central dysregulation, I don't think you can definitively say it's due to SDB, and if so, your dial wingin' is a total waste of time. Indeed, the ventilatory instability in your DLs continues unabated no matter what you have selected.

So what does the VT trend really mean? Can it be used to accurately determine VT? Does the timing match up correctly to the rate changes? Do abrupt VT decreases vs. downward trends have clinical relevance? Or, during those periods of high respiratory rates when the VT drops, is that simply an error in measurement?
I think respiratory rate lends itself to present accurate data in trend analysis, and the MV is very helpful in determining respiratory stability (however, this may be somewhat of an "art form". With 6-second data posting, everything appears to have 5 cycle/minute frequency).
Further, look at that MV upwards creep toward the end. The VT and rate are relatively stable, so how can that be ("IMHO", it's how the algorithm deals with sudden changes. It corrects relatively slowly)?
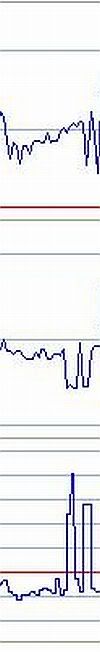
Reminder: Insert leak sample here:
Anyway, that said, and in a whimsical flight of fancy, I would say that your original screen has 20 spontaneous arousals and 6 hypopneas. The hypopneas could just as easily be central as obstructive.
THE -HCO3!!! BICARB!!! BI-CARB!!!!!!!! IF I'VE ASKED YOU ONCE I'VE ASKED YOU A MILLION TIMES, GET ME A NEW MF BICARB!!!!blizzardboy wrote:BTW, if I could sit with you face-to-face now Muffy, and you had any diagnostic currently available to you to use, what would you choose to set me up with to try and gain insight into my sleep disorder?
Happy Mother's Day.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Yes, I know what the software said, but these are the Muffy Scoring Rules.Muffy wrote:I would say that your original screen has... 6 hypopneas. The hypopneas could just as easily be central as obstructive.
Now let me get back to putting my washing machine back together so I can clean my greasy clothes that I got from putting my washing machine back together:

Bad trans on right (blown seal). Good trans on left (from neighbor's machine. Boy is SHE going to be surprised!)
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem










