CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I still would not discount (silent) GERD (briefly touched upon on page 4). If you're having night-time flare-ups, AND you scored high on the sensitivity scale, it could be a cause of some of those arousals. By the way is reflux or other gastro problems a side-effect of any of those meds?
As jnk reminded us, the low night-time BP also sounds a bit strange...
Also I wouldn't underestimate the power of getting good exercise to help you sleep better. I know, easier said that done Been there done that. If you're pressed for time and/or energy, try getting 10 minutes a day or every other day, and work your way up. Go for a walk, a bike ride, get a Wii , walk up and down stairs for 10 minutes during your lunch break, whatever it takes to get some movement in.
As jnk reminded us, the low night-time BP also sounds a bit strange...
Also I wouldn't underestimate the power of getting good exercise to help you sleep better. I know, easier said that done Been there done that. If you're pressed for time and/or energy, try getting 10 minutes a day or every other day, and work your way up. Go for a walk, a bike ride, get a Wii , walk up and down stairs for 10 minutes during your lunch break, whatever it takes to get some movement in.
PR System One APAP, 10cm
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Our pros can correct me if I'm wrong, but if you have PLMD, while there are some lifestyle and nutritional recommendations, along with giving attention to the ferritin level, this disorder can be resistent to improve much by these means. And IF yours were to happen to be med induced, those efforts would be irrelevant. I don't mean to sound discouraging, but true PLMD will not be fixed by treating OSA. You have such a high number of movements. I just don't know how likely it is you're going to make much of a dent in those without a direct approach. And they may be so intricately tied in to your overall sleep architecture that they could sabotage your other efforts. There's more to them than the movement that shows on a test. When my prior medication was causing my movements to intrude into my superficial sleep and I was aware of them and all the sensations that surround them, I realized there is a buildup of tension before the abrupt movements. I wonder how that could affect sleep architecture. Just consider if things are improving as you would hope, you may need to make addressing your movements a co-priority. By the way, I wasn't saying don't take the dopamine meds, I was saying not to take them casually. If the movements make quality sleep impossible, I see that as a necessity.blizzardboy wrote:I concur wholeheartedly. I was very hesitant to go on fluoxetine. I would probably been even more concerned about taking the types of drugs that I have seen listed for treating PLMD. I think I would like to ensure that I have exhausted as many health, diet, exercise, relaxation, etc options before I start going down the meds path. For, as you testify to, tampering with one's biochemistry can be a bit of a Pandora's box.
Hope you find the magic formula for all your sleep issues to be resolved.
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
No, it looks like a majority of 9 cps alpha, there's isn't enough mixed frequency theta to stretch that into a 1.blizzardboy wrote:Maybe not? Did you notice that the EEG/ECG traces are on a different time scale to the others? Does this change your reading?Muffy wrote:BTW, in the Epoch you presented from the HST:
(look back for picture)
you're awake. Throw out all those centrals.
Muffy
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
[quote="Muffy No, it looks like a majority of 9 cps alpha, there's isn't enough mixed frequency theta to stretch that into a 1.
Muffy[/quote]
I love sitting in on technical conversations, listening intently, and pretending like I'm actually a part of it!
Muffy[/quote]
I love sitting in on technical conversations, listening intently, and pretending like I'm actually a part of it!
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
NM, you mean the 30 second epoch on top vs. the 5 minute epoch on the flow channels. It looks like you started out with some flow limitation that led to an arousal to start the cascade, so you were probably asleep at that point. Lemme do a C&P to try to put that epoch where it should be.Muffy wrote:No, it looks like a majority of 9 cps alpha, there's isn't enough mixed frequency theta to stretch that into a 1.blizzardboy wrote:Maybe not? Did you notice that the EEG/ECG traces are on a different time scale to the others? Does this change your reading?Muffy wrote:BTW, in the Epoch you presented from the HST:
(look back for picture)
you're awake. Throw out all those centrals.
Muffy
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Bloodwork: Check Ferritin, Iron, TIBC, Transferrin Saturation, and Transferrin, not just Ferritin. This is very important and you're regular internist may only know to draw Ferritin and not all the rest.
Check Folate. While they are drawing blood, you might as well check Magnesium too.
These are to rule out possible causes of PLMS.
I should have thought of this awhile back in this thread, sorry. If you were anemic, this could explain a lot of your symptoms. Any GI issues that you know?
Check Folate. While they are drawing blood, you might as well check Magnesium too.
These are to rule out possible causes of PLMS.
I should have thought of this awhile back in this thread, sorry. If you were anemic, this could explain a lot of your symptoms. Any GI issues that you know?
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
SU, do you happen to have any links readily available about the various tests you mentioned and how the different aspects they are testing play a role in some people's limb movement issues? My knowledge on that is very generic. Just know that the brain uses iron in it's processing of movement. Are the other tests the kind of thing that if the ferritin is low and doesn't respond to added iron, then further investigation is needed? I mean, can one have a good ferritin level and still have the other tests be abnormal?
Seems I remember from old discussions that although a large number of those with RLS (and/or PLMD) have low ferritin levels, it doesn't translate to a similar number experiencing relief by addressing their low iron issues. Guess I need to do some research. Things have likely changed in the last few years. Since it's still a bit mysterious the different causes of the symptoms, understandable that the resolution that works for one might not another. We have one board member that gets periodic blood transfusions to address her severe anemia. She has said that when she is due for a transfusion her movements are real bad, but that she does find relief after.
My brain is tired. Must need more iron.
Seems I remember from old discussions that although a large number of those with RLS (and/or PLMD) have low ferritin levels, it doesn't translate to a similar number experiencing relief by addressing their low iron issues. Guess I need to do some research. Things have likely changed in the last few years. Since it's still a bit mysterious the different causes of the symptoms, understandable that the resolution that works for one might not another. We have one board member that gets periodic blood transfusions to address her severe anemia. She has said that when she is due for a transfusion her movements are real bad, but that she does find relief after.
My brain is tired. Must need more iron.
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Kathy, I don't think I have any articles that explicitly state what the various tests measure relative to each other, but I know for a fact (and there are very few things that I know for a FACT!) that it's possible to have normal Ferritin, but have one of the other tests be abnormal. So you should run all tests at the same time because if you only run Ferritin and it's normal, it doesn't mean you aren't iron deficient.
Yes, exactly.I mean, can one have a good ferritin level and still have the other tests be abnormal?
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
AFAIK, my GI seems to be OK. Regular performance on a strong stool. No indigestion, reflux or heart burn. Just my old mate aerophagia.SleepingUgly wrote:Bloodwork: Check Ferritin, Iron, TIBC, Transferrin Saturation, and Transferrin, not just Ferritin. This is very important and you're regular internist may only know to draw Ferritin and not all the rest.
Check Folate. While they are drawing blood, you might as well check Magnesium too.
These are to rule out possible causes of PLMS.
I should have thought of this awhile back in this thread, sorry. If you were anemic, this could explain a lot of your symptoms. Any GI issues that you know?
I went to make a call to my GP just then and then hung up. I think I will give myself one month on ASV to give my body a decent chance to shift its equilibrium if required. Probably best for me to keep the variables to a minimum in order to have confidence in my numbers.
Thanks for the list of tests. I will take them to my GP when the time comes. I had a blood test about one and half years ago and there were no anomalies inc. thyroid function and iron. I will have a look to see if any of the above were checked.
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Somewhat common "silent GERD" would be GERD without symptoms. I have silent GERD.blizzardboy wrote: No indigestion, reflux or heart burn. Just my old mate aerophagia.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2576329/
I look forward to hearing about your upcoming trial, blizzardboy. Good luck!
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
SWS, how do you know you have GERD if it's silent?-SWS wrote:I have silent GERD.
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Did you have any of your current problems 1.5 yrs ago when your iron was tested?blizzardboy wrote:I had a blood test about one and half years ago and there were no anomalies inc. thyroid function and iron. I will have a look to see if any of the above were checked.
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Thanks Muffy! Hygiene is 81 outta 100, pretty good.Muffy wrote:Here's a couple threads where sleep hygiene is discussed:
viewtopic/p472062/viewtopic.php?f=1&t=4 ... ne#p401345
viewtopic/p472062/viewtopic.php?f=1&t=4 ... ne#p372562
...
Didn't know my T3 levels could affect sleep! Diagnosed hypo last Sept, TSH hit 5.91, last lab 2.83 better but I feel best when under 2 (periodically my thyroid system goes wonky then in a few months 'fixes' itself)...free T3 in now consistently in the lower third of the range, on levothyroxine now. Interesting, my wakeups really got started in earnest when my TSH went into the 4s Dec '08... a yr of these dratted frequent wakeups. Maybe this is my key to managing this really frustrating activity....will do some investigation. Why haven't my docs mentioned this .
THANKS!
ResMed S9 range 9.8-17, RespCare Hybrid FFM
Never, never, never, never say never.
Never, never, never, never say never.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I believe this is where the Wake epoch is (blue bar):Muffy wrote:It looks like you started out with some flow limitation that led to an arousal to start the cascade, so you were probably asleep at that point. Lemme do a C&P to try to put that epoch where it should be.
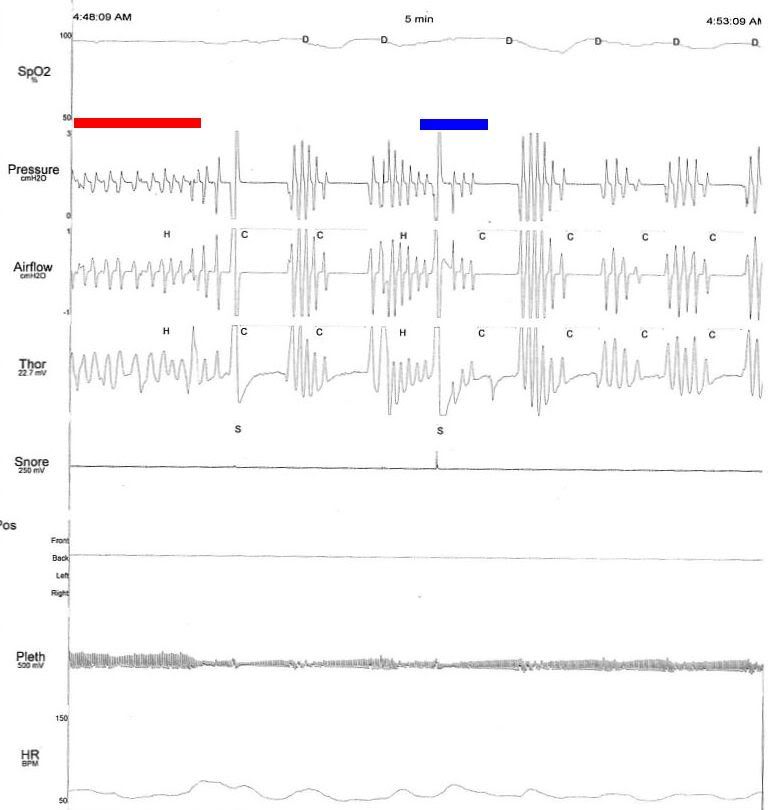
Red bar over area of flow limitation leading to probable arousal and post-arousal central.
Can you get the download from the ASV?
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Endoscopic exam after getting food caught in my esophagus. Your question perfectly highlights my current ongoing problem: if GERD severity is variable (and it is) how do I know when I'm under-treated? My last endoscopic exam showed that I was slightly under treated. My next endoscopic exam is several years down the road.SleepingUgly wrote:SWS, how do you know you have GERD if it's silent?-SWS wrote:I have silent GERD.
Lack of GERD symptoms clearly does not imply lack of GERD---especially in the SDB population.
Back on topic: Might variable or episodic GERD occasionally affect blizzardboy's home-measured data? It will be interesting to see how stable all the upcoming home measurements stay.












