The server dudes here at work block that site from me entirely.-SWS wrote:. . . to download the files. . . .
CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
jnk wrote:The server dudes here at work block that site from me entirely.-SWS wrote:. . . to download the files. . . .
Well, I just now managed to retrieve the linked file and added this comment to my previous post:
-SWS wrote:I just downloaded the file successfully. Not sure what went wrong the first time. I saw this erroneous average heart rate followed by the :I certainly wouldn't put hypoventilation, hypercapnia, bradycardia, or vagal events on the front burner or back burner based on that data. However, if I episodically returned wild swings in my home-measured BP, SpO2, or ASV data, then I'd take a close look at some of those possibilities. My understanding is that some cardiac and central symptoms can be highly transient---especially during onset of certain diseases.Average heart rate during sleep: 20
Number of Bradycardic periods: 0
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I can't see your data. Did you have PLMs on the home study that you didn't discontinue Fluoxetine for? On the "real" study in the lab, the one that you discontinued Fluoxetine 2 weeks prior, did the PLMs cause arousals?blizzardboy wrote:Given that I apparently have a lot of PLMs I certainly would be interested to know what are the options for treatment.
Muffy, what is your position on PLMS in the absence of arousals? It is controversial.
The first line treatments for PLMS are dopaminergics. Personally, I would not be inclined to take dopaminergics, nor 2nd line therapies such as gabapentin, for PLMs that might be medication-induced. I would personally rather get off the Prozac and see what my sleep looked like without it (although keep in mind there is great night-to-night variability with PLMS, although someone who has 450/8 hrs, ought to evidence still quite a few if it's not medication induced...I would think...). I know this might be easier said than done because withdrawing gradually from Prozac takes time, and you'd have to deal with the implications of your untreated depression and anxiety.
(Aside: I am very curious what studies have been done on the implications of REM-suppressing agents, such as Fluoxetine, on the sleep of those who have REM-dependent OSA... Just curious.)
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Please try this link to see my PSG reports:SleepingUgly wrote:I can't see your data. Did you have PLMs on the home study that you didn't discontinue Fluoxetine for?
http://users.adam.com.au/sixsome/
The home study did not monitor leg movements.
I would also like to add that during my diagnostic study I was kept awake for quite a while during the night due to the loud snoring coming from the room next door.
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Sure, can't hurt, but I reserve the right to debate whether or not this is truly CompSAS at some point. The 11.02.2010 study was on ambient pressure (CompSAS is usually defined as the appearance of centrals with the addition of pressure) and their location could make them caused simply by sleep fragmentation (they are post-arousal) or due to sleep transition (dozing at the end of the night's sleep).blizzardboy wrote:Probably good just to give my body a good run on the ASV first. What do you reckon?
However, a major issue is your sleep architecture, which is poor. You have these long periods of wake in the middle of the night that need to be addressed.
To try to explain sleep architecture, here's a spot done a while ago:
Sleep Architecture 101
These are examples of hypnograms showing sleep architecture during a full night's sleep.
The first example represents normal sleep. Sleep progresses from wake, through light sleep (Stage 1 and 2), followed by deep sleep (Stages 3 & 4), and finally a REM period. This is called a Sleep Cycle, and takes about 90 minutes to complete. There are usually 4-6 Sleep Cycles per night. Most deep or delta sleep occurs in the first Sleep Cycle. The duration of REM periods increase as the night goes on. Normal sleep stage percentages are Stage 1 5%, Stage 2 60%, Stage 3 & 4 combined 20%, and REM 20%. Delta sleep generally decreases as a function of age.

This example represents someone with OSA. After sleep onset, the patient moves back and forth from Stage 1 to Stage 2 sleep. Stage 1 sleep is simply a transition stage to quality sleep and should only appear at the beginning of the night. It has virtually no value as far as restorative sleep goes. It is should not appear to any great degree once bona fide sleep begins. There is no delta sleep whatsoever. REM sleep is 19.9%. The patient is aroused to wake at least 10 times. There is some continuous stage 2 and REM sleep, but overall this is fairly poor quality sleep, with frequent disruptions caused by OSA.

This example shows a patient with a large quantity of delta sleep (20.8%) and REM sleep (33.8%). Sleep is fairly continuous. This patient will be well rested in the morning. This patient is the one from example 2 during his CPAP titration. This greater than normal quantity of delta and REM sleep is termed Rebound Phenomenon. With regular use, the CPAP user will move to a more normal sleep architecture as the "sleep debt" is paid off. This usually occurs in a day or so. This also serves to explain why some people think they slept so well in the lab, but then do poorly at home. It's not that they're doing poorly, they're actually now approaching normal architecture, the aggravating factor is now gone.

This example represents a Split-Night study. Initially, there is a very disrupted, light sleep pattern, that turns into prolonged REM after application of CPAP. There are areas of sustained sleep, but there are still areas of disrupted light sleep. This patient also had Periodic Limb Movements which continued to disrupt sleep even though respiratory events were well-controlled on CPAP.

There should probably be about 40-50 stage shifts in a normal, healthy patient not troubled by lab effect (the test itself can drive up the stage shifts). Most references are looking at about 7 stage shifts per hour, give or take. There should be few, if any awakenings, perhaps in the neighborhood of like "2". An awakening is a sleep disturbance that lasts >15 seconds, as opposed to an arousal, which lasts 3 - 15 seconds. Consequently, awakenings are highly disruptive to sleep.
BTW, those were generated prior to the new standards for NREM, which now combine Stages 3 & 4.
________________________________________________
In re: the PLMs, if they generate a lot of arousals, they should be treated. However, not only can SSRIs make PLMs worse, they can be highly disruptive to sleep. In an effort to kill three birds with one stone, if you need an ADM, there is one that is PLM friendly, Wellbutrin (bupropion) that you might want to consider.
Needless to say, changing your ADM regimen is something that you really need to review carefully with your physician. SSRI Discontinuation Syndrome can be a major drag.
We need the Muffy Guide to sleep hygiene.
Are you on any other medications?
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
By comparison, your sleep architecture on the 25.02.2010 titration:
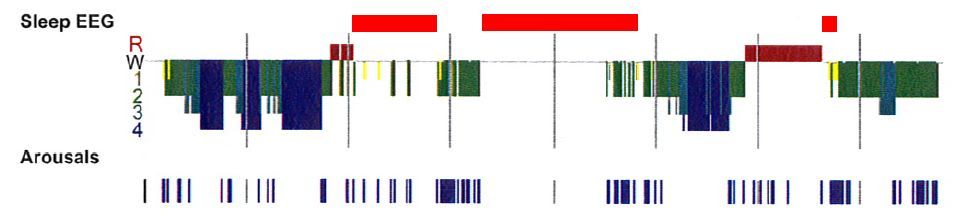
shows long periods of sustained wake and severe fragmentation (marked by red bars) as well as that Stage 2 at about 0130 which is swarming with arousals.
That's a lot of bad "sleep".
Muffy
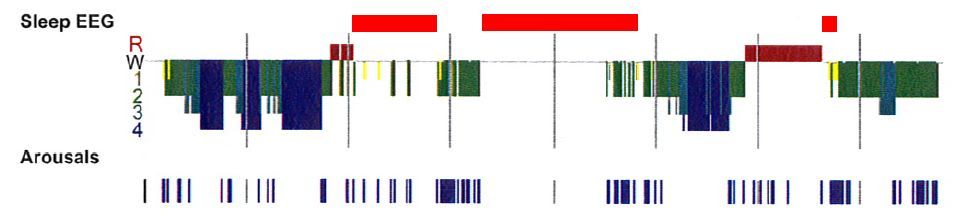
shows long periods of sustained wake and severe fragmentation (marked by red bars) as well as that Stage 2 at about 0130 which is swarming with arousals.
That's a lot of bad "sleep".
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Yup, yup, yup...ASAP! I had lousy sleep architecture: skipping between S1 & S2, 2 mins of S3, no S4, no REM, AHI 62 all hypops, Sa02 went down to 83%, average heart rate 98 (yikes, I forgot this), no limb movement, normal EKG & EEG, arousal index=30 mostly resiratory; split-study sleep efficiency 99% (no numbers given in summary) & SaO2 +92%. I barely made it into the category of slept long enough for insurance to pay for my PSG. First 17-18 months with dataless CPAP, I slept thru the night; thereafter, wakeups every 90-120 mins. Still have wakeups; now that I have detailed data, tracking to see if these follow events, so far, some yes, some no. Hypersensitive to noise, light, movement (even air), temp changes, state of my chronic congestion (vasomotor rhinitis, allergies, chronic sinusitis), phase of the moon too maybe -- it's so very frustrating not to be able to stay asleep & being tired as a result. The more wakeups, the lousier I feel the next day. Since last Nov, my average AHI=1.4 with AI=0.1, some--maybe many--envy these numbers I know but these wakeups are wrecking havoc with my energy, alertness, sleepiness, cognition, mood regardless of how good they are. We all have our crosses to bear with SDB and right now mine seem to cluster around my variable congestion and these dratted wakeups. Oh, I also still have a ton of wt to lose; lost 57#, then stalled for a yr, gained back 12 over the last few months and can't seem to find the energy, time, or incentive to exercise regularly -- the excess wt isn't helping either. At least my bloodwork's better, no more compensation as if I were living at high altitute so I assume I'm not desating much.Muffy wrote:...We need the Muffy Guide to sleep hygiene....
I take no psychoactive drugs; I take lots of supplements, omega 3s & DHA, & eat very low carb. Thinking of trialing melatonin tho I fall asleep fairly easily. With a yr's layoff & now some demanding contract work, I'm stressed and it's hard to get a routine going so I'm only sleeping 7.5 hrs or so when I really need 8...with wakeups, who knows how many hrs I'm actually asleep .
Muffy, please post sleep tips...I'm already doing everything I know to do and it's not helping me get restful sleep.
~~~~~~~~
Control returned to OP...reading thread with much interest. What can cause that sort of severe sleep fragmentation that OP shows?
ResMed S9 range 9.8-17, RespCare Hybrid FFM
Never, never, never, never say never.
Never, never, never, never say never.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Unless it falls on his head, of course.Muffy wrote:Sure, can't hurt . . .blizzardboy wrote:Probably good just to give my body a good run on the ASV first. What do you reckon?
What about the whole "80 mmHg systolic" hypotension thingy?:
Or did that get addressed, and I just got lost again? Sorry if I did.blizzardboy wrote:. . . using a CMS-60C ABPM I find that my blood pressure drops to 80/43 during the night . . .
jeff
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I have also now added my home PSG as three JPGs to this webpage:
http://users.adam.com.au/sixsome/
Its odd for me to even consider that I have a sleep disorder as I have said for most of my life that one of my key strengths has been the ability to get a good sleep anywhere, anytime.
http://users.adam.com.au/sixsome/
Its odd for me to even consider that I have a sleep disorder as I have said for most of my life that one of my key strengths has been the ability to get a good sleep anywhere, anytime.
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
There's always the possibility that PLMD would be present without any of the meds in question, and that a med is exacerbating the symptoms. I've been in the situation of going off a med and finding a degree of relief, then going back on it just to know for sure the role it played. It was a few miserable months out of my life that I never want to relive, but I'd do it again if there was ANY chance to reverse the pattern of adding meds to treat the side effects of other meds. BlizzardBoy, it seems to me you are between a rock and a hard place regarding the limb movements. Just knowing what I know now after over 10 years on meds for mine, I would not add ANY med for the limb movements without knowing beyond a shadow of a doubt that going off another med wouldn't resolve them, unless that med was necessary to my very life and I had no choice. What that looks like for you is very personal. I'm not the one who would have to live in your hell if you were to choose to start working with your doctors to research this in a methodical safe manner. I just can't help but wonder if you are stuck in a vicious cycle, that your fragmented sleep is responsible for at least some of your need for meds, and if the sleep issues were resolved (which PLMS play a big role), you wouldn't need so much of the meds. Besides arousals, the body needs to rest during sleep. Your legs don't rest. I have found the chronic muscle and joint pain to be as limiting as the poor sleep, just in different ways. Do you have pain with yours? I just broke down and called my doctor today. As much as I dread another transition, the Requip is now causing more limb movement issues than it is fixing. Woke up last nite in the middle of a movement - lying on my side my arm was stretched straight up in the air like the hand on a clock pointing toward midnight. Enough is enough. These exaggerated movements aren't the PLMD, they're the side effect of the high dose of the med. This is not a path you want to take if it is in your power to avoid it.
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I concur wholeheartedly. I was very hesitant to go on fluoxetine. I would probably been even more concerned about taking the types of drugs that I have seen listed for treating PLMD. I think I would like to ensure that I have exhausted as many health, diet, exercise, relaxation, etc options before I start going down the meds path. For, as you testify to, tampering with one's biochemistry can be a bit of a Pandora's box.kteague wrote:Besides arousals, the body needs to rest during sleep. Your legs don't rest. I have found the chronic muscle and joint pain to be as limiting as the poor sleep, just in different ways. Do you have pain with yours? I just broke down and called my doctor today. As much as I dread another transition, the Requip is now causing more limb movement issues than it is fixing. Woke up last nite in the middle of a movement - lying on my side my arm was stretched straight up in the air like the hand on a clock pointing toward midnight. Enough is enough. These exaggerated movements aren't the PLMD, they're the side effect of the high dose of the med. This is not a path you want to take if it is in your power to avoid it.
Probably best to start with a good period of ASV usage and then have another PSG. I am sure a few iterations can be undertaken before the need to consider meds.
OK. So how to improve architecture? I have cut right back on alcohol consumption. My diet is pretty good although maybe a little too high in carbs. My exercise levels are not satisfactory at present (exacerbated by fatigue related to sleep problems). I don't smoke. Maybe three coffees per day. No other recreational drugs. I have a new bed and mattress that seems to be comfortable for my body. I don't each much after 7:30pm, tend to be in bed no later than 10:30pm and usually sleep until 7:30am.Muffy wrote:...swarming with arousals. That's a lot of bad "sleep".
Muffy
BTW, thank you for posting all that architectural info - I really appreciate your time and effort.
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Here's a couple threads where sleep hygiene is discussed:
viewtopic/p472062/viewtopic.php?f=1&t=4 ... ne#p401345
viewtopic/p472062/viewtopic.php?f=1&t=4 ... ne#p372562
Is there another page of the home study showing the architecture?
The text report shows the same pattern of sleep maintenance insomnia.
Interestingly, they make that important point about the origin of the centrals, namely, that they are post-arousal in nature-- a sleep disturbance occurs, you hyperventilate a little bit, then have a compensatory central apnea, which is normal. Now, while an increased frequency response following an arousal (5 centrals following an arousal) is suggestive of the hyperreactivity of CompSAS, I think this is a subtle, but very important point to argue that your CompSAS is not clinically relevant. It makes no sense to hammer a post-arousal central with an ASV because the damage is done. Further, from the data presented so far there's no evidence of pressure-induced centrals. If arousals are causing the centrals, you have to find and fix the cause of the arousals.
If everything gets optimized and sleep architecture remains poor, I would consider the use of Cognitive Behavior Therapy.
Consider changing/getting rid of the ADM. This must be done under physician recommendation/supervision because untreated depression can create even worse sleep problems than you have now, and during the withdrawal phase, probably will. The problem with that is then you tell the doctor "hey, I'm crawling out of my skin" so he gives you some sort of Happy Juice that makes your OSA worse (although probably not because it's not all that bad to begin with and you're on pressure support) or fall asleep at the wheel going 90 miles an hour on the A1 cause you've got a grog on and you pile into a flock of roo (or whatever a herd of them things are called) and end up in a ravine somewhere (ASV is touted as being able to fix everything, but it definitely can't fix dead).
Muffy
viewtopic/p472062/viewtopic.php?f=1&t=4 ... ne#p401345
viewtopic/p472062/viewtopic.php?f=1&t=4 ... ne#p372562
Is there another page of the home study showing the architecture?
The text report shows the same pattern of sleep maintenance insomnia.
Interestingly, they make that important point about the origin of the centrals, namely, that they are post-arousal in nature-- a sleep disturbance occurs, you hyperventilate a little bit, then have a compensatory central apnea, which is normal. Now, while an increased frequency response following an arousal (5 centrals following an arousal) is suggestive of the hyperreactivity of CompSAS, I think this is a subtle, but very important point to argue that your CompSAS is not clinically relevant. It makes no sense to hammer a post-arousal central with an ASV because the damage is done. Further, from the data presented so far there's no evidence of pressure-induced centrals. If arousals are causing the centrals, you have to find and fix the cause of the arousals.
If everything gets optimized and sleep architecture remains poor, I would consider the use of Cognitive Behavior Therapy.
Consider changing/getting rid of the ADM. This must be done under physician recommendation/supervision because untreated depression can create even worse sleep problems than you have now, and during the withdrawal phase, probably will. The problem with that is then you tell the doctor "hey, I'm crawling out of my skin" so he gives you some sort of Happy Juice that makes your OSA worse (although probably not because it's not all that bad to begin with and you're on pressure support) or fall asleep at the wheel going 90 miles an hour on the A1 cause you've got a grog on and you pile into a flock of roo (or whatever a herd of them things are called) and end up in a ravine somewhere (ASV is touted as being able to fix everything, but it definitely can't fix dead).
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
BTW, in the Epoch you presented from the HST:
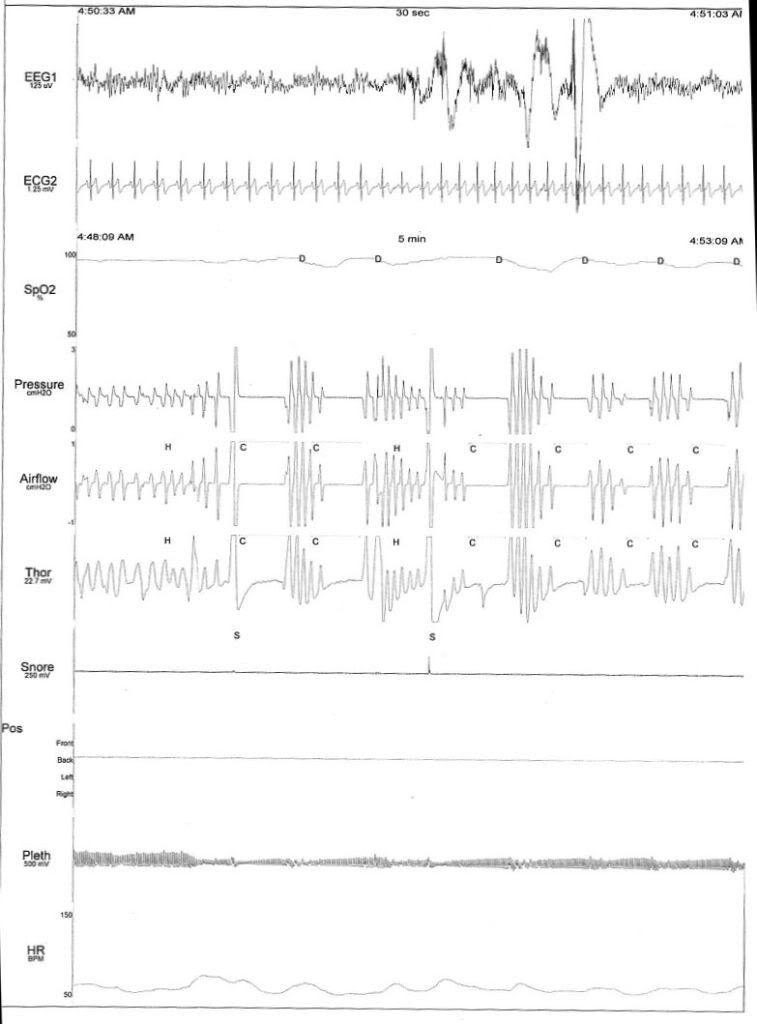
you're awake. Throw out all those centrals.
Muffy
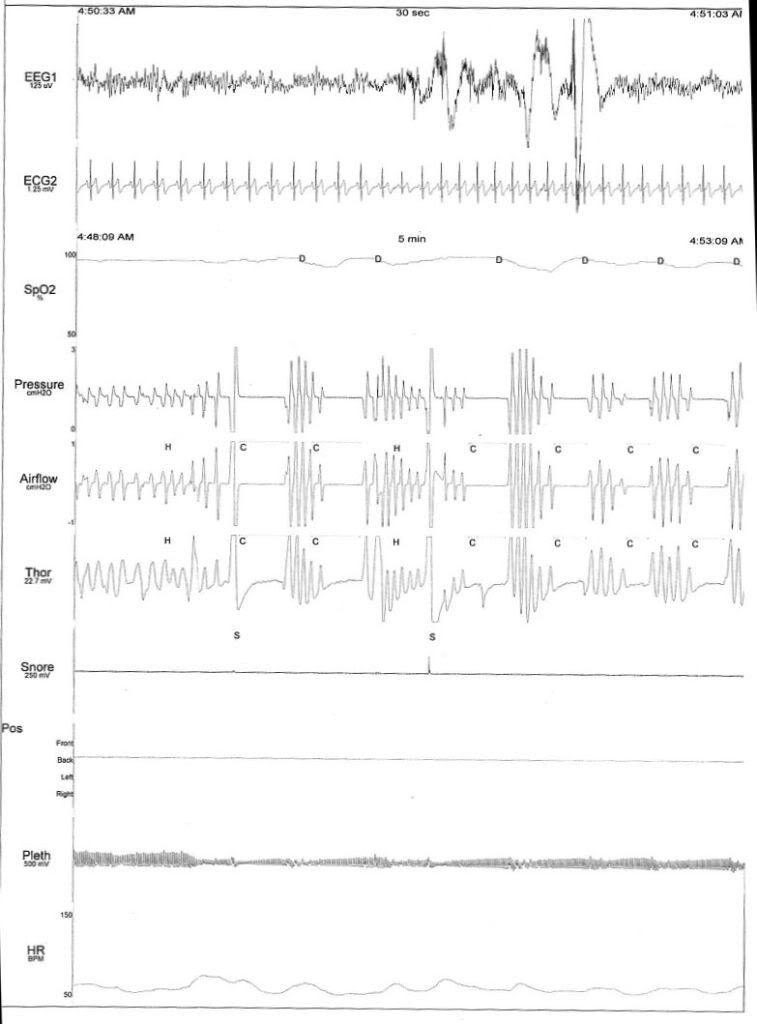
you're awake. Throw out all those centrals.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
I scored 55 on that high-tech sleep hygiene survey. 'Twould seem I am a moderately grubby sleeper.Muffy wrote:Here's a couple threads where sleep hygiene is discussed:
viewtopic/p472062/viewtopic.php?f=1&t=4 ... ne#p401345
viewtopic/p472062/viewtopic.php?f=1&t=4 ... ne#p372562
No sleep architecture page was shown/given to me following my first PSG.Muffy wrote:Is there another page of the home study showing the architecture?
I can see that my sleep architecture is not necessarily helped by the ASV, but isn't it still worth having an ASV assist in ventilating me during centrals until the cause of arousals is identified?Muffy wrote:It makes no sense to hammer a post-arousal central with an ASV because the damage is done.
I have been receiving CBT regularly for a couple of years now. Profoundly helpful to me.Muffy wrote:If everything gets optimized and sleep architecture remains poor, I would consider the use of Cognitive Behavior Therapy.
Ditch fluoxetine, eh? I'll talk to my GP about options less likely to increase PLMs. Elsewise: Get properly fit again? Work outdoors? Plenty of sunlight?Muffy wrote:Consider changing/getting rid of the ADM.
Muffy
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
- blizzardboy
- Posts: 368
- Joined: Mon Feb 15, 2010 12:13 am
- Location: South Australia
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Maybe not? Did you notice that the EEG/ECG traces are on a different time scale to the others? Does this change your reading?Muffy wrote:BTW, in the Epoch you presented from the HST:
(look back for picture)
you're awake. Throw out all those centrals.
Muffy
Machine: Resmed VPAP Adapt SV Enhanced
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM
Mask: Resmed Quattro/Mirage Liberty
Humidifier: Resmed H2i
Other comments: Sleepzone heated tube; CMS-50E SPO2 & CMS-60C ABPM











