ResMed vs. Respironics: AHI and Variable Breathing
ResMed vs. Respironics: AHI and Variable Breathing
This posting is dedicated to Muffy, who has made what I think to be an extremely important and insightful observation. Her comments can be found in:
viewtopic.php?f=1&t=44022 Frustrated re: Lack of Improvement w #’s
I am initiating this separate thread, concerned that Muffy’s significant contribution may not be widely seen in that location.
What is Variable Breathing?
I wish I knew. A variety of patents describe methods of identifying “irregular breathing” which may indicate anything from partial wakefulness, to REM sleep, and to utilize that information in regulating AutoPAP algorithms. It has been known to some (though nothing about it appears on EncorePro or EncoreViewer reports) that Respironics smartcard data (.xml files) includes information about Variable Breathing: time-stamped notations of each occurrence, and total time in a Variable Breathing state for the night. Mr. Skinner’s Encore Pro Analyzer presents graphic information about Variable Breathing.
The topic has been occasionally discussed in this forum; see, for example,
viewtopic.php?f=1&t=36541
ResMed vs. Respironics AHI numbers
It is “common knowledge” that respiratory event numbers reported by ResMed machines and software “tend to be higher” than similar numbers reported by Respironics machines and software. This has caused some concern and confusion, particularly in light of the frequently repeated “guidance” that the “goal” of PAP therapy should be an AHI of 5.0 or less. ResMed users in particular have reportedly been troubled by an inability to meet that “goal.”
There are two common explanations for the difference in AHI numbers between the two machine manufacturers.
1) The concepts of “apnea” and “hypopnea” are defined, and thus measured and reported, differently by the two manufacturers. This affects both CPAP and AutoPAP.
2) At least in part as a result of this, but also due to other intentional differences, the AutoPAP algorithms of the two manufacturers behave differently, producing different results.
RestedGal, in a very practical effort to allay undue concerns about this “5.0 goal,” has at various times suggested that ResMed users might “mentally” divide their HI in half, and then add it to their AI, to arrive at an “adjusted” AHI which might be more “comparable” to the numbers produced by Respironics. This suggestion has been met with the criticism that it implies that Respironics numbers are “right” in a way which makes the ResMed numbers “wrong.”
Respironics and Variable Breathing
Muffy, in the post cited above, argued very cogently that, in fact, the Respironics numbers may be “wrong” because of Variable Breathing issues. She hypothesized that not only did Respironics machines identify and collect Variable Breathing data (though their reports never mentioned these data), but that the Variable Breathing construct was in fact being used by Respironics machines. Possibly, Variable Breathing was an active factor in the Respironics AutoPAP algorithm. In addition, Variable Breathing, Muffy hypothesized, affected the way both CPAP and AutoPAP machines actually reported apneas and hypopneas.
If accurate, this would constitute a THIRD and largely unrecognized mechanism underlying the difference between AHI numbers for the two manufacturers:
3) When Respironics machines detect Variable Breathing, they DO NOT REPORT apneas or hypopneas which might otherwise be present, according to their definitions of these events.
In response to Muffy’s hypothesis, I spot-checked a number of my own Respironics data collections (in both CPAP and AutoPAP modes). I have found no situations in which her hypothesis was incorrect. While this does not confirm its accuracy, I find it to be very convincing. And very disturbing.
An Example
I offer the following example, selected because of the high density of respiratory events. Several weeks ago I intentionally created a situation in which I would have VERY high AI and HI numbers during therapy with a Respironics M-Series AutoPAP machine, set in fixed-pressure CPAP mode. (I was paying no attention to Variable Breathing at the time).
My AHI was 37.7 over a 6h:22m blower time, consisting of an AI of 8.8 (56 events) and an HI of 28.9 (183 events). Yes, terrible. On re-analysis, with a specific view toward Variable Breathing, this condition was present for 5h:3m, or 80.7% of the total blower-on time.
But here is the key. During any timeframe (Respironics reports respiratory events in 30-second time windows) in which Variable Breathing was reported, NO OTHER respiratory event was reported.
The following link (I provide it as a url link to an Excel spreadsheet rather than as an image due to its length; it is safe to open it) shows “raw” Respironics data for a period of a bit over an hour. There are 136 time-stamped data points. Ten reflect apneas. Forty reflect hypopneas. Eighty one reflect Variable Breathing. All but five show events: exactly ONE event each.
Look at the patterns. Look at how apneas and hypopneas “pop out” when Variable Breathing is not reported. And ask: is it more likely that there were no apneas or hypopneas during Variable Breathing periods, or is it more likely that Variable Breathing is SUPPRESSING the reporting of apnea and hypopnea events?
http://velbor.home.comcast.net/cpap/cpap_vb.xls
Implications
If we conclude that Respironics “Variable Breathing” suppresses the reporting (and the inclusion in AHI statistics) of apneas and hypopneas, it changes how we must think about what these numbers mean. (It does not - necessarily - change our standards for “adequate therapy.”
My own typical spending of about 1/3 of the night in Variable Breathing may be different from what others experience. The link about Variable Breathing referenced earlier includes a “questionnaire” regarding frequency of occurrence through the night; in real time the distribution is:
viewtopic.php?f=1&t=36541&start=0&st=0& ... w=viewpoll
This is a new twist which should be discussed and absorbed, and I invite comments to this thread to begin the process.
Velbor
viewtopic.php?f=1&t=44022 Frustrated re: Lack of Improvement w #’s
I am initiating this separate thread, concerned that Muffy’s significant contribution may not be widely seen in that location.
What is Variable Breathing?
I wish I knew. A variety of patents describe methods of identifying “irregular breathing” which may indicate anything from partial wakefulness, to REM sleep, and to utilize that information in regulating AutoPAP algorithms. It has been known to some (though nothing about it appears on EncorePro or EncoreViewer reports) that Respironics smartcard data (.xml files) includes information about Variable Breathing: time-stamped notations of each occurrence, and total time in a Variable Breathing state for the night. Mr. Skinner’s Encore Pro Analyzer presents graphic information about Variable Breathing.
The topic has been occasionally discussed in this forum; see, for example,
viewtopic.php?f=1&t=36541
ResMed vs. Respironics AHI numbers
It is “common knowledge” that respiratory event numbers reported by ResMed machines and software “tend to be higher” than similar numbers reported by Respironics machines and software. This has caused some concern and confusion, particularly in light of the frequently repeated “guidance” that the “goal” of PAP therapy should be an AHI of 5.0 or less. ResMed users in particular have reportedly been troubled by an inability to meet that “goal.”
There are two common explanations for the difference in AHI numbers between the two machine manufacturers.
1) The concepts of “apnea” and “hypopnea” are defined, and thus measured and reported, differently by the two manufacturers. This affects both CPAP and AutoPAP.
2) At least in part as a result of this, but also due to other intentional differences, the AutoPAP algorithms of the two manufacturers behave differently, producing different results.
RestedGal, in a very practical effort to allay undue concerns about this “5.0 goal,” has at various times suggested that ResMed users might “mentally” divide their HI in half, and then add it to their AI, to arrive at an “adjusted” AHI which might be more “comparable” to the numbers produced by Respironics. This suggestion has been met with the criticism that it implies that Respironics numbers are “right” in a way which makes the ResMed numbers “wrong.”
Respironics and Variable Breathing
Muffy, in the post cited above, argued very cogently that, in fact, the Respironics numbers may be “wrong” because of Variable Breathing issues. She hypothesized that not only did Respironics machines identify and collect Variable Breathing data (though their reports never mentioned these data), but that the Variable Breathing construct was in fact being used by Respironics machines. Possibly, Variable Breathing was an active factor in the Respironics AutoPAP algorithm. In addition, Variable Breathing, Muffy hypothesized, affected the way both CPAP and AutoPAP machines actually reported apneas and hypopneas.
If accurate, this would constitute a THIRD and largely unrecognized mechanism underlying the difference between AHI numbers for the two manufacturers:
3) When Respironics machines detect Variable Breathing, they DO NOT REPORT apneas or hypopneas which might otherwise be present, according to their definitions of these events.
In response to Muffy’s hypothesis, I spot-checked a number of my own Respironics data collections (in both CPAP and AutoPAP modes). I have found no situations in which her hypothesis was incorrect. While this does not confirm its accuracy, I find it to be very convincing. And very disturbing.
An Example
I offer the following example, selected because of the high density of respiratory events. Several weeks ago I intentionally created a situation in which I would have VERY high AI and HI numbers during therapy with a Respironics M-Series AutoPAP machine, set in fixed-pressure CPAP mode. (I was paying no attention to Variable Breathing at the time).
My AHI was 37.7 over a 6h:22m blower time, consisting of an AI of 8.8 (56 events) and an HI of 28.9 (183 events). Yes, terrible. On re-analysis, with a specific view toward Variable Breathing, this condition was present for 5h:3m, or 80.7% of the total blower-on time.
But here is the key. During any timeframe (Respironics reports respiratory events in 30-second time windows) in which Variable Breathing was reported, NO OTHER respiratory event was reported.
The following link (I provide it as a url link to an Excel spreadsheet rather than as an image due to its length; it is safe to open it) shows “raw” Respironics data for a period of a bit over an hour. There are 136 time-stamped data points. Ten reflect apneas. Forty reflect hypopneas. Eighty one reflect Variable Breathing. All but five show events: exactly ONE event each.
Look at the patterns. Look at how apneas and hypopneas “pop out” when Variable Breathing is not reported. And ask: is it more likely that there were no apneas or hypopneas during Variable Breathing periods, or is it more likely that Variable Breathing is SUPPRESSING the reporting of apnea and hypopnea events?
http://velbor.home.comcast.net/cpap/cpap_vb.xls
Implications
If we conclude that Respironics “Variable Breathing” suppresses the reporting (and the inclusion in AHI statistics) of apneas and hypopneas, it changes how we must think about what these numbers mean. (It does not - necessarily - change our standards for “adequate therapy.”
My own typical spending of about 1/3 of the night in Variable Breathing may be different from what others experience. The link about Variable Breathing referenced earlier includes a “questionnaire” regarding frequency of occurrence through the night; in real time the distribution is:
viewtopic.php?f=1&t=36541&start=0&st=0& ... w=viewpoll
This is a new twist which should be discussed and absorbed, and I invite comments to this thread to begin the process.
Velbor
Re: ResMed vs. Respironics: AHI and Variable Breathing
Still reading the other thread...man, my brain is so slow compared to before my loose lips adventure! Might have something intelligent to add when I've digested that thread. This is a bump for interested forum members.
ResMed S9 range 9.8-17, RespCare Hybrid FFM
Never, never, never, never say never.
Never, never, never, never say never.
Re: ResMed vs. Respironics: AHI and Variable Breathing
Cool. Maybe the variable breathing thingy in the Respironics machines is what it uses to say "I can't find what I consider a good baseline."
I don't think of any brand of machine as overscoring or underscoring, myself. I think of machine-estimated numbers as being a way to see if things are getting better or worse while using that one brand of machine.
I have always thought that "real" apneas and hypopneas were ones that were scored as such during a PSG by a good scorer and that any home machine is only giving an estimate (since it is only going by flow) and that none of the numbers directly compare to a PSG (which tracks arousals and O2) but that the estimates are still very useful for trending.
I don't think of any brand of machine as overscoring or underscoring, myself. I think of machine-estimated numbers as being a way to see if things are getting better or worse while using that one brand of machine.
I have always thought that "real" apneas and hypopneas were ones that were scored as such during a PSG by a good scorer and that any home machine is only giving an estimate (since it is only going by flow) and that none of the numbers directly compare to a PSG (which tracks arousals and O2) but that the estimates are still very useful for trending.
Re: ResMed vs. Respironics: AHI and Variable Breathing
Velbor --
Thanks for another thought-provoking and well constructed post. It certainly seems that you and Muffy are on to something.
I only have limited experience with data, and with ResMed]s data, at that. But I do have a question. Can Respironics machines report more than one event per 30-second interval? I don't see a single example of that in your Excel file.
Keep up the good work.
Thanks for another thought-provoking and well constructed post. It certainly seems that you and Muffy are on to something.
I only have limited experience with data, and with ResMed]s data, at that. But I do have a question. Can Respironics machines report more than one event per 30-second interval? I don't see a single example of that in your Excel file.
Keep up the good work.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: DreamWear Nasal CPAP Mask with Headgear |
jeff
Re: ResMed vs. Respironics: AHI and Variable Breathing
Respironics data structure, as I see it in the .xml files produced by EncoreViewer, is anchored by the the 0:00:00 first blower-on relative start time. Some data timing is flexible: subsequent blower-off and blower-on events will be precise to the second. Most data timing, though, appears rigidly linked to blower-on times. Pressure and leak values are posted EVERY 30 seconds. (I have no idea whether it's the mean value or the "final" value; I doubt that it's the maximum value for the period.) Respiratory events, if and when they occur, are posted at the same 30-second intervals as pressure and leak. Regarding apnea, hypopnea, and flow limitation, I've never seen more than one recorded for any single time-window. (Respironics does not report or record the duration of any of these events. In theory, one could have two - or even just barely three - apneas in 30 seconds, or a combination of events. Nor do I know how Respironics "keeps score" if an apnea, for example, starts during one data window and continues into another.) My working presumption, based on what I see, is that, for respiratory events, Respironics simply notes the presence of the "worst" event to occur during the window. Vibratory Snore is different; its presence can be noted simultaneously with an A, H or FL. I had assumed that Variable Breathing would work similarly to Vibratory Snore, but based on my observation, it does not. It seems to take reporting precedence even over an apnea.jdm2857 wrote: But I do have a question. Can Respironics machines report more than one event per 30-second interval?
ResMed data structure, as I know it from the "export" (to Excel) function of AutoScan 5.7, is different. Pressure and leak values are posted EVERY one minute. (Again, precisely WHAT the numbers reflect is unclear to me.) Apneas and hypopneas are also posted for the minute in which they occur. Hypopneas are posted simply as having occurred. Apneas are posted with their duration in seconds. I have seen up to three apneas posted as occurring during the same minute, as well as combinations of A and H. (I do not think that multiple apneas during one minute are accurately handled by the software graphics.) And again I am not certain how reporting deals with events starting during one window and extending into another time window. Unfortunately, ResScan software does not support this kind of detail data export to Excel. ResLink provides data every few seconds, but it's more trouble than its worth to get at the data underlying the ResLink graphs.
Both systems leave much to be desired by the ardent data-diver. Respironics gives data more often. ResMed gives (or more to the point, displays) pressure and leak data to greater precision, as well as giving apnea duration. Respironics data can be coaxed from an .xml file into Excel without too much difficulty; ResMed no longer provides that capability in ResScan.
You take what you can get, and make the most of it! Regards. Velbor
Re: ResMed vs. Respironics: AHI and Variable Breathing
Thanks once again.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: DreamWear Nasal CPAP Mask with Headgear |
jeff
Re: ResMed vs. Respironics: AHI and Variable Breathing
Certainly interesting and prob over my head. I know for myself I add my FL's to my AHI and feel best when AHI + FL < 1.
So no I don't use the AHI <5 guide and have to agree with JNK what we have is simply some measure we can use when not hooked up to all those diagnostic leads.
So no I don't use the AHI <5 guide and have to agree with JNK what we have is simply some measure we can use when not hooked up to all those diagnostic leads.
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: New users can't remember they can't remember YET! |
BeganCPAP31Jan2007;AHI<0.5
I have no doubt, how I sleep affects every waking moment.
I am making progress-NOW I remember that I can't remember

If this isn’t rocket science why are there so many spaceshots?
Be your own healthcare advocate!
I have no doubt, how I sleep affects every waking moment.
I am making progress-NOW I remember that I can't remember
If this isn’t rocket science why are there so many spaceshots?
Be your own healthcare advocate!
Re: ResMed vs. Respironics: AHI and Variable Breathing
Velbor wrote
I think your observations support another explanation: our Respironics machines only report ONE event per Time-Stamped (TS) 30-second interval and, when multiple events occur in a TS interval, have a priority scheme to decide which ONE to report in that TS interval. Respironics machines report a NRAH before an Apnea before a Hypopnea before a Flow Limitation before a Snore before a Variable breathing event. Note that Variable breathing is the lowest priority for reporting in a TS interval. A Variable Breathing "event" will ONLY be TS interval reported if no higher level events occurred in that TS interval. Our Respironics machines do provide a solution for keeping NRAH, Apnea, Hypopnea, FL, and Snore total counts accurate for a session just in case more than one event (other than VB) occurs in a 30-second reporting interval. Our machines keep an internal count for each event type (NRAH, Apnea, Hypopnea, Flow Limitation, or Snore) during a session and report these total event counts (without a time-stamp) at the end of each session. These internally recorded total counts are written to the SmartCard, transferred along with the voluminous TS event data, and stored in the EncorePro SQL database in a separate table (along with total time in Apnea and other session totals). These internally recorded #s are what EP shows in its Daily Details report (and these same #s are used and reported by EPA). The 30-second time-stamped events are ONLY used to build the Sleep Therapy Flags chart. However, this chart, when multiple events occur in a TS 30-second reporting interval are missing the "multiples". It is not your eyesight (or the resolution) why you can't see all the EP/EPA reported events as Tick marks - they are not there AS THE MULTIPLES ARE MISSING from the TS event data for the above stated design reason.The following link (I provide it as a url link to an Excel spreadsheet rather than as an image due to its length; it is safe to open it) shows “raw” Respironics data for a period of a bit over an hour. There are 136 time-stamped data points. Ten reflect apneas. Forty reflect hypopneas. Eighty one reflect Variable Breathing. All but five show events: exactly ONE event each.
Look at the patterns. Look at how apneas and hypopneas “pop out” when Variable Breathing is not reported. And ask: is it more likely that there were no apneas or hypopneas during Variable Breathing periods, or is it more likely that Variable Breathing is SUPPRESSING the reporting of apnea and hypopnea events?
_________________
| Machine: AirSense™ 10 CPAP Machine with HumidAir™ Heated Humidifier |
| Mask: ResMed AirFit™ F30 Full Face CPAP Mask with Headgear |
| Additional Comments: CPAP Auto with Min 10, Max 12, and OSCAR |
I live in my body. I know my body better than anyone else in the world. I may consult a medical professional for advice, but no one, and I do mean NO ONE tells me what I am permitted to do. - Kiralynx
Re: ResMed vs. Respironics: AHI and Variable Breathing
Cinco, thank you for your clear response, which cuts to the heart of the question. If I may rephrase the issue at hand, in line with your comment:cinco777 wrote: .... Respironics machines report a NRAH before an Apnea before a Hypopnea before a Flow Limitation before a Snore before a Variable breathing event. Note that Variable breathing is the lowest priority for reporting in a TS interval. A Variable Breathing "event" will ONLY be TS interval reported if no higher level events occurred in that TS interval. ....
-- Assuming that ONLY ONE of NRAH, OA, H, FL, VB is reported per 30-second time-stamped data-frame by Respironics (and this is supported by my observations as well, though I omit Vibratory Snore which I have often seen concurrently with an OA or other event)
-- The question at hand is the actual order of priority of reporting. Is it, as you suggest,
A) NRAH, OA, H, FL, VB
with Variable Breathing as the lowest in precedence, or is it
B) VB, NRAH, OA, H, FL
as hypothesized by Muffy and arguably supported by patent information?
I don't know that we can formally distinguish between the two options only by looking at the data itself, though the example I presented would have me leaning toward the second option. Can you identify a source, external to the data itself, which supports your understanding?
Many thanks for you help in clarifying this issue. Regards, Velbor
Re: ResMed vs. Respironics: AHI and Variable Breathing
Velbor wrote
Additionally, since starting CPAP, I no longer snore. Since June 1st, only seven snore (VS events) have been recorded, and six of them took place within the first minute of a session leading me to believe that they resulted from my hose rubbing against the headboard when I was getting into bed and finding a comfortable sleeping position. Velbor noted above that he has observed that a snore (VS event) and a VB event were recorded in a single 30-second time-stamped (TS) interval. With my low VB% and few snore (VS events), I have not seen this occur where a VB event and VS event(s) are reported within the same 30-second time interval.
Since March '09, I have now seen 14 occurences where the EP/EPA reported counts (from the machines internal event counters) are greater than the number of TS events for the same session. I have observed differences for OA, Hypopnea, FL, and Snores (I do not experience centrals, NRAH). I attribute these occurences to the fact that "multiple" events are occuring (rarely) within a 30-second reporting interval and, by Respironics hardware/software design, are not being recorded in the Time-stamped 30-second interval records written on the SmartCard and subsequently loaded into the Encore Pro SQL database tables.
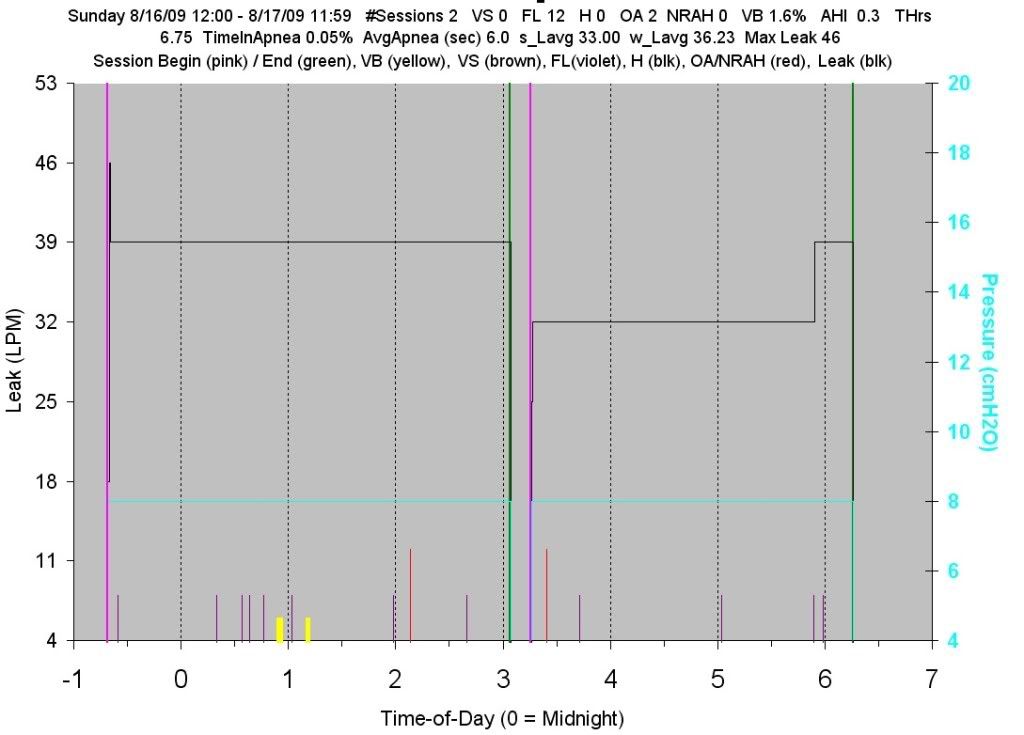
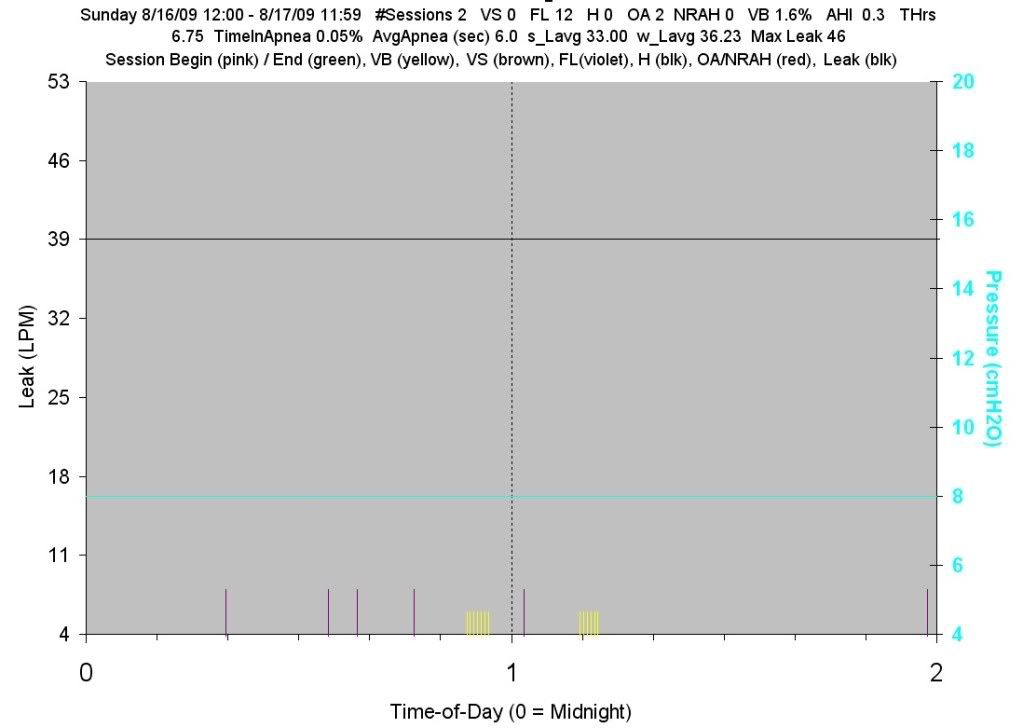
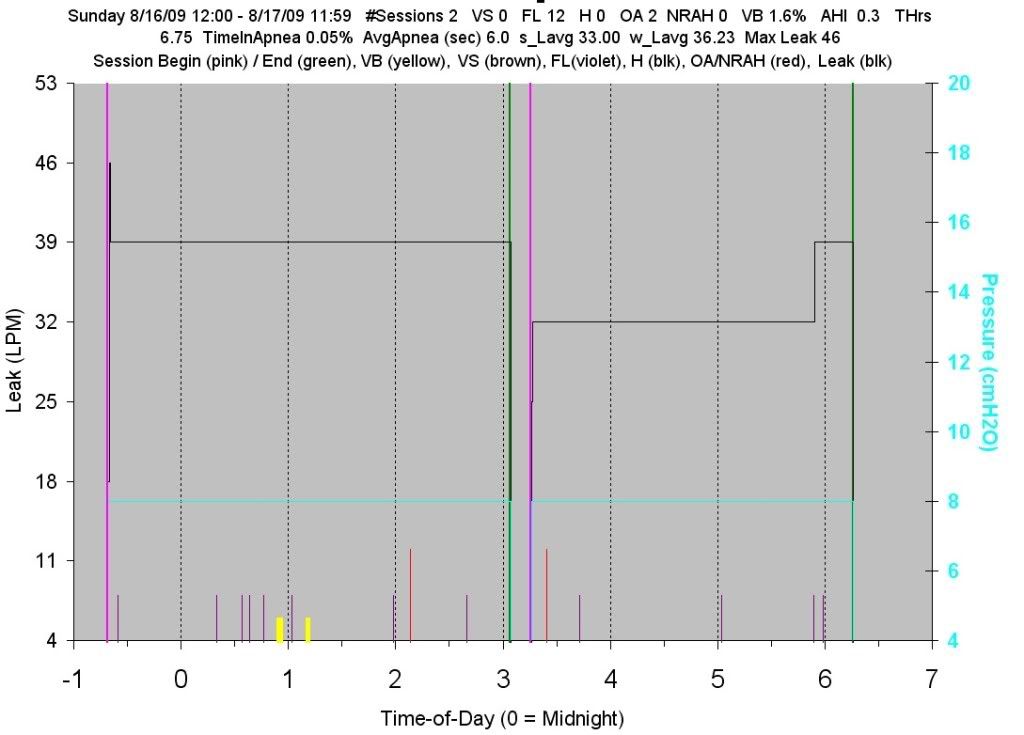
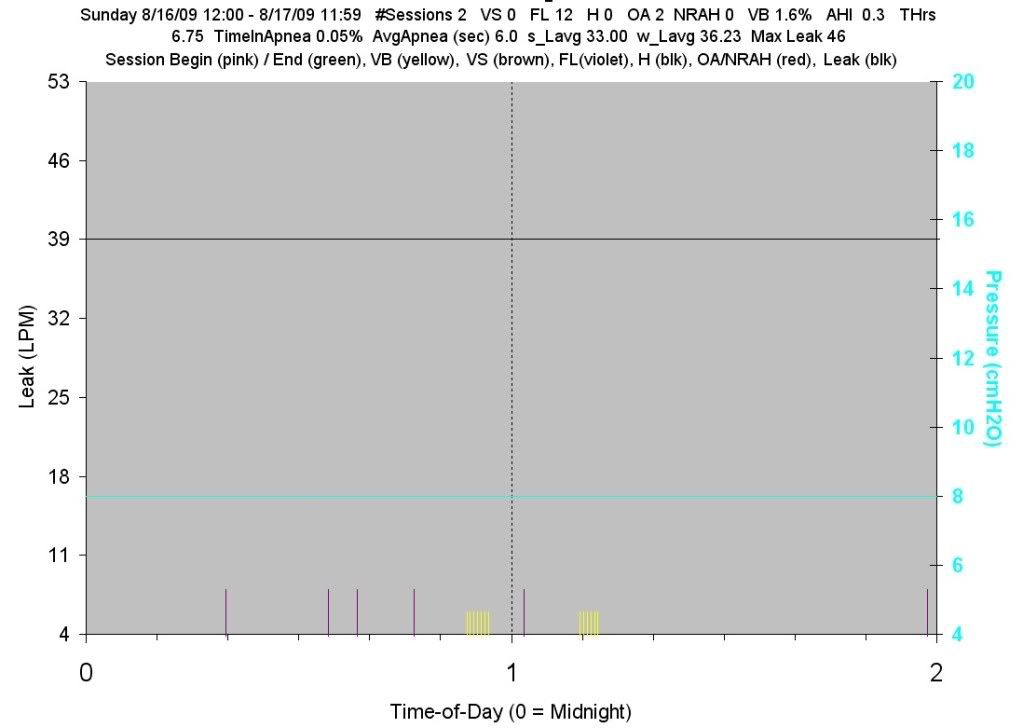
My Variable Breathing experiences/observations create a very different baseline than Velbor's. I started CPAP in March '09. In April, my Variable Breathing % (VB%) was usually above 20% with one night above 50%. NOW, 4 1/2 months later, my VB% is usually less than 10% with last month's average less than 5%. My VB % for last night (see attached chart) was 1.6% which, while low, is one of three nights this month where my VB% was less than 2%. In reviewing my observations, please note that my typical VB% is less than 1/6 what Velbor experiences.My own typical spending of about 1/3 of the night in Variable Breathing may be different from what others experience.
Additionally, since starting CPAP, I no longer snore. Since June 1st, only seven snore (VS events) have been recorded, and six of them took place within the first minute of a session leading me to believe that they resulted from my hose rubbing against the headboard when I was getting into bed and finding a comfortable sleeping position. Velbor noted above that he has observed that a snore (VS event) and a VB event were recorded in a single 30-second time-stamped (TS) interval. With my low VB% and few snore (VS events), I have not seen this occur where a VB event and VS event(s) are reported within the same 30-second time interval.
Since March '09, I have now seen 14 occurences where the EP/EPA reported counts (from the machines internal event counters) are greater than the number of TS events for the same session. I have observed differences for OA, Hypopnea, FL, and Snores (I do not experience centrals, NRAH). I attribute these occurences to the fact that "multiple" events are occuring (rarely) within a 30-second reporting interval and, by Respironics hardware/software design, are not being recorded in the Time-stamped 30-second interval records written on the SmartCard and subsequently loaded into the Encore Pro SQL database tables.
_________________
| Machine: AirSense™ 10 CPAP Machine with HumidAir™ Heated Humidifier |
| Mask: ResMed AirFit™ F30 Full Face CPAP Mask with Headgear |
| Additional Comments: CPAP Auto with Min 10, Max 12, and OSCAR |
I live in my body. I know my body better than anyone else in the world. I may consult a medical professional for advice, but no one, and I do mean NO ONE tells me what I am permitted to do. - Kiralynx
Re: ResMed vs. Respironics: AHI and Variable Breathing
If you have noticed fewer OA events in the detail than in the totals, and have not had any NRAHs, then the top of the priority order for the recording of detail events can't be NRAH followed by OA, can it?
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: DreamWear Nasal CPAP Mask with Headgear |
jeff
Re: ResMed vs. Respironics: AHI and Variable Breathing
Velbor wrote
I just printed the two patent articles and will read them this afternoon. I have read other patent articles related to VB but these two are new to me.
Regarding your question as to why I believe that VB is the lowest priority in reporting sleep events rather than the highest, I have to revisit what led me to this belief/conclusion. Some initial thoughts on why? follow:
First, VB events suppressing (being a higher priority) than OAs, etc., defies common sense and logic. Why would Respironics with, I assume, many smart CPAP people, place VB events (that cause no air/oxygen loss to a CPAP user) at a higher priority for reporting than NRAH/Apnea/Hypopnea/Flow Limitations that do.
Second, during my first month of using CPAP, I noticed that my laying awake in bed either before falling asleep or after awakening could generate numerous Apnea events. These were included in my AHI calculation and I also put them in a separate category that I labeled "False Apneas". Since April, the number of "False Apneas" has trended down so that they are now rare. Since I made tens of changes since March to my CPAP "sleeping habits", I don't have definitive proof on which change(s) made them mostly disappear. I suspect, however, that my breathing is now much more regular and relaxed when I am laying awake in bed as I am no longer anxious about my mask, about the pressure, about any noise (I keep a table fan on medium speed while I am in bed), etc. I now feel that my breathing (and heart rate) is more even and regular and these physiological changes led to the now rare occurrence of "false apneas".
Third is my observation that our Respironics machines maintain an internal counter to capture "multiples" that occur within a single TS 30-second interval.
That IS the question!-- The question at hand is the actual order of priority of reporting. Is it, as you suggest,
A) NRAH, OA, H, FL, VB
with Variable Breathing as the lowest in precedence, or is it
B) VB, NRAH, OA, H, FL
as hypothesized by Muffy and arguably supported by patent information?
I just printed the two patent articles and will read them this afternoon. I have read other patent articles related to VB but these two are new to me.
Regarding your question as to why I believe that VB is the lowest priority in reporting sleep events rather than the highest, I have to revisit what led me to this belief/conclusion. Some initial thoughts on why? follow:
First, VB events suppressing (being a higher priority) than OAs, etc., defies common sense and logic. Why would Respironics with, I assume, many smart CPAP people, place VB events (that cause no air/oxygen loss to a CPAP user) at a higher priority for reporting than NRAH/Apnea/Hypopnea/Flow Limitations that do.
Second, during my first month of using CPAP, I noticed that my laying awake in bed either before falling asleep or after awakening could generate numerous Apnea events. These were included in my AHI calculation and I also put them in a separate category that I labeled "False Apneas". Since April, the number of "False Apneas" has trended down so that they are now rare. Since I made tens of changes since March to my CPAP "sleeping habits", I don't have definitive proof on which change(s) made them mostly disappear. I suspect, however, that my breathing is now much more regular and relaxed when I am laying awake in bed as I am no longer anxious about my mask, about the pressure, about any noise (I keep a table fan on medium speed while I am in bed), etc. I now feel that my breathing (and heart rate) is more even and regular and these physiological changes led to the now rare occurrence of "false apneas".
Third is my observation that our Respironics machines maintain an internal counter to capture "multiples" that occur within a single TS 30-second interval.
_________________
| Machine: AirSense™ 10 CPAP Machine with HumidAir™ Heated Humidifier |
| Mask: ResMed AirFit™ F30 Full Face CPAP Mask with Headgear |
| Additional Comments: CPAP Auto with Min 10, Max 12, and OSCAR |
I live in my body. I know my body better than anyone else in the world. I may consult a medical professional for advice, but no one, and I do mean NO ONE tells me what I am permitted to do. - Kiralynx
Re: ResMed vs. Respironics: AHI and Variable Breathing
jdm2857 wrote
Please elaborate/explain your question/statement. Thanks.If you have noticed fewer OA events in the detail than in the totals, and have not had any NRAHs, then the top of the priority order for the recording of detail events can't be NRAH followed by OA, can it?
_________________
| Machine: AirSense™ 10 CPAP Machine with HumidAir™ Heated Humidifier |
| Mask: ResMed AirFit™ F30 Full Face CPAP Mask with Headgear |
| Additional Comments: CPAP Auto with Min 10, Max 12, and OSCAR |
I live in my body. I know my body better than anyone else in the world. I may consult a medical professional for advice, but no one, and I do mean NO ONE tells me what I am permitted to do. - Kiralynx
Re: ResMed vs. Respironics: AHI and Variable Breathing
Event hierarchy is not necessarily the point of the Muffpothesis. The Muffpothesis offers a possible explanation why some patients may have HI Respironics < HI ResMed, namely, potential events are excluded by VB in the Respironics algorithm that may otherwise appear as hypopneas in the ResMed algorithm:Velbor wrote:The question at hand is the actual order of priority of reporting. Is it, as you suggest,
A) NRAH, OA, H, FL, VB
with Variable Breathing as the lowest in precedence, or is it
B) VB, NRAH, OA, H, FL
as hypothesized by Muffy and arguably supported by patent information?
However, you have to actually be in VB Layer before event scoring is suspended (The Muffpothesis), and further, you have to actually be breathing (apneas supersede VB) so this is restricted to hypopneas.Muffy wrote:I have recently had the opportunity to observe a patient with highly erratic breathing noted on NPSG, that when placed on a ResMed unit, exhibited a relatively high HI (and AI, for that matter). Arguably, there were few "scorable events" in NSPG, as well as confounding wake and sleep transition. Close examination of the defining window(s) for the determination of the calculation of "baseline" (key to hypopnea identification) is pending.
However, I believe that "erratic breathing" is the key as to why some ResMed users exhibit higher relatively high(er) HI when compared to Respironics. I am hypothesizing that it is the Variable Breathing Controller in the Respironics algorithm that acts as a filter for erratic breathing. As I understand the operation of the VB Layer, event scoring is suspended. Without this filter, events are scored, as would be seen in A10.
And since A10 requires flow limitation and/or snoring in order to score hypopnea, the most important consideration here is that the events excluded in the Respironics algorithm are done so erroneously by VB.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: ResMed vs. Respironics: AHI and Variable Breathing
If the total OA from the summary data is greater than the total number of OA events in the detail data, then some other event must have priority over OA in the detail data. That higher priority detail event would be recorded, eclipsing the missing OA detail event. Otherwise summary total OA would alway equal the total number of OA details.
Since you have no NRAH events that event type cannot be the higher priority detail event in this example. So some other event type must have higher priority than OA
Since you have no NRAH events that event type cannot be the higher priority detail event in this example. So some other event type must have higher priority than OA
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: DreamWear Nasal CPAP Mask with Headgear |
jeff












