I had obstructive apnea during my first sleep study my AHI was about 27. I did have a few centrals but it was only 2% (4) and .5% (1)of them were mixed so mostly obstructive 97.5% (189). I had 5 awakenings and normal sleep architecture and no electromyographic abnormalties.
During my titration two weeks latter I had central apnea. I only had one obstruction and it was during the very begining of the study. They increased the pressures and i continued to have the centrals. They then did a bilevel titration for a while (I didn't have any centrals on this part) they then put me at an even higher level presure and determined I stoped snoreing and the was my pressure to use.
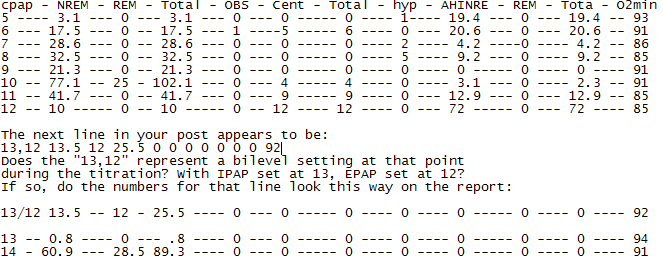
cpap NREM REM Total OBS Cent Total hyp AHINRE REM Tota O2min
5 3.1 0 3.1 0 0 0 1 19.4 0 19.4 93
6 17.5 0 17.5 1 5 6 0 20.6 0 206 91
7 28.6 0 28.6 0 0 0 2 4.2 0 4.2 86
8 32.5 0 32.5 0 0 0 5 9.2 0 9.2 85
9 21.3 0 21.3 0 0 0 0 0 0 0 91
10 77.1 25 102.1 0 4 4 0 3.1 0 2.3 91
11 41.7 0 41.7 0 9 9 0 12.9 0 12.9 85
12 10 0 10 0 12 12 0 72 0 72 85
13,12 13.5 12 25.5 0 0 0 0 0 0 0 92
13 0.8 0 .8 0 0 0 0 0 0 0 94
14 60.9 28.5 89.3 0 0 0 0 0 0 0 91
I have used cpap for 5 weeks I didn't feel any better using it and had a high leak rate. Using full face masks and the liberty. My AHI is around 5.
I just got a hybrid mask and will see if it helps but I really have trouble breathing out without leaking. I had this problem during the study I had to get help replaceing the mask on my face at least 3 times and woke up 14 times.
Any ideas on what to try? My doctor will not let me use auto on the machine or a lower pressure. I have the M series auto with cfex and heated humidifier. The cfex is on 3.
Central apnea during titration
- blackvelvet
- Posts: 11
- Joined: Tue Jan 29, 2008 5:30 pm
- Location: Idaho
Centrals at the onset of sleep is pretty common, you almost have to ignore the first 30 minutes or so of sleep. Some machines even have a feature for getting past this period called settling.
Your machine has it built-in but it only lasts about 20 minutes. You can extend that by using the Auto:Ramp feature.
To access your menu, hold down the <- -> keys at the same time while plugging in the power at the back, then press the + key and follow the LCD.
Your numbers listed don't really mean anything I can use to see what was happening. But from what you describe, my guess is you would do better keeping your pressure at or below 9.0 and ignoring that snoring. Chasing snores when you are at risk of Central Apnea is the wrong thing to do in my opinion.
Sometimes you cannot eliminate snores with pressure if they are associated with the soft palate.
Check your pressure settings, I would set Auto:Min to something comfortable like 6.5 or 7.0 and set Auto:Max=9.0 and use CFlex setting of 2, try it for a few nights and compare to what you have been getting.
You can clear the Therapy menu data (doesn't erase whats on the card) by holding down the (-) key for 5 seconds when the Therapy menu is displayed.
Press the On/Off button to exit setup mode, settings are all menu driven so it is pretty easy to set.
Your machine has it built-in but it only lasts about 20 minutes. You can extend that by using the Auto:Ramp feature.
To access your menu, hold down the <- -> keys at the same time while plugging in the power at the back, then press the + key and follow the LCD.
Your numbers listed don't really mean anything I can use to see what was happening. But from what you describe, my guess is you would do better keeping your pressure at or below 9.0 and ignoring that snoring. Chasing snores when you are at risk of Central Apnea is the wrong thing to do in my opinion.
Sometimes you cannot eliminate snores with pressure if they are associated with the soft palate.
Check your pressure settings, I would set Auto:Min to something comfortable like 6.5 or 7.0 and set Auto:Max=9.0 and use CFlex setting of 2, try it for a few nights and compare to what you have been getting.
You can clear the Therapy menu data (doesn't erase whats on the card) by holding down the (-) key for 5 seconds when the Therapy menu is displayed.
Press the On/Off button to exit setup mode, settings are all menu driven so it is pretty easy to set.
someday science will catch up to what I'm saying...
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Did your doctor say "why" he will not "let" you use auto mode? Do you have COPD or CHF? Auto-titration is perhaps not a good idea for some people with either of those conditions.blackvelvet wrote:My doctor will not let me use auto on the machine or a lower pressure.
Some centrals that pop up in a titration are temporary and subside when the body adjusts to a change in pressure. Those wouldn't mean a person "has Central Apnea" as a sleep breathing disorder.
Is this more like the way the numbers in your report are spaced out?
I'm no doctor. Neither is Snoredog, as he'd be quick to tell you. It looks to me like the doctor ordered one of the higher pressures in your titration because of the pretty drastic drop in O2 (85) during the almost one hour spent at pressures of 11 and 12.
The pressure of 9 doesn't represent any time spent in REM, and the doctor probably also wanted to see an effective pressure during REM -- which he saw during the time spent at 10 and at 14. I don't mean that those pressures made you have REM or let you have REM. It's just that seeing if a pressure can be effective during REM is good information.
I'd have probably picked the pressure of 10, since there was some REM to see during 10, and the O2 was above 90. I'd have discounted those 4 centrals there -- especially if they occurred soon after the pressure was raised to 10 and subsided as the time at the pressure went on.
But, I'm not a doctor, nor a sleep tech, nor a fly on the wall. I kind'a bet though, that the tech's reported mentioned 14 as being "the effective pressure" and...well, busy doctors do just glance at what the tech wrote and sign off on it...imho. Not that there was anything wrong with "14". Neither the tech nor the doctor have to wear a mask or have a machine blowing at them all night, probably. They'd feel the difference if they did.
If 10 will give as effective treatment as 14 (I'm not a doctor, so I don't know) that would be a much easier pressure for you AND a mask to deal with.
If it were me, I'd turn on auto mode and set it for 10 - 15, with C-flex set at 3. But that's just me.
By the way, does your M Auto machine happen to have the words "A-Flex" written on top? If so, I'd set it for auto with A-flex (rather than C-Flex) set at 3.
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
I'd also be sure to get the readings on the smart card for a week or so on those pressures. They'd tell you what you need to know.rested gal wrote:If it were me, I'd turn on auto mode and set it for 10 - 15, with C-flex set at 3. But that's just me.
I'm no doctor either, but I don't think it's the end of the world to stumble around a bit while looking for the perfect pressure, especially given those study results. If it's not ideal, then you can always bump it up to your scrip and see how you do then. Just remember not to take one night as conclusive proof of anything. Do a few and watch the general trends.
Of course another way you could do it is to start at the prescribed pressure and make small adjustments down and wait a week or so to see how you're going.
Or you could simply take what the prescription says and set your machine there and forget about it. Basically remember that treatment is better than no treatment, even if it's not 100% perfect. The important thing to do is to get into a routine, get comfortable with the machine, and start getting some air in your lungs. Getting it perfect can come later. It's up to you.
Personally I'd start at the lower pressure range around 10 - 15 auto and work my way higher if needed. While you're still adjusting to this it's harder to take the higher pressures especially.
I'm a programmer Jim, not a doctor!
- blackvelvet
- Posts: 11
- Joined: Tue Jan 29, 2008 5:30 pm
- Location: Idaho
I don't know if I have either COPD or CHF but I would guess not I'm 26 and mostly healthy aside from allergies and the obstructive sleep apnea. The snoring and daytime sleepyness got me to go in and get the sleep study.
My doctor said that autos don't work and can not tell you anything about your sleep. He also doesn't care what my card said as far as thearapy results but he said if I change it to auto he will tell my insurance I'm non compliant and they will stop paying for the machine.
He owns the sleep lab though and tried to get me to go do another sleep study to see if I could go on bipap instead but I don't have the 1000 for my copay at this time.
There is a graph on the next page of the report that shows when the events occured the centrals on a setting of ten where about 30-60 min into the pressure and I was dreaming after that point untill the pressure changed again waking me up.
I'm looking for another doctor that can work with me and wants to tell me why they are setting the pressures the way that they are.
I also have been using the ramp at home it was set for 45 min so by the time I get to pressure I'm asleep.
My doctor said that autos don't work and can not tell you anything about your sleep. He also doesn't care what my card said as far as thearapy results but he said if I change it to auto he will tell my insurance I'm non compliant and they will stop paying for the machine.
He owns the sleep lab though and tried to get me to go do another sleep study to see if I could go on bipap instead but I don't have the 1000 for my copay at this time.
There is a graph on the next page of the report that shows when the events occured the centrals on a setting of ten where about 30-60 min into the pressure and I was dreaming after that point untill the pressure changed again waking me up.
I'm looking for another doctor that can work with me and wants to tell me why they are setting the pressures the way that they are.
I also have been using the ramp at home it was set for 45 min so by the time I get to pressure I'm asleep.
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
LOL... wow, what a "smart" doctor he is, making a blanket statement like that. I'm saying that sarcastically, of course.blackvelvet wrote:My doctor said that autos don't work
Reminds me of this:
Feb 19, 2005 subject: "Sleep Doctor" doesn't like autopaps
viewtopic.php?t=1461
True, an autopap can't give the kind of extensive data about your sleep that being wired up during a full PSG sleep study can. But he's kind'a rubbing apples and oranges together... almost implying that an autopap also cannot tell you anything about your continuous positive air pressure TREATMENT. Getting some nightly information about that is what's important at this point, imho.blackvelvet wrote: and can not tell you anything about your sleep.
If a person is using an autopap (or even a cpap) which has the capability to record more data than just "hours of use", we can get some useful information that can help us see if there might be problems in our treatment. VERY useful information, imho, about leaks and about AHI -- how many apneas and hypopneas are still sneaking though despite treatment.blackvelvet wrote:He also doesn't care what my card said as far as thearapy results
I can think of a lot of things I would tell him at that point. But I wouldn't bother wasting my breath. I'd find a new doctor -- one who didn't try to act like a god over YOUR life -- and never see that @#$% again. Doesn't have to be a sleep doctor. A regular family doctor can write the prescription -- the DME and insurance companies are fine with that.blackvelvet wrote:he said if I change it to auto he will tell my insurance I'm non compliant and they will stop paying for the machine.
That god-doctor may sincerely believe that "autopaps don't work" and that it's THAT important to keep you from using auto mode that he chooses to be a bully. But if he's willing to completely stop you from getting ANY kind of treatment at all even if it really were suboptimal treatment, then he's WAY out of line, imho.
He's got a great cash cow business going, and he knows it.blackvelvet wrote:He owns the sleep lab though and tried to get me to go do another sleep study to see if I could go on bipap instead but I don't have the 1000 for my copay at this time.
I'm not a doctor and not an expert by any means about "sleep studies." My hunch, though...and that's all it is...not a medical opinion, just a hunch...is that you really don't need to be worried about centrals. If "centrals" were really going to be a problem for you, they'd have continued showing up at those two final single high pressures that you spent plenty of time at, in the sleep study...imho.blackvelvet wrote:There is a graph on the next page of the report that shows when the events occured the centrals on a setting of ten where about 30-60 min into the pressure and I was dreaming after that point untill the pressure changed again waking me up.
If you don't find another sleep doctor who will work with you in that way, then...again, I'd find a sensible GP...General Practitioner...family doctor... who, even though he might not have any idea WHY the "sleep doctor" prescribed the pressure he did, might be willing to let YOU work with your pressures to see what seems to work effectively as well as comfortably for you.blackvelvet wrote:I'm looking for another doctor that can work with me and wants to tell me why they are setting the pressures the way that they are.
That's fine, if you need that easier start.blackvelvet wrote:I also have been using the ramp at home it was set for 45 min so by the time I get to pressure I'm asleep.
Me....well, while I was looking for another sleep doctor or a sympathetic GP, I'd go right ahead and set the machine for auto mode anyway. At a pressure range of 10 - 15. Even if I didn't have software to see how it's going. If in a week or two, or a month from now (if ever), anyone from the DME or doctor's office contacted me to bring or send the Smart Card in for a download, I'd say "ok."
But it just wouldn't happen to be convenient for me to make the trip in, and I'd "forget" to mail the card. I'd buy time, while using my machine the way I wanted to use it, until I found another doctor. That FIRST doctor would never see me again. Ever.
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435











