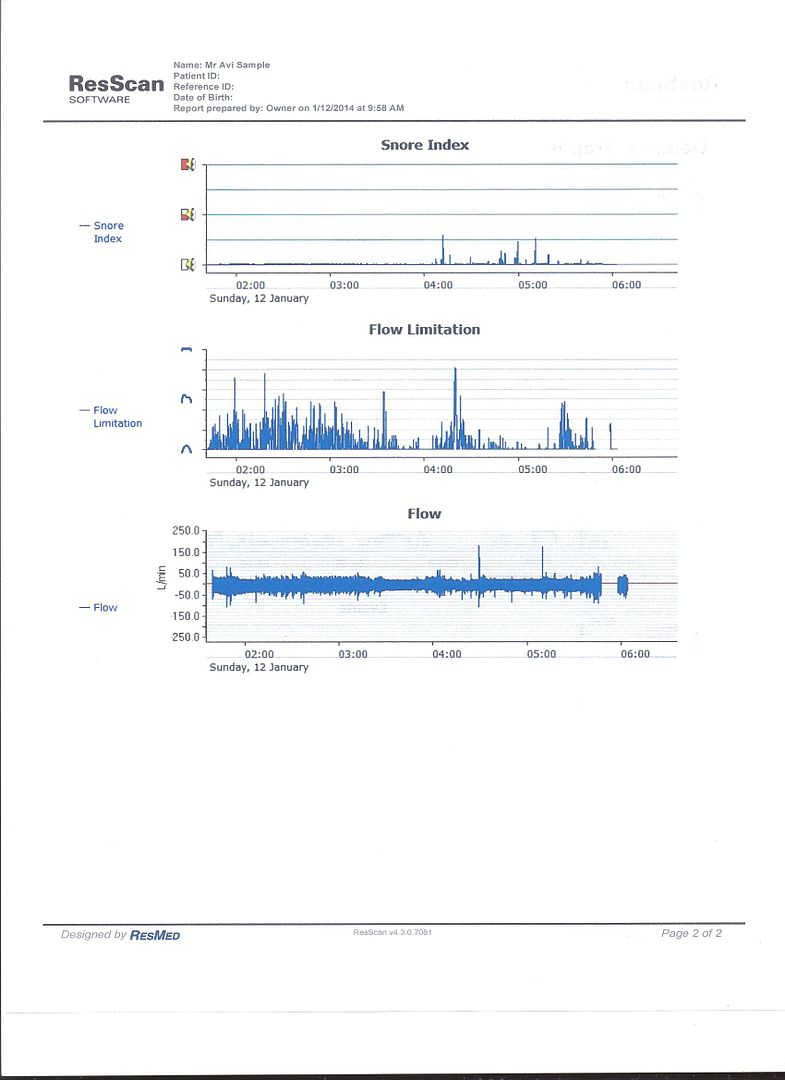
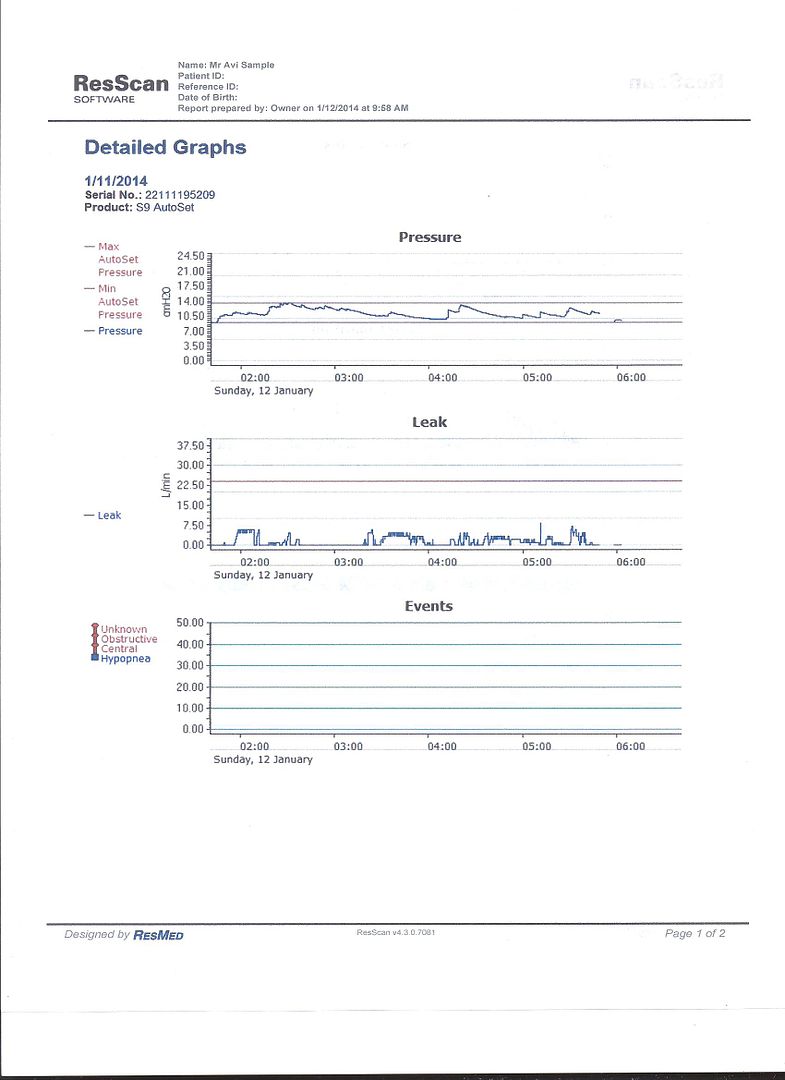
Den,Wulfman... wrote:And, in my opinion, the reason is of dubious value. One has to interrogate the reports to see how many FLs turn into Hypopneas, Snores or Apneas. Also, one should look to see how many snores precede apnea events.Pugsy wrote:I have to respectfully disagree.Wulfman... wrote:For all intents and purposes, "Flow Limitations" don't really matter much with regard to the therapy......they and Snores are what the APAPs use to trigger pressure changes.
When trying to figure out why a person is waking up (and we can't see any logical reason) I prefer to have all available information at my finger tips...just in case.
The FLs and UARS thing is always a possibility and even if remote....bears keeping one eye open.
After all...there is a reason why the apap mode will respond to a FL.
Many people have "frank" apneas (without preceding events) and will never get a pressure increase BECAUSE of the lack of preceding events.
Considering that these machines use "air flow" to interpret events, there are many things that a sleeper could do that would NOT be an actual event worth increasing pressure for. Just turning over or repositioning yourself could be interpreted as a flow limitation. The hose rubbing across the edge of the bed could be interpreted as a snore.
But, we were talking about straight pressure for this user and his sleep disturbances. Tracking FLs may be interesting to see how many times the machine didn't have to bump the pressure......but that's about it.
If Flow Limitations were that important, the machines would record them in CPAP mode, too. Yeah, I know, ResMed Elite machines do.......whoopie!
As far as UARS.......???
Upper Airway Resistance Syndrome (UARS) - part of the spectrum of obstructive sleep-related breathing disorders in which repetitive increases in resistance to airflow in the upper airway lead to brief arousals and daytime fatigue. Apneas and hypopneas (see RDI) may be totally absent. Blood oxygen levels can be in the normal range.
Den
.
You're missing Pugsy's point. Flow limitations by themselves can be disruptive to some people's sleep. That's the basic problem in untreated UARS: The FLs themselves lead to arousals before they are bad enough to be scored as a full-fledged hypopnea. And there are some sleep labs and some sleep docs who believe that during a titration study, the sleep tech who does the titrating should attempt to eliminate all the FLs well as the OAs, Hs, RERAs and snoring. In other words, there are some sleep med professionals who believe that a properly titrated CPAP pressure should be high enough to eliminate the FLs as well as the other stuff.
In light of that, it's not hard to see that if a person's titrated CPAP pressure is high enough to take care of the OAs and Hs, but low enough to allow a substantial number of FLs to continue to happen, then the residual FLs themselves could lead to problems in some OSA patients using straight CPAP. And that's why Pugsy is saying to eliminate the APAP variable by setting min Pressure = max Pressure in APAP mode: You get the benefits of a nonvarying pressure (if pressure changes are what is triggering the wakes) and you still get the FL data (in case its FL that are causing the wakes instead of the pressure changes.)
Are you aware that PR machines only record half the snoring data when in CPAP mode? Does that mean the VS2 snores are somehow more important than the VS snores?If Flow Limitations were that important, the machines would record them in CPAP mode, too.
In my (not so humble) opinion, PR made a stupid programming mistake when they chose to make their machines record only half the snore data and none of the FL data when their machines are run in CPAP mode.