I don't think there's any such thing as waking "naturally" for me. I always wake up more tired than I went to bed, never refreshed. So I have to use an alarm.mollete wrote:If one is waking up naturally, then it should occur at the end of the final REM period, so if one has 5 sleep cycles (each one approximately 90 minutes), they should end up with 7.5 hours of sleep. So perhaps a plan could be, figure out what time your day must begin and back up 7.75 hours (don't forget the 15 minutes it takes to fall asleep!) to figure bedtime.
Post-Surgery Blues: Scoring Question
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: Post-Surgery Blues: Scoring Question
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
Re: Post-Surgery Blues: Scoring Question
I may just give up for now. I can't handle this. My sanity is at its limits even with these naps, to the point that I am doing irrational stuff, so hopefully the oral appliance route or Provent or something will give me an upside.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
Re: Post-Surgery Blues: Scoring Question
Hello, Brian. I just read the meds you've already tried to help with xPAP intolerance:
https://www.google.com/search?q=tricycl ... 40&bih=561
search.php?keywords=amitriptyline
https://www.google.com/search?q=amitrip ... =firefox-a
Consider asking your doctor about trialing a TCA class med, like amitriptyline, before bedtime to help with xPAP tolerance. TCA's are sometimes prescribed in smaller doses prior to sleep to help with certain types of sleep-maintenance issues. They are also prescribed in slightly larger doses for day use as antidepressants.Occasionally and as needed: Ambien 5-10mg, Lunesta 3mg, Clonazepam 0.5mg-1mg. Since I'm not using the CPAP most of the time these days, I usually don't need to take any of these
https://www.google.com/search?q=tricycl ... 40&bih=561
search.php?keywords=amitriptyline
https://www.google.com/search?q=amitrip ... =firefox-a
Re: Post-Surgery Blues: Scoring Question
Thanks -SWS for weighing in. I'll ask the next time I see the docs. I'm slated to see an oral appliance dude next week. I'll probably see the sleep docs after that finishes out. I actually have no problems going to sleep on xPAP. (That's different from when I first started, when it was a real issue.) I sleep through most or all of the night (half the time, I wake up after about four hours -- and I either can't settle down and strip the mask, or can get back to sleep intact).
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
Re: Post-Surgery Blues: Scoring Question
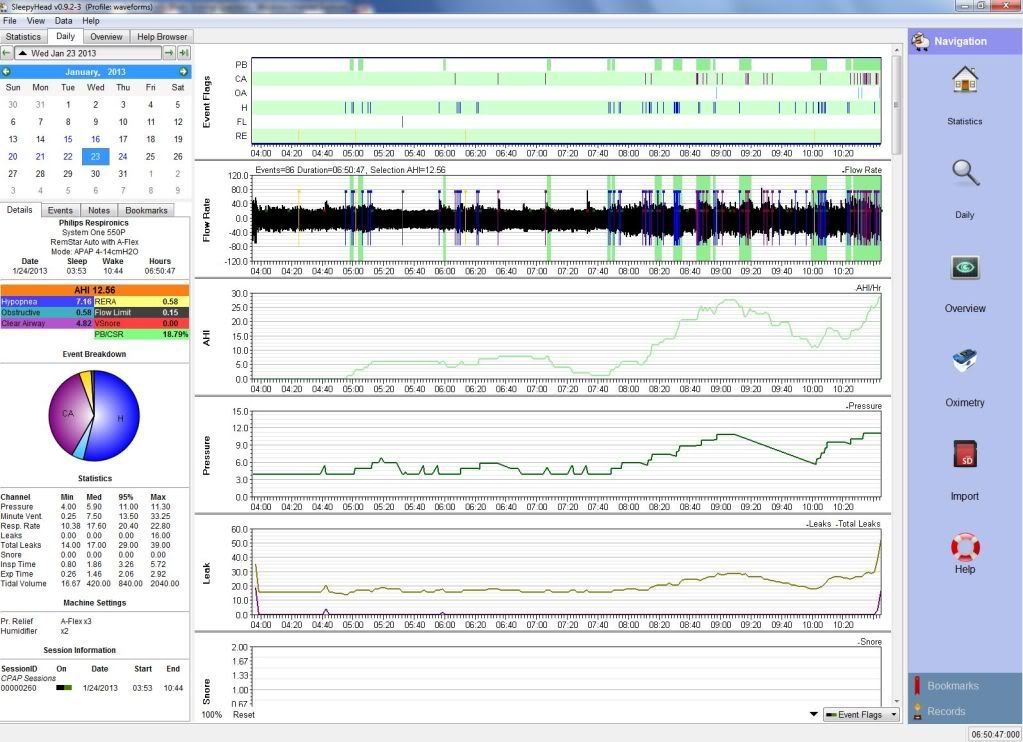
Well here's something new. Your screenshot of 1.23.2013:

And mine:
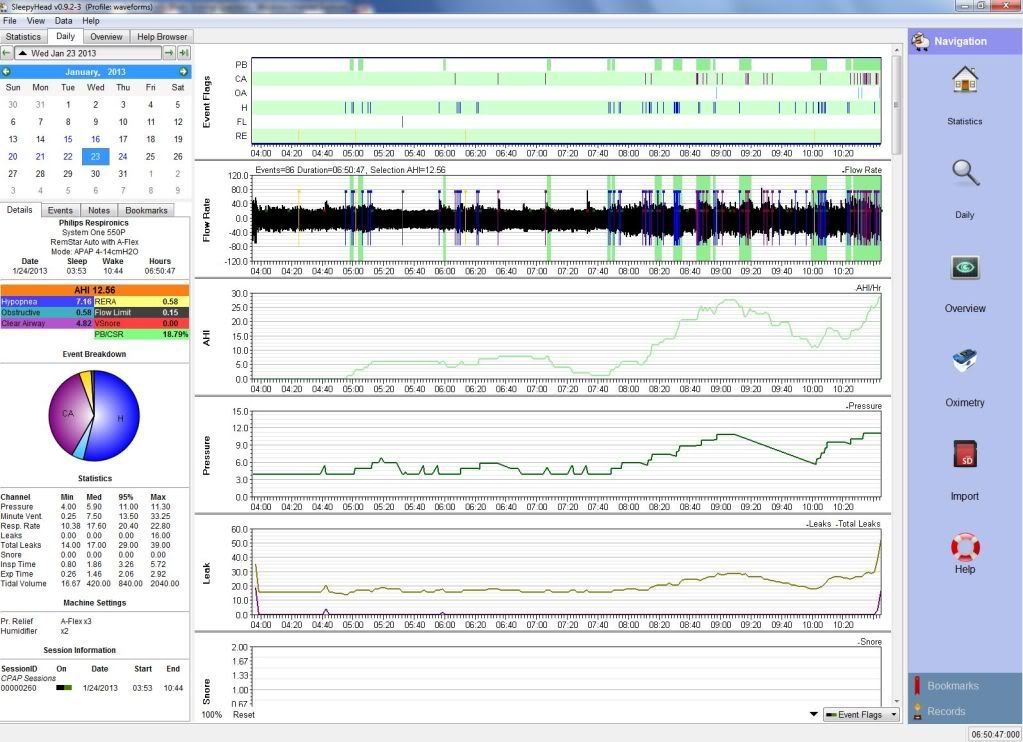
So you not be in Tennessee. You be in Caulifornia!

And mine:
So you not be in Tennessee. You be in Caulifornia!
Re: Post-Surgery Blues: Scoring Question
Given the above,

you look a little less like a shift worker.
That said, the huge variation in Lights Out, Sleep Time, Naps and Wake Up is still significant.
when reviewing the past couple of years:BrianinTN wrote:I thought my tolerances in terms of +/ on lights out and wake up weren't bad on average.mollete wrote: Take everything you're doing now and do the opposite.

you look a little less like a shift worker.
That said, the huge variation in Lights Out, Sleep Time, Naps and Wake Up is still significant.
Re: Post-Surgery Blues: Scoring Question
Hey, I hear ya! I can certainly understand what frustration can be like!BrianinTN wrote:I may just give up for now. I can't handle this. My sanity is at its limits...
Yeah, and some of your co-workers can have babies, but you can't do that either.BrianinTN wrote:As in exact same time every night and morning? C'mon, other than people in the military, who does that? In today's world, who can? The vast majority of people don't, and they function just fine. My classmates are grooving along with far nuttier schedules than me. So did most of my old coworkers.
Going back to the original point, I believe there's going to be some (much?)(total?) improvement in the Post-Surgical CompSAS if you give it some time.
Meanwhile, since CompSAS is largely fueled by pCO2 variability, I think Provent really may have an application here. One of the mechanisms that allows it to work is that rather than having exaggerated breathing and free flowing gas associated with xPAP therapy and decreasing pCO2 from ambient, breathing through the resistance offered by Provent may allow pCO2 increase:
This in turn might (theoretically) help with CompSAS, ameliorating that periodic breathing.David Rapoport, MD in an interview wrote:What other mechanisms were you able to identify?
If you impede breathing and don’t allow free exhalation, we generally do not think that has much of an effect on the total amount you breathe, but it turns out it can, especially with Provent—which has a fairly high resistance. While you’re asleep, some of your reflexes to control the level of breathing don’t function as well as they do while you’re awake. The level of CO2 in the blood rises slightly, and we were able to confirm that increased CO2 was present in patients who were breathing on Provent—both awake and asleep.
What happens when you raise CO2?
If you raise CO2 slightly, you increase the drive to breathe, and that normally compensates and produces a reflex increase in breathing. However, it also produces an increase in the amount of tone that is driven in the muscles that control the stiffness of the upper airway—and we think that might play a role.
It has been shown in other studies that giving CO2 externally does increase the stiffness of the upper airway, and the tone in the muscles, and may have a small effect on sleep apnea by itself. So this is creating the patient’s own CO2 and using that to raise the level in the blood—increasing the level of drive—and therefore the amount of stiffness in the upper airway.
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: Post-Surgery Blues: Scoring Question
Brian, try the Provent! When I tried it, it was absolutely liberating to go to bed with nothing on but a couple of stickers on my nose! How I wish it had worked for me...
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
Re: Post-Surgery Blues: Scoring Question
Let me toss in this old post to try to show the role of pCO2 in all this:
Here is an Adapt SV chugging merrily along (look at "ASV Pressure", which are the breaths going in), attacking central apneas with rapid pressure increases, and backing off during periods of increased patient ventilation:

Note the undulation of pCO2 (TcpCO2) here, otherwise known as The Root of All Evil. When the CO2 dips, respirations cease. When they rise, the patient (hyper)ventilates. Now, the CO2 waveform lags a little because of circulatory time (to the ear, where this is measured) and perfusion time (this is a transcutaneous electrode), but nonetheless, this really shows well what is happening.
Anyway, the goal is to ventilate through the central apnea to ameliorate the ventilatory overshoot. In other words, by controlling the central apnea, you control the ventilatory response, or the ensuing event. So, to our original point, it takes a little bit of time for this thing to catch:
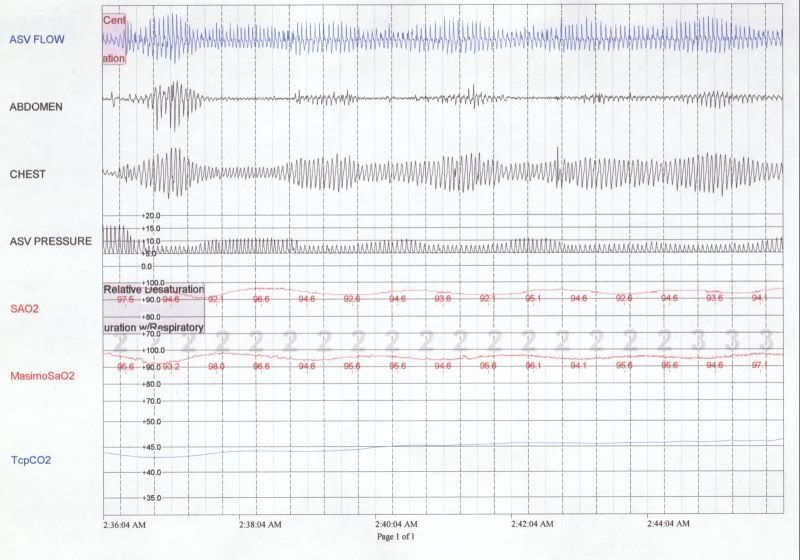
But eventually it does, pCO2 gets over apnea threshold and the cycle breaks:

It this particular CSBD attack, there's a salvo of at least 7 centrals alone. So, in your NPSG, we need to look for evidence of these "salvos".
ASV breaks the cascade of centrally-oriented events by by (1) successfully ventilating through the central apnea, increasing pressure rapidly to achieve a pre-calculated Target, but this Target, based on preceding minute ventilation, is less than what would be perceived by the body as "hyperventilation" and cause the cycling to perpetuate; and (2) avoiding overshoot during the ensuing respiratory cycle by pre-setting parameters to a low baseline. This results in a manipulation of the CO2 level that gets it above (central) apnea threshold, and keeps it there.Kiralynx wrote:But how DOES the ASV "break the cycle"?
Here is an Adapt SV chugging merrily along (look at "ASV Pressure", which are the breaths going in), attacking central apneas with rapid pressure increases, and backing off during periods of increased patient ventilation:

Note the undulation of pCO2 (TcpCO2) here, otherwise known as The Root of All Evil. When the CO2 dips, respirations cease. When they rise, the patient (hyper)ventilates. Now, the CO2 waveform lags a little because of circulatory time (to the ear, where this is measured) and perfusion time (this is a transcutaneous electrode), but nonetheless, this really shows well what is happening.
Anyway, the goal is to ventilate through the central apnea to ameliorate the ventilatory overshoot. In other words, by controlling the central apnea, you control the ventilatory response, or the ensuing event. So, to our original point, it takes a little bit of time for this thing to catch:
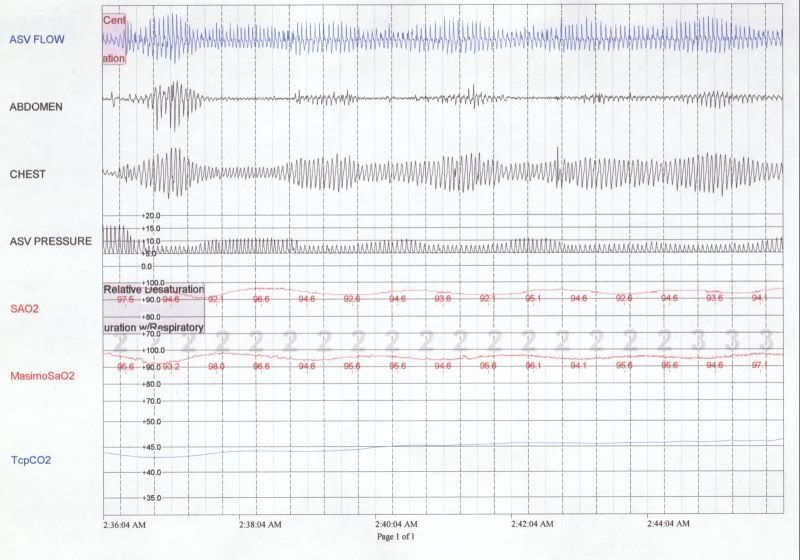
But eventually it does, pCO2 gets over apnea threshold and the cycle breaks:

It this particular CSBD attack, there's a salvo of at least 7 centrals alone. So, in your NPSG, we need to look for evidence of these "salvos".
Re: Post-Surgery Blues: Scoring Question
Now of course, what we're talking about is addressing SICs instead of PICs, so this is like a whole 'nother plane in using Provent to control PSCompSAS.
But if the Stanford guys buy into this and it works, they'll be the lead article in JCSM, and Provent will be your new best friend.
But if the Stanford guys buy into this and it works, they'll be the lead article in JCSM, and Provent will be your new best friend.
Re: Post-Surgery Blues: Scoring Question
1) The Stanford guys were not optimistic on ASV doing me much good. I can whip it out the old behemoth for a couple nights, but you don't get to see any of the breath-by-breath data with that POS. Would that be worthwhile? To my naive brain, the pCO2 regulation in the graphs and discussion you linked suggest that especially for me right now, with my overshoot/undershoot cycle, it might have merit. Check out this small sample from last night's AHI=11; I'd quickly reached the max pressure of 9.

2) On Provent, HealthNet does not appear to cover it, classifying it as "experimental" treatment. As Stanford's tuition costs have bled me dry, that's a major negative. By contrast, HealthNet's policy is surprisingly charitable toward oral appliances. Back when I was on BCBS, the rule was "if severe, no coverage." HealthNet has a provision for people who are moderate to severe but also are CPAP intolerant.
If the oral appliance (and possibly ASV) route fail, perhaps it's worth biting the bullet on the Provent, despite the expense. But I'd rather put myself in those shoes after exhausting the other insurance-subsidized routes.
As an addendum, check out Sunday night -- a real doozy. I've updated my original data link (https://dl.dropbox.com/u/15497133/P-Series.zip) in case you'd like to see the new stuff.


2) On Provent, HealthNet does not appear to cover it, classifying it as "experimental" treatment. As Stanford's tuition costs have bled me dry, that's a major negative. By contrast, HealthNet's policy is surprisingly charitable toward oral appliances. Back when I was on BCBS, the rule was "if severe, no coverage." HealthNet has a provision for people who are moderate to severe but also are CPAP intolerant.
If the oral appliance (and possibly ASV) route fail, perhaps it's worth biting the bullet on the Provent, despite the expense. But I'd rather put myself in those shoes after exhausting the other insurance-subsidized routes.
As an addendum, check out Sunday night -- a real doozy. I've updated my original data link (https://dl.dropbox.com/u/15497133/P-Series.zip) in case you'd like to see the new stuff.

_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
Re: Post-Surgery Blues: Scoring Question
Provent is 2 bucks a night. How much were those margaritas up there?BrianinTN wrote:On Provent, HealthNet does not appear to cover it, classifying it as "experimental" treatment. As Stanford's tuition costs have bled me dry, that's a major negative.
Re: Post-Surgery Blues: Scoring Question
Happy hour, so dirt cheap. But that's beside the point. Provent would be a perpetual expense -- so you can frame it as $2/night, which sounds great, or you can frame it as $7300 for the next decade, which sounds cha-ching. Which, if it is the only thing that works, then so be it.
But I guess that brings me to the more fundamental and important question: how does one know if it is "working"? Hunting around, I find references to AHI reduction of 50% (known how?), and people "feeling rejuvenated" (which, if my xPAP experience is any indicator, is a poor metric -- how I feel and what the numbers say have been inversely correlated).
But I guess that brings me to the more fundamental and important question: how does one know if it is "working"? Hunting around, I find references to AHI reduction of 50% (known how?), and people "feeling rejuvenated" (which, if my xPAP experience is any indicator, is a poor metric -- how I feel and what the numbers say have been inversely correlated).
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: Post-Surgery Blues: Scoring Question
By doing a sleep study with Provent. Obviously that won't tell you if you're going to feel better on it, but it should tell you if your AHI is normalized.BrianinTN wrote:how does one know if it is "working"?
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
- chunkyfrog
- Posts: 34545
- Joined: Mon Jul 12, 2010 5:10 pm
- Location: Nowhere special--this year in particular.
Re: Post-Surgery Blues: Scoring Question
If such a study were to have positive results, then it would have been in Provent's best interests
to have done it. Then again, the test may have actually been done, but the results were shredded.
to have done it. Then again, the test may have actually been done, but the results were shredded.
_________________
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Airsense 10 Autoset for Her |