Here is some data from my sleep study:
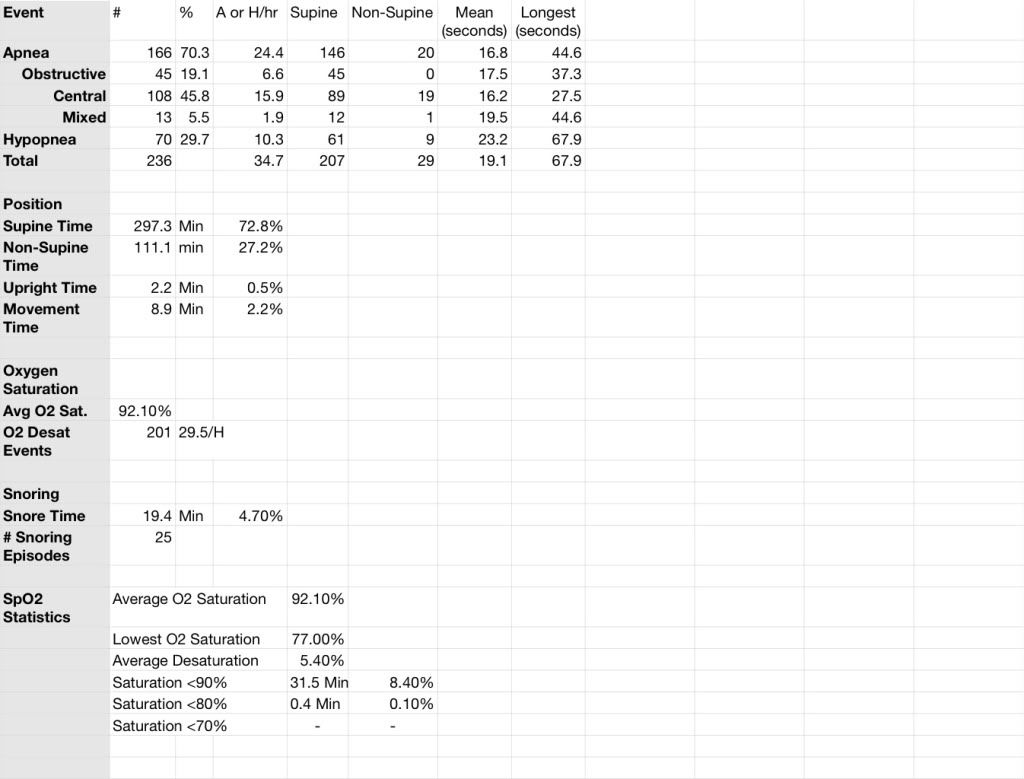
So here's the problem. 45.8% of my apneas were centrals. My hypopneas were not trivial - the longest was over a minute - a long time to leave the heart and brain with too little oxygen. Speaking of oxygen, with 201 desaturation events, and 31.5 minutes below 90%, I'm starving my brain/heart body systems of what they need to function.
My sleep Dr put me on a BiPAP Auto SV (servo ventilator) due to my centrals. He did not titrate me, as the manufacturer recommends. Maybe he has enough clinical experience to set my prescription without titration He has told me he doesn't think I need to know my data, he is "afraid I would obsess on a number," because I don't have the clinical judgement to evaluate it. Since I've been evaluating my diabetes numbers for 10 years, blood pressure for about 5, and taking my own graphs, moving averages, and trends to my PCP Dr. when I have an appointment, I find the sleep Dr's attitude medieval, demeaning, obstructing my path to better therapy, etc. etc. Enough about this aspect of the mess. From my health plan's point of view, he's the only sleep Dr available to me - I'll either win him over or find some other way to get the help I need. I've gotten a lot help from this forum, more than the sleep department has offered to date. Many, many thanks
I've had two weeks on the machine that breathes for me when my brain forgets to take care of it. I've summarized some of the numerical data on a spreadsheet.
Here is 14 days of therapy:
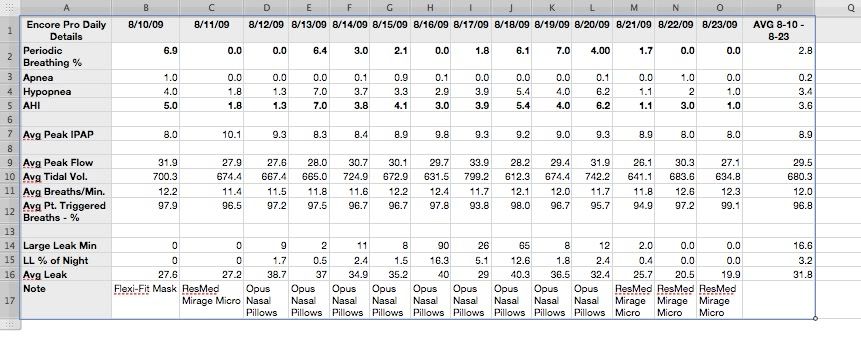
I previously posted detail for one night, 8-19. Now, you can look across two weeks of data, summarized on the spreadsheet, and let me know which dates you would like to see in more detail. Please let me know what looks worth further investigation, and I'll do the copies of the Encore Pro detail pages and the posting. There may be some delays - I only get to work on this in fits and starts, or 5 AM - 6:30 AM. And all this is new to me so I'm pretty slow at doing the computer stuff.
Clearly, I've had mask issues. But I didn't know it until I got Encore Pro and got my first reports. Thank you SWS . I've changed back from the Opus Pillows to a nasal mask, but I'm having such nose pain I may have to go back to the pillows.
My settings are Max IPAP 20; Min IPAP 5, EPAP 5, Backup Rate Auto. I've never approached my Max IPAP - the highest AVG PEAK was 10.1 on night 2. My Apnea number is way down, and I'm hoping Patient Triggered Breaths at about 97% means I'm having few centrals. Periodic Breathing has itself waxed and waned over this two-week time frame. I'm not sure at all what that means.
Kira has suggested setting Min IPAP closer to my Average IPAP. SWS has consistently suggested that I find a more cooperative, patient-oriented sleep Dr. (plus many other helpful suggestions) I'm keeping all recommendations and will follow up with the board, reporting what happens.
Who else can add to the mix?
Thanking you in advance,
Mr Capers













