ASV setting help on Resmed AND PR1 systems: DATA POSTED
- Zzzzzzzzzzz...
- Posts: 331
- Joined: Sun Mar 04, 2012 9:19 am
ASV setting help on Resmed AND PR1 systems: DATA POSTED
Happy Friday!
Below are my current PR System One REMstar BiPAP Auto SV Advanced settings rx'd by my sleep doc to eliminate Hypopneas. AHI's in the 5,6,7 range after a couple weeks at this setting. Centrals are handled, as well as OA's and A's. I'm still struggling with mainly Hypopneas. Leaks aren't bad. Sleep doc is on vacation now. Any suggestions on further tweaks?
MinEPAP 7
MaxEPAP 8
MinPS. 0
Max PS 12
Max Pressure 20
Auto rate
Flex 1
ALSO... I'm considering purchasing a Resmed S9 Adapt SV to keep at my GF's place and see if it just might treat me better than the PR system. I'm aware of the differences between the two. Can anyone advise me on the proper base setting for initial titration on it given the parameters I'm currently at on the PR machine above? I'd ask my sleep doc, however, they're not a Resmed facility.
Thanks in advance (no PR system pun intended)
Z
Below are my current PR System One REMstar BiPAP Auto SV Advanced settings rx'd by my sleep doc to eliminate Hypopneas. AHI's in the 5,6,7 range after a couple weeks at this setting. Centrals are handled, as well as OA's and A's. I'm still struggling with mainly Hypopneas. Leaks aren't bad. Sleep doc is on vacation now. Any suggestions on further tweaks?
MinEPAP 7
MaxEPAP 8
MinPS. 0
Max PS 12
Max Pressure 20
Auto rate
Flex 1
ALSO... I'm considering purchasing a Resmed S9 Adapt SV to keep at my GF's place and see if it just might treat me better than the PR system. I'm aware of the differences between the two. Can anyone advise me on the proper base setting for initial titration on it given the parameters I'm currently at on the PR machine above? I'd ask my sleep doc, however, they're not a Resmed facility.
Thanks in advance (no PR system pun intended)
Z
Last edited by Zzzzzzzzzzz... on Fri Oct 05, 2012 5:27 pm, edited 1 time in total.
- JohnBFisher
- Posts: 3821
- Joined: Wed Oct 14, 2009 6:33 am
Re: ASV setting help on Resmed AND PR1 systems needed please.
I would leave it as is for another couple weeks. Sometimes as we adjust to ASV therapy our breathing actually improves as our bodies become accustomed to the therapy. This is just based on anecdotal evidence on the forum, but it's happened often enough that I suggest you give it some time on these settings.Zzzzzzzzzzz... wrote:... Centrals are handled, as well as OA's and A's. I'm still struggling with mainly Hypopneas. Leaks aren't bad. ... Any suggestions on further tweaks? ...
The S9 ASV unit does not have an auto adjust feature on EPAP. So, I would set it as follows:Zzzzzzzzzzz... wrote:... [My current settings on a PR S1 ASV unit are ...]
MinEPAP 7
MaxEPAP 8
MinPS. 0
Max PS 12
Max Pressure 20
Auto rate
Flex 1
[What should they be on an S9 ASV unit? ...]
...
Mode = ASV
EPAP = 8
MinPS = 3 [3cm H2O is the minimum MinPS]
MaxPS = 12
And that's it. Not a hard system to setup. Certainly not as many dials to jiggle about.
Hope that helps.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: User of xPAP therapy for over 20 yrs. Resmed & Respironics ASV units with EEP=9cm-14cm H2O; PSmin=4cm H2O; PSmax=15cm H2O; Max=25cm H2O |
"I get up. I walk. I fall down. Meanwhile, I keep dancing” from Rabbi Hillel
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
-
StillAnotherGuess
- Posts: 132
- Joined: Sat Apr 23, 2011 4:26 pm
Re: ASV setting help on Resmed AND PR1 systems needed please.
Min PS 3Zzzzzzzzzzz... wrote: Below are my current PR System One REMstar BiPAP Auto SV Advanced settings rx'd by my sleep doc to eliminate Hypopneas. Any suggestions on further tweaks?
MinEPAP 7
MaxEPAP 8
MinPS. 0
Max PS 12
Max Pressure 20
Auto rate
Flex 1
Flex Off
Everything else the same.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: S9 Adapt for Home and Travel, On-Board Firmware, Std. Tubing. EEP 9.8, Min PS 4.6, Max Pressure 21 |
- Zzzzzzzzzzz...
- Posts: 331
- Joined: Sun Mar 04, 2012 9:19 am
Re: ASV setting help on Resmed AND PR1 systems needed please.
Thanks for the advice. I've been on ASV therapy for a few months now. Just been on these SETTINGS for a couple weeks. Might try to optimize further before switching machines... however, something tells me the S9 would treat me more effectively.
The PR1 is free at this point, and it's just hard to imagine shelling out Adapt SV dough out of pocket...
Z
The PR1 is free at this point, and it's just hard to imagine shelling out Adapt SV dough out of pocket...
Z
Re: ASV setting help on Resmed AND PR1 systems needed please.
I'd turn flex off, since it's not terribly helfpul on Bilevel machines if they're set properly.
As you're still having hypopneas (how many?), you're going to want to increase your IPAP slightly. On SV machines, that's done by increasing PS.
The PS min of 0 is an odd setting to begin with for most people and why I wouldn't recommend waiting a few more weeks - it basically means you're currently running your SV as a hybrid CPAP/BiPAP and it's probably slightly uncomfortable. In general, IPAP should be at least 2-3 over your EPAP, so try PS min at 2 for now and see how that works. If you still have significant hypopneas after a few weeks at that setting, you can bump it up a bit more.
As you're still having hypopneas (how many?), you're going to want to increase your IPAP slightly. On SV machines, that's done by increasing PS.
The PS min of 0 is an odd setting to begin with for most people and why I wouldn't recommend waiting a few more weeks - it basically means you're currently running your SV as a hybrid CPAP/BiPAP and it's probably slightly uncomfortable. In general, IPAP should be at least 2-3 over your EPAP, so try PS min at 2 for now and see how that works. If you still have significant hypopneas after a few weeks at that setting, you can bump it up a bit more.
- JohnBFisher
- Posts: 3821
- Joined: Wed Oct 14, 2009 6:33 am
Re: ASV setting help on Resmed AND PR1 systems needed please.
Err.... If his sleep study found that he does not need BiLevel pressure (and his low apnea scores seem to confirm it), then we should not recommend changing the settings. If anything, I would recommend the change after things have settled for a bit.old64mb wrote:... The PS min of 0 is an odd setting to begin with for most people and why I wouldn't recommend waiting a few more weeks - it basically means you're currently running your SV as a hybrid CPAP/BiPAP and it's probably slightly uncomfortable. In general, IPAP should be at least 2-3 over your EPAP, so try PS min at 2 for now and see how that works. If you still have significant hypopneas after a few weeks at that setting, you can bump it up a bit more. ...
Yes, it means that normally his unit acts as a CPAP device, until he has a central apnea .. and then it ramps up the IPAP pressure to sustain respiration. But this sometimes is all that's needed. It's unusual, yes. But completely unheard of, no.
Anyway, that's my two cents on this. But otherwise, I agree with your recommended approach to tackle the hypopneas.
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: User of xPAP therapy for over 20 yrs. Resmed & Respironics ASV units with EEP=9cm-14cm H2O; PSmin=4cm H2O; PSmax=15cm H2O; Max=25cm H2O |
"I get up. I walk. I fall down. Meanwhile, I keep dancing” from Rabbi Hillel
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
Re: ASV setting help on Resmed AND PR1 systems needed please.
I hear you John, but I'd still respectfully disagree.JohnBFisher wrote:Yes, it means that normally his unit acts as a CPAP device, until he has a central apnea .. and then it ramps up the IPAP pressure to sustain respiration. But this sometimes is all that's needed. It's unusual, yes. But completely unheard of, no.
If he was still just having some apneas and a few leftover hypopneas, I'd say running the machine a while longer as a hybrid just to see if things resolve would make sense. But with something like a 4-6 HI (presuming apneas are <1), the machine is ramping pressure a bunch to chase those hypopneas anyway since it can (and probably does given a 5-7 AHI) crank IPAP up to 20 under current settings. If they're obstructive flow limitations, a couple cm on base IPAP may very well resolve this.
At worst, it's not going to do any harm since it's almost certainly running at that pressure most of the time anyway.
Zzz, could you post a graph of a typical night by any chance?
- Zzzzzzzzzzz...
- Posts: 331
- Joined: Sun Mar 04, 2012 9:19 am
Re: ASV setting help on Resmed AND PR1 systems needed please.
Unfortunately, everything everyone is saying makes sense to me. Ha. I guess that's the problem with options, opinions, solutions and variables. Will post up a graph from encore basic when I get home later. For some reason sleepyhead on my mac doesn't like the PR1 data card delivery. But I sure wish it did... not a big fan of Encore Basic.
Thanks!
Z
Thanks!
Z
- Zzzzzzzzzzz...
- Posts: 331
- Joined: Sun Mar 04, 2012 9:19 am
Re: ASV setting help on Resmed AND PR1 systems needed please.
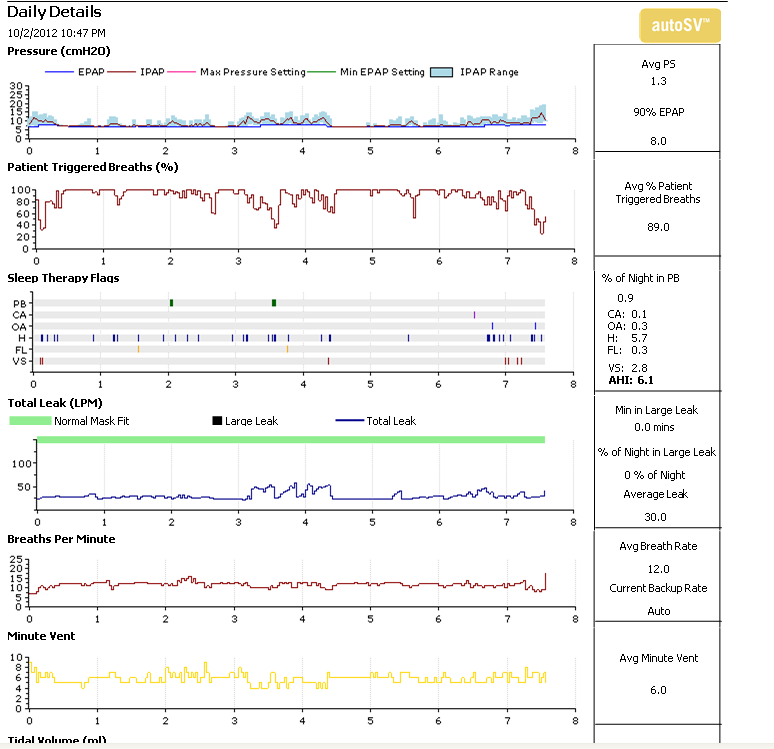
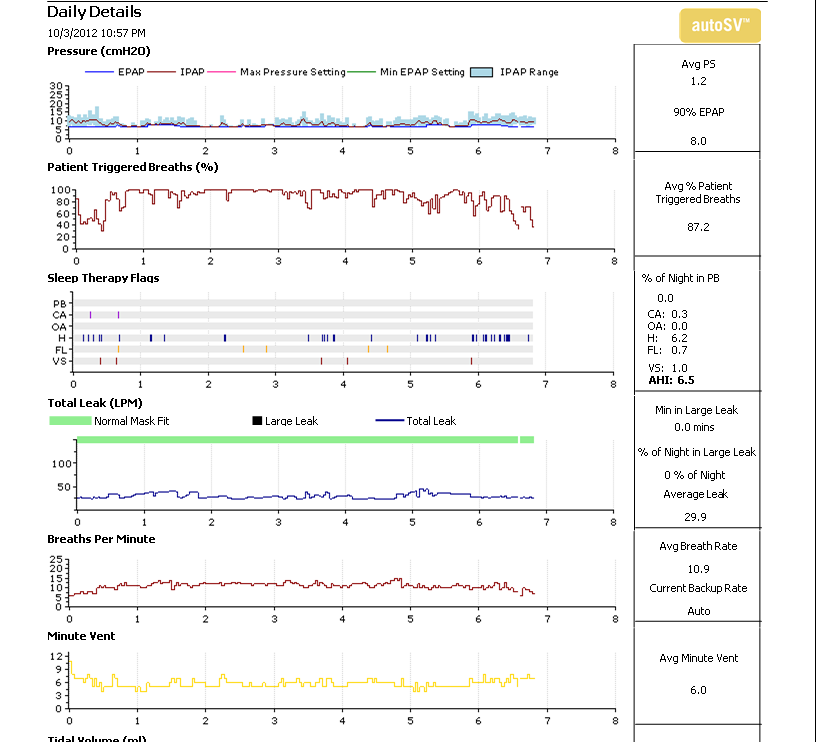
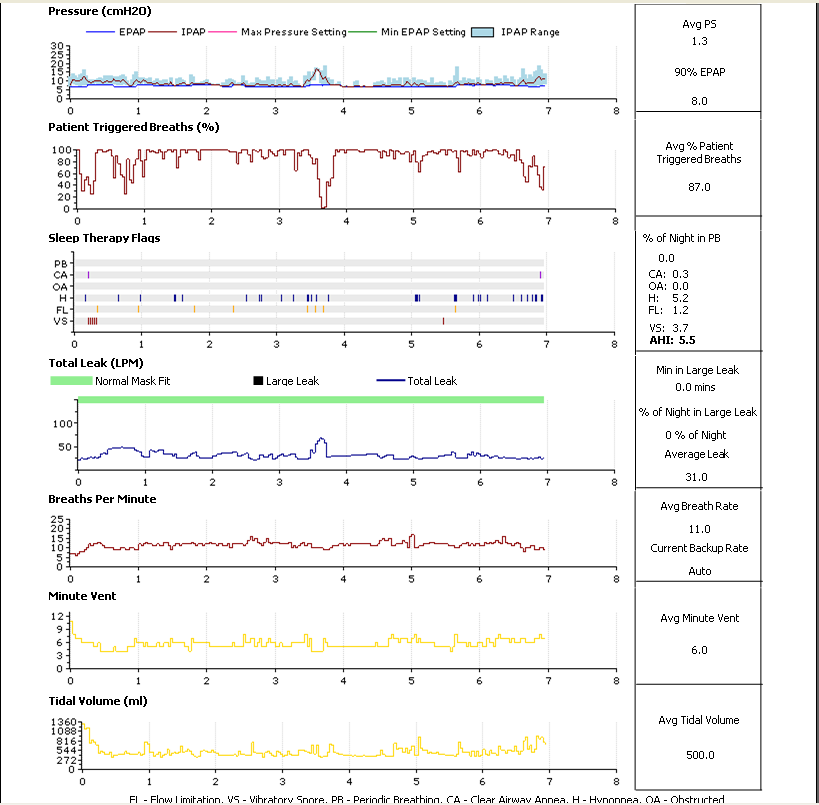
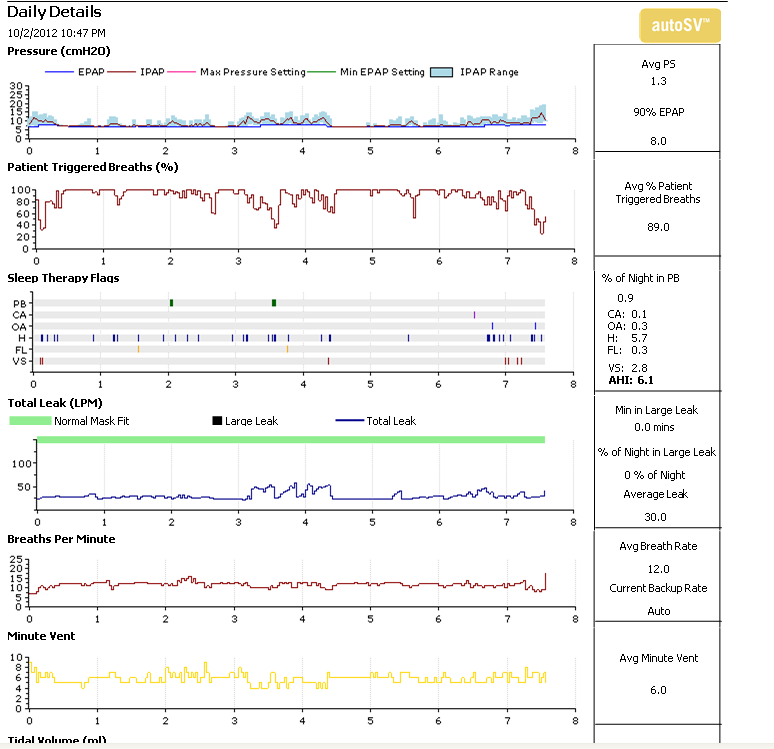
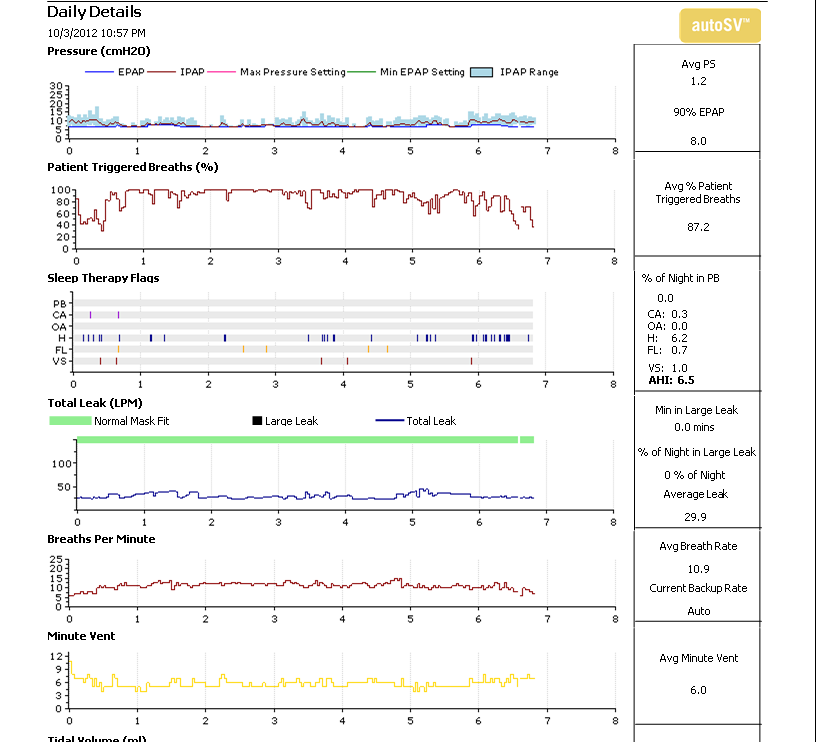
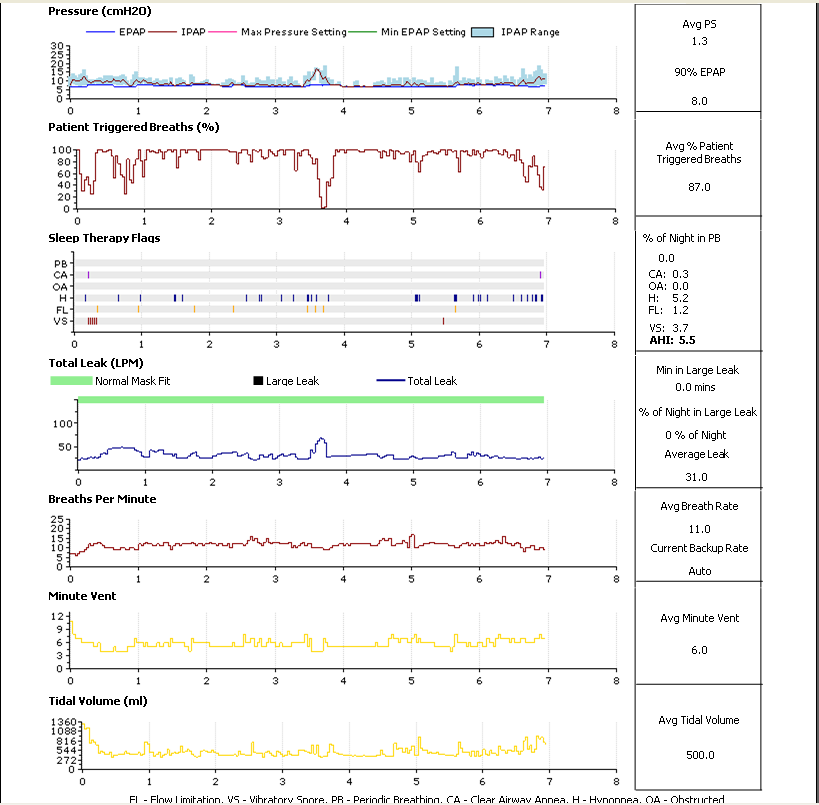
These are my last three nights in descending order:
Thanks for any analysis and advice on settings to decrease Hypopneas.
Z
Thanks for any analysis and advice on settings to decrease Hypopneas.
Z
Re: ASV setting help on Resmed AND PR1 systems: DATA POSTED
Zzzzzzzzzzz... wrote:Any suggestions on further tweaks?
Hi Z,JohnBFisher wrote:Yes, it means that normally his unit acts as a CPAP device, until he has a central apnea .. and then it ramps up the IPAP pressure to sustain respiration. But this sometimes is all that's needed. It's unusual, yes. But completely unheard of, no.
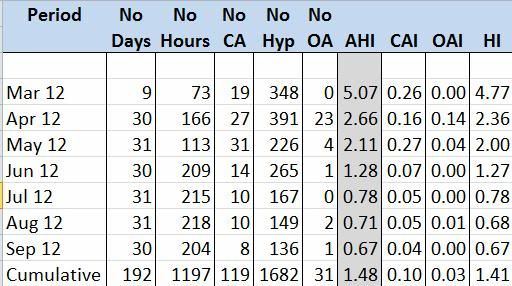
I'm gonna' have to go along with JohnBFisher on this one. I have been on the same autoSV as you since March. Below I posted the 192 days between March 2012 and September 30, 2012. As you can see, I had the same issue as you. From the beginning, it almost totally eliminated both CAs and OAs, but I had an excessive number of hypopneas. I have never had a problem exhaling against pressure, so over time I increased my settings to:
EPAP Min: 12.5
EPAP Max: 16.0
PS Min: 0
PS Max: 12.5
BPM: Auto
Flex: None
I always had my Min PS at 0 and it was very comfortable for me to have the machine function as a CPAP machine until it needed to adddress a CA. I have had a steady reduction in hypopneas and, as you can see, the September results of:
AHI: 0.67
CAI: 0.04
OAI: 0.00
HI: 0.67
Were about as good as I could expect for the 30 period.
(BTW: I use SleepyHead V09.2.1 and it works perfectly with my S1 BiPAP autoSV Advanced)
Hope that helps!
Good luck with your therapy.
_________________
| Machine: ResMed AirCurve 10 ASV Machine with Heated Humidifier |
| Mask: AirFit™ F40 System - M/STD |
Re: ASV setting help on Resmed AND PR1 systems: DATA POSTED
Thanks for posting that Z. Couple things jump out.
First, pressure. I'm going to stick with my recommendation to try PS Min at 2 and to turn off Flex.
It's possible you might be like Grand Pap and do better on a fixed pressure for as long as you can tolerate it. There are certainly people with central-predominant apnea who do better with fixed pressure than on Bilevel. In fact, Grand Pap started a nice thread a few months ago where -SWS points out a decent study on this here - viewtopic/t82822/viewtopic.php?f=1&t=77572.
The study works out to about a quarter of patients had more centrals on Bilevel (and 10% less) - although it's important to note the average delta between IPAP and EPAP for them was 5.9 +/- 3.1, so quite a bit more severe than the 2 or 3 I was recommending. (And to quote the study, "Larger (bilevel) pressure differences lead to larger tidal volumes, which lower Pco2, thus worsening central apneas." Makes good theoretical sense, although I freely admit I'm not as strong on the pulmonary side as some people around here.)
What's interesting and not nearly as well known is that the same thing applies to some UARS patients, where CPAP is a more effective treatment than Bilevel. I've not seen a study on this, but I've heard ancedotal evidence from a couple sleep doctors about it. Bilevel isn't a catch-all by any means.
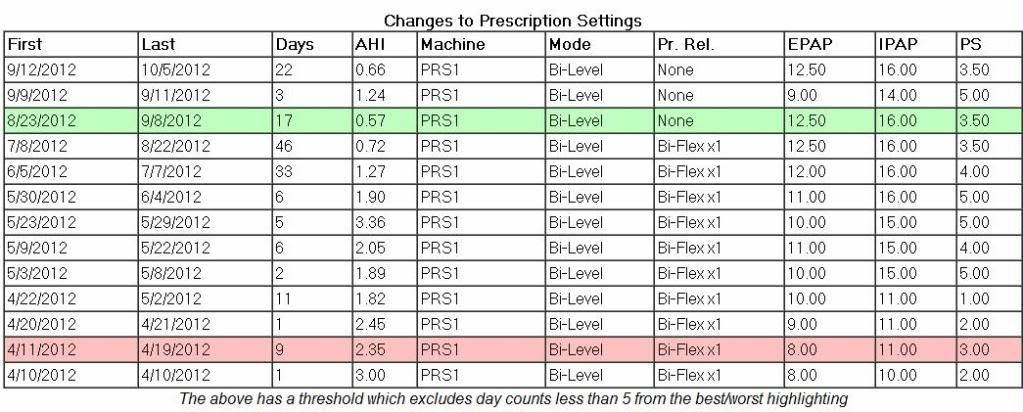
That said, what's also important to note about Grand Paps' experience is that (as he states here) ultimately he did increase pressure from his original Rx settings and that eliminated the hypopneas. From what I can tell (and please feel to jump back in if I'm wrong Grand Pap), he dropped IPAP down to EPAP levels to run the machine as a CPAP, but the more relevant point is that he also did raise his EPAP from 8 to 10, and that 2 cm delta was enough to really wipe out most of his events over time.
Basically, that's the same thing I'm suggesting - you need to try slightly higher base pressure on one setting or another to take out your hypopneas. It may end up being that it'll be better to keep running in CPAP mode, but there's no real harm in trying to raise IPAP a couple cm first to see if you're in the 75%. If after a few weeks ramping slowly up to something like 3-4 cm at most doesn't work - one of the things that you've got to keep in mind with any titration, CPAP or meds, is that unless you've got to deal with something acute a little goes a long way - then you can try pushing that extra pressure though EPAP instead.
Second, the other thing that jumps out at me is the combination of the patient triggered breathing line dropping off a cliff when leaks get bad along with enough snoring to be noteworthy. Any chance you're a mouth breather, or was that just from getting up in the middle of the night?
First, pressure. I'm going to stick with my recommendation to try PS Min at 2 and to turn off Flex.
It's possible you might be like Grand Pap and do better on a fixed pressure for as long as you can tolerate it. There are certainly people with central-predominant apnea who do better with fixed pressure than on Bilevel. In fact, Grand Pap started a nice thread a few months ago where -SWS points out a decent study on this here - viewtopic/t82822/viewtopic.php?f=1&t=77572.
The study works out to about a quarter of patients had more centrals on Bilevel (and 10% less) - although it's important to note the average delta between IPAP and EPAP for them was 5.9 +/- 3.1, so quite a bit more severe than the 2 or 3 I was recommending. (And to quote the study, "Larger (bilevel) pressure differences lead to larger tidal volumes, which lower Pco2, thus worsening central apneas." Makes good theoretical sense, although I freely admit I'm not as strong on the pulmonary side as some people around here.)
What's interesting and not nearly as well known is that the same thing applies to some UARS patients, where CPAP is a more effective treatment than Bilevel. I've not seen a study on this, but I've heard ancedotal evidence from a couple sleep doctors about it. Bilevel isn't a catch-all by any means.
That said, what's also important to note about Grand Paps' experience is that (as he states here) ultimately he did increase pressure from his original Rx settings and that eliminated the hypopneas. From what I can tell (and please feel to jump back in if I'm wrong Grand Pap), he dropped IPAP down to EPAP levels to run the machine as a CPAP, but the more relevant point is that he also did raise his EPAP from 8 to 10, and that 2 cm delta was enough to really wipe out most of his events over time.
Basically, that's the same thing I'm suggesting - you need to try slightly higher base pressure on one setting or another to take out your hypopneas. It may end up being that it'll be better to keep running in CPAP mode, but there's no real harm in trying to raise IPAP a couple cm first to see if you're in the 75%. If after a few weeks ramping slowly up to something like 3-4 cm at most doesn't work - one of the things that you've got to keep in mind with any titration, CPAP or meds, is that unless you've got to deal with something acute a little goes a long way - then you can try pushing that extra pressure though EPAP instead.
Second, the other thing that jumps out at me is the combination of the patient triggered breathing line dropping off a cliff when leaks get bad along with enough snoring to be noteworthy. Any chance you're a mouth breather, or was that just from getting up in the middle of the night?
Re: ASV setting help on Resmed AND PR1 systems: DATA POSTED
Hi old64md,old64mb wrote:That said, what's also important to note about Grand Paps' experience is that (as he states here) ultimately he did increase pressure from his original Rx settings and that eliminated the hypopneas. From what I can tell (and please feel to jump back in if I'm wrong Grand Pap), he dropped IPAP down to EPAP levels to run the machine as a CPAP, but the more relevant point is that he also did raise his EPAP from 8 to 10, and that 2 cm delta was enough to really wipe out most of his events over time.
Yes, you are correct. To not confuse the post for the OP, I kept this post fairly basic, but since you referred to my prior post, I decided I would cut and post the SleepyHead Graph of the "Prescription Settings." When I was on CPAP, my Rx was for 10cm H2o. So I attempted to adjust the pressures to attain that result. Then, as you can see from the graph, I experimented with gradually raising (and lowering) the EPAP to tweak the IPAP and attempt to get the best resolution of the hypopneas.
Probably more info than needs, but might be helpful.
_________________
| Machine: ResMed AirCurve 10 ASV Machine with Heated Humidifier |
| Mask: AirFit™ F40 System - M/STD |
Last edited by Grand-PAP on Sat Oct 06, 2012 1:37 pm, edited 1 time in total.
- Zzzzzzzzzzz...
- Posts: 331
- Joined: Sun Mar 04, 2012 9:19 am
Re: ASV setting help on Resmed AND PR1 systems: DATA POSTED
Hey all,
Boy did I have a crap night last night. I DID try the new settings... however, due to a migraine just before bed, a sore throat and a stuffed up nose, well... you can imagine the results this morning.
ZEO looked a bit better, however. Managed to still get some deep sleep and not TOO much wake.
At any rate, I'll stay the course til I feel better and see what happens. Incidentally, I don't have too much trouble with mouth breathing/snoring (at least with the gear on). My leaks are typically okay, and
correct me if I'm wrong but the total leak doesn't subtract the built in leak rate from the total, correct?
Thanks again for the help,
Z
Boy did I have a crap night last night. I DID try the new settings... however, due to a migraine just before bed, a sore throat and a stuffed up nose, well... you can imagine the results this morning.
ZEO looked a bit better, however. Managed to still get some deep sleep and not TOO much wake.
At any rate, I'll stay the course til I feel better and see what happens. Incidentally, I don't have too much trouble with mouth breathing/snoring (at least with the gear on). My leaks are typically okay, and
correct me if I'm wrong but the total leak doesn't subtract the built in leak rate from the total, correct?
Thanks again for the help,
Z










