OK, BB, you know the expression, "Another Day, Another Disaster". But Life gives you a Bucketful of Challenges every day, not a Bucketful of Winning Lottery Tickets (which is NBD unless you let the buckets pile up).BleepingBeauty wrote:But it's my b-day, and I'm not in the mood to start bleeping, so can we talk about this more at another time?
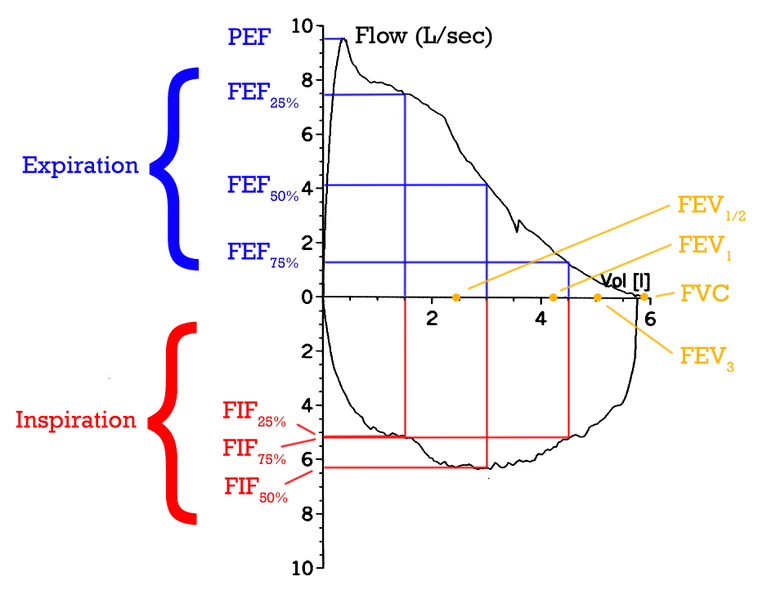
In the Forced Vital Capacity maneuver, which is what you did up there Pre- and Post-Bronchodilator, the absolute maximum effort blowing out (as in "your eyes pop out of your head and roll onto the floor") must be maintained for at least 6 seconds to insure the lung is completely empty and get accurate measurements. As noted in the results, your expiratory times are 1.6 and 1.4 seconds, respectively, so all measurements involving expiratory times > FEV 1.0 (Forced Expiratory Time in 1 second) and FVC are inaccurate (the FVC is undoubtedly a little low).
Indeed, values like the FEF 75 and FEF 75-85% are "frivolous".
The good news is, since your FVC is probably a little higher, I don't think you are "restricted".
The bad news is, one of the measurements that measures "obstruction" (reactive airways), the PEF (Peak Expiratory Flow)(which may be accurate, depending on effort) is quite low. This is suggestive of smoking damage (or perhaps allergy).
Anyway, PFT is completely effort-dependent, and if you weren't coached to do this test correctly, then that value isn't accurate, either.
When the test is done correctly, perhaps the most important parameter to measure the damage caused by smoking will be the FEF 25-75%.
When you said you were seeing a pulmonologist for the OSA, I thought you'd be getting the PFT out of there, it never occurred to me that the PCP would be doing the test. Shoot.
Y'know what, get them in here to explain themselves. I mean, does anybody out there know what they're doing?
The small spirometers can be accurate for Simple Spirometry if the maneuver is done properly and the machine is operating correctly. However, this includes calibrating the machine daily, and as you can see, that thing hasn't been calibrated for a nearly a month (May 7).robertmarilyn wrote:I want you to know that the official real PFT test at a lab is sort of fun. The one I did had me shut inside of a big box and there were a lot of instructions I had to follow...
However, to your point, mar, the Complete PFT, including Lung Volumes and Diffusion, would have offered BB important information (diffusion) and Muffy fodder for CompSAS discussion (FRC and, consequently, CO2 Reserve).
Show him this post. That might alter what he's thinking a bit.BleepingBeauty wrote:My PCP probably thinks I've become a hypochondriac
Muffy