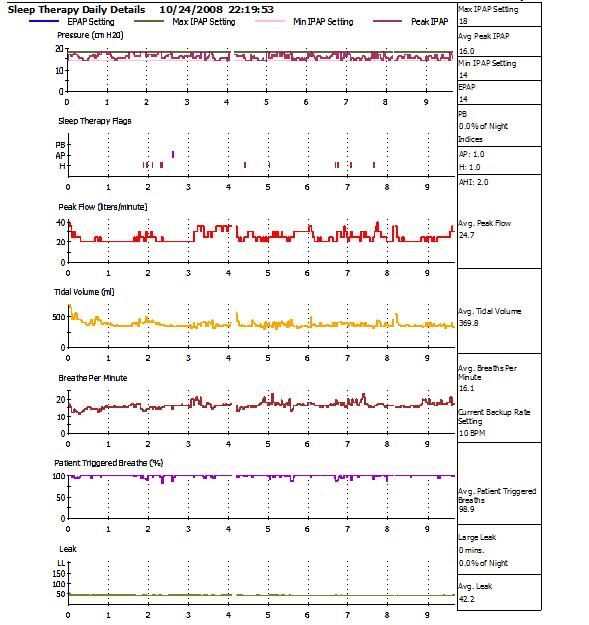
Those values are available on the fly right on the LCD in monitor mode, but it is better to use an avg from the report if you have it except IT is not displayed on the report, so LCD is only place you will find it outside of the lab.-SWS wrote: Turning BPM from auto to manual means that you need to know not only the correct spontaneous breath rate, but just as importantly the correct pulse width or time that should be spent in inspiration. We can see on Bev's Encore charts a larger than acceptable spread between manual backup BPM of 10 and Bev's spontaneous machine-affected breath rate of 16.1 (now higher than before). We have absolutely no way of knowing how counterproductive the manual inspiratory time setting of 1.2 happens to be.... it's a blind guess also for lack of PSG instrumentation. And to continue making adjustments to manual BPM and manual IT short of a PSG simply flounders around in blind pilot mode IMO.
Let's get this straight, I suggested on page 2 of this thread that she stay on Aflex and probably wouldn't see any improvement going to the SV. Think it may even be right next to your post with the URL to cpapauction.-SWS wrote: Snoredog's rationale, so far, for turning auto BPM off has been to get at that alluring but mysterious inspiratory setting of 1.2 seconds. He's not sure specifically why it shows up in literature so much, but the fact that it does apparently lends a measure of promise. The PSG titration charts recommend IT of 1.2 as a starting point for routine manual titration by clinicians who have PSG equipment to closely follow all the effects of manual titration changes. Snoredog's been wanting to try that alluring and mystical 1.2 second IT setting ever since he first laid eyes on it.
And it is NOT my rationale at all, it is mfg protocol for the machine of which Bev has a hardcopy of, follow the decision tree it tells you to use those settings. Those are "Minimum" settings so even the mfg thinks they are okay or they wouldn't have established a recommended minimum.
You only got 16.1 avg BPM from last night's report, it is shown lower on prior Encore reports, but I realize it is much easier to criticize someone's suggestions after the fact, I guess if you want to play that game we could say the same thing about buying the SV only that she'd still have $1500+ left in her wallet.
Shotgun approaches? if you haven't already edited it out (yeah we know about that bookmark game) as I recall for initial settings I wanted EPAP at 9 cm (her first night Encore on the SV) and you wanted it at 14 cm. My reasoning was I think they missed her titration and hand gone over the hill, but desats from her PSG said don't stay there too long.-SWS wrote:
I think these experiments might have been better controlled if they were baselined and incremental. The more I think about it, the more I think shotgun changes are not the way to go. PSG certainly is the way to go. I would personally at least like to see those CPAP and BiLevel baseline measurements that should have been the experimental front-end before introducing small controlled deltas.
So the next night we used your settings of 14 cm, and the next night were the same. Periodic Breathing showed up where there was none the first night. You think 2nd and 3rd night were better? I'd argue that, she hasn't had a 2 hr stretch yet on that machine I'd call good.
Hey all shotgun approaches remaining are yours, I thought my settings were pretty conservative from the beginnning after all you argued why we wanted to use the 9 cm EPAP settings (where she actually did the best IMO). I suggest she go back on Aflex, AHI is AHI and using that machine she has the lowest seen, if that AHI includes central events she's doing even better.
He's a box of bird shot, have at it.