420E Run Question ???
tangents-Cathy:
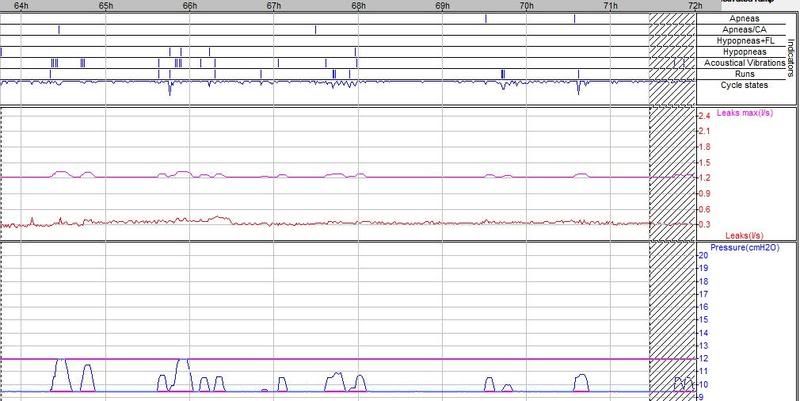
I like your graphs and how you identified the events in the center chart with vertical arrows which drove up your pressure, very nice.
Your example is also why I feel Bill has problems with all those flow runs, all one has to do is look at your top graph while on CPAP and the bottom graph on Auto, lower pressure suits you well, doesn't appear at all to have anything to do with changing pressure, your bottom chart looks to offer much more restful sleep than the top chart and that is what Bill's should look like if the machine was responding to his needs properly.
He also has had problems with aerophagia, he should be using the lowest possible pressure to assist that even to a point of allowing a higher AHI in favor of lower pressure use.
I like your graphs and how you identified the events in the center chart with vertical arrows which drove up your pressure, very nice.
Your example is also why I feel Bill has problems with all those flow runs, all one has to do is look at your top graph while on CPAP and the bottom graph on Auto, lower pressure suits you well, doesn't appear at all to have anything to do with changing pressure, your bottom chart looks to offer much more restful sleep than the top chart and that is what Bill's should look like if the machine was responding to his needs properly.
He also has had problems with aerophagia, he should be using the lowest possible pressure to assist that even to a point of allowing a higher AHI in favor of lower pressure use.
someday science will catch up to what I'm saying...
Thanks for the kind words, Snoredog!
My feeling is that the lower pressure setting is especially important to my therapy. At constant 10, I had runs all over the place. At 8-12, I had intermittent runs that had to be "chased" by the APAP. But with the lower pressure at 9.5, I think the majority of my flow limitations were prevented. Does that make any sense? That's why I was suggesting to Nighthawkeye to raise his pressure range.
Cheers,
Cathy
My feeling is that the lower pressure setting is especially important to my therapy. At constant 10, I had runs all over the place. At 8-12, I had intermittent runs that had to be "chased" by the APAP. But with the lower pressure at 9.5, I think the majority of my flow limitations were prevented. Does that make any sense? That's why I was suggesting to Nighthawkeye to raise his pressure range.
Cheers,
Cathy
[quote="tangents"]Thanks for the kind words, Snoredog!
My feeling is that the lower pressure setting is especially important to my therapy. At constant 10, I had runs all over the place. At 8-12, I had intermittent runs that had to be "chased" by the APAP. But with the lower pressure at 9.5, I think the majority of my flow limitations were prevented. Does that make any sense? That's why I was suggesting to Nighthawkeye to raise his pressure range.
Cheers,
Cathy
My feeling is that the lower pressure setting is especially important to my therapy. At constant 10, I had runs all over the place. At 8-12, I had intermittent runs that had to be "chased" by the APAP. But with the lower pressure at 9.5, I think the majority of my flow limitations were prevented. Does that make any sense? That's why I was suggesting to Nighthawkeye to raise his pressure range.
Cheers,
Cathy
someday science will catch up to what I'm saying...
- NightHawkeye
- Posts: 2431
- Joined: Thu Dec 29, 2005 11:55 am
- Location: Iowa - The Hawkeye State
LOL. Well, bad as it may look now, Snoredog, it's noticeably better now than it was with a wider APAP range. Most nights now I never have to get up in the middle of the night. The wider APAP range earlier was necessary to combat aerophagia for a while though, and therapy under those conditions was a lot better than no therapy at all. I was well aware that it was sub-optimal though.Snoredog wrote: ... and that is exactly what is happening to Bill's therapy in my opinion, he made changes to get his AHI down and created a condition that contradicts restful sleep.
As I said before AHI is not everything.
Tangent's charts serve as an inspiration. I'm left wondering what makes the difference in my case that the machine indicates such a large number of "runs". Possibilities seem to be:
- Data reporting anomaly - seems less likely as this thread has progressed
- Nasal congestion - SWS's comment suggests that congestion may not be the answer
- Cardiac issues - seems unlikely to be the cause of "runs" in data for so many folks
- Respiratory drive - it's a major component of OSA anyway. CAP seems to be an extension with instabilities. Exercise helps, but ...
The last three definitely apply to me, and I have some limited control over all three. Nasal congestion appears to be the one which I may be able to do the most about. All three are also interrelated so that an improvement in one might very well improve the others. Sure would like to have more definite info supporting any of the possibilities though.
Regards,
Bill
Bill, just a crazy thought, but could your 420E be chasing snores that ain't really snores? I'm talking about phantom snores that your machine thinks are snores but are caused by your hose rubbing against something and vibrating.
Just a thought, but ya might try looking at your hose routing.
Kajun
Just a thought, but ya might try looking at your hose routing.
Kajun
_________________
| Mask: Ultra Mirage™ Full Face CPAP Mask with Headgear |
| Additional Comments: APAP, 8-14 cm H2O. |
This therapy WORKS!!!
NightHawkeye wrote:LOL. Well, bad as it may look now, Snoredog, it's noticeably better now than it was with a wider APAP range. Most nights now I never have to get up in the middle of the night. The wider APAP range earlier was necessary to combat aerophagia for a while though, and therapy under those conditions was a lot better than no therapy at all. I was well aware that it was sub-optimal though.Snoredog wrote: ... and that is exactly what is happening to Bill's therapy in my opinion, he made changes to get his AHI down and created a condition that contradicts restful sleep.
As I said before AHI is not everything.
Tangent's charts serve as an inspiration. I'm left wondering what makes the difference in my case that the machine indicates such a large number of "runs". Possibilities seem to be:
- Data reporting anomaly - seems less likely as this thread has progressed
- Nasal congestion - SWS's comment suggests that congestion may not be the answer
- Cardiac issues - seems unlikely to be the cause of "runs" in data for so many folks
- Respiratory drive - it's a major component of OSA anyway. CAP seems to be an extension with instabilities. Exercise helps, but ...
The last three definitely apply to me, and I have some limited control over all three. Nasal congestion appears to be the one which I may be able to do the most about. All three are also interrelated so that an improvement in one might very well improve the others. Sure would like to have more definite info supporting any of the possibilities though.
Regards,
Bill
someday science will catch up to what I'm saying...
Friends,
I've just lost almost 2 hours of work trying to compile something on this subject - due to a power failure.
pjwalman was worried about central apneas, had NR (non-resopnsive, therefore suspected central) apneas on a Respironics, and was loaned a PB by Rested Gal so she could see if that machine showed her having central apneas.
The first 2 nights settings ("setting no. 2"):
Peggy's first 2 nights on the PB420E had the following setting
Mode : Pilot : A+AV+IFL2
Min. pressure : 10.0 cmH2O
Initial pressure : 10.0 cmH2O
Max. pressure : 20.0 cmH2O
Max. press. for command on Apnea : 10.0 cmH2O
Ramp duration : 0 min

The results for the sessions when the machine was in use:
Events :
Index/h Apneas : 0.8
Index/h Apneas/CA : 0.6
Index/h Hypopneas : 3.1
Flow limited apneas Hypopneas: 0.5
Number Runs (FL): 230
Index/h Runs (FL): 53.1
And 53% flow limited breaths.
Each of 2 nights sessions had concentrated obstructive events, to which the machine responded sluggishly. There was no chance was those sustained obstructions could be healthy.


My reasoning was that Peggy has far more hyponeas than apneas (PSG and present data), IFL1 off really cuts response to hypopneas, so I suggested she turn IFL1 on and cap the pressure - with the amount of flow lmitation runs she had, I was afraid it would go stratospheric otherwise. I chose 14 because that's what seemed to stabilize her breathing on both nights. She was not having pressure induced apneas, and she was having (to my mind) unnecessary apneas.
Compare the slow respond to the hypopnea buch in session 186 (alas, no snores to push the pressur along) to the fast rise on the first, where snores came along to help.
And note also, on session 187 how the machine does not respond to the apnea - because the maximum pressure for response on apnea was 10.
This it the next configuration:
Min. pressure : 10.0 cmH2O
Initial pressure : 11.0 cmH2O
Max. pressure : 14.0 cmH2O
Max. press. for command on Apnea : 12.0 cmH2O
The worst night for that period had an AHI of 4.9 - and the pressure hung at 14 most of the first night, it did drop, all the way to 10, and go back up agian, on the second night, which had 0 obstructive events, 0 hypopneas with flow limitation, a few snores and a few apneas/ca. Much better, and aerophagia was better too.
Clearly, those NR events on the Respironics were non responsive obstructive events. We thought she may be dreaming at home, needing higher pressure, (1.5 mins of dreaming during the PSG) and maybe swallowing air during the struggle to breath.
The doc. was right about her central apneas being arousal responses.
I think that for some us, the PB mis-identifies flow limited cycles. As a result of that, it has far too many flow limitation runs and response to them pushes the pressure up too much.
On the other hand, when a person does have more hypopneic events, turning IFL1=off may mean they end up with a non responsive (or sluggish, to say the least) machine.
O.
I've just lost almost 2 hours of work trying to compile something on this subject - due to a power failure.
pjwalman was worried about central apneas, had NR (non-resopnsive, therefore suspected central) apneas on a Respironics, and was loaned a PB by Rested Gal so she could see if that machine showed her having central apneas.
The first 2 nights settings ("setting no. 2"):
Peggy's first 2 nights on the PB420E had the following setting
Mode : Pilot : A+AV+IFL2
Min. pressure : 10.0 cmH2O
Initial pressure : 10.0 cmH2O
Max. pressure : 20.0 cmH2O
Max. press. for command on Apnea : 10.0 cmH2O
Ramp duration : 0 min

The results for the sessions when the machine was in use:
Events :
Index/h Apneas : 0.8
Index/h Apneas/CA : 0.6
Index/h Hypopneas : 3.1
Flow limited apneas Hypopneas: 0.5
Number Runs (FL): 230
Index/h Runs (FL): 53.1
And 53% flow limited breaths.
Each of 2 nights sessions had concentrated obstructive events, to which the machine responded sluggishly. There was no chance was those sustained obstructions could be healthy.


My reasoning was that Peggy has far more hyponeas than apneas (PSG and present data), IFL1 off really cuts response to hypopneas, so I suggested she turn IFL1 on and cap the pressure - with the amount of flow lmitation runs she had, I was afraid it would go stratospheric otherwise. I chose 14 because that's what seemed to stabilize her breathing on both nights. She was not having pressure induced apneas, and she was having (to my mind) unnecessary apneas.
Compare the slow respond to the hypopnea buch in session 186 (alas, no snores to push the pressur along) to the fast rise on the first, where snores came along to help.
And note also, on session 187 how the machine does not respond to the apnea - because the maximum pressure for response on apnea was 10.
This it the next configuration:
Min. pressure : 10.0 cmH2O
Initial pressure : 11.0 cmH2O
Max. pressure : 14.0 cmH2O
Max. press. for command on Apnea : 12.0 cmH2O
The worst night for that period had an AHI of 4.9 - and the pressure hung at 14 most of the first night, it did drop, all the way to 10, and go back up agian, on the second night, which had 0 obstructive events, 0 hypopneas with flow limitation, a few snores and a few apneas/ca. Much better, and aerophagia was better too.
Clearly, those NR events on the Respironics were non responsive obstructive events. We thought she may be dreaming at home, needing higher pressure, (1.5 mins of dreaming during the PSG) and maybe swallowing air during the struggle to breath.
The doc. was right about her central apneas being arousal responses.
I think that for some us, the PB mis-identifies flow limited cycles. As a result of that, it has far too many flow limitation runs and response to them pushes the pressure up too much.
On the other hand, when a person does have more hypopneic events, turning IFL1=off may mean they end up with a non responsive (or sluggish, to say the least) machine.
O.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
I'm confused about that statement, ozij. I am guessing that you meant to say IFL2.ozij wrote:IFL1 off really cuts response to hypopneas
So here's the way I interpret the above:Regarding the 420e, Silver Lining 3 Online Documentation wrote: Events for which the device automatically increases the pressure:
- Apneas (A)
- Acoustical Vibrations (AV)
- Flow Limitation (FL)
Flow Limitation Run (IFL1) and Flow Limitation combined with an amplitude decrease (IFL2) are the sole events for which you can choose to authorise an increase in pressure.
1) Standalone Hypopneas that are unaccompanied by flow limitation should never cause the 420e to increase pressure (regardless of any IFL settings),
2) Turning off IFL1 should halt pressure increases to Flow Limitation Runs (but have nothing to do with hypopneas),
3) Turning off IFL2 will halt pressure increases to any and all hypopneas (I may need to reconsider/revise this---any help appreciated),
4) Turning on IFL2 does not at all guarantee that all "H + FL" meets the 420e pressure-increase criteria within the 420e algorithm
To exemplify that last interpretive point, imagine that we place a similar soft-switch or trigger for hypopneas in the Respironics algorithm, while leaving the algorithm otherwise intact. Let's call that trigger or soft-switch "RH2". As patients or clinicians we might turn "RH2" off to ensure the Remstar does not respond to any hypopneas whatsoever. But if we turn "RH2" on, hypopnea response reverts to factory defaults: not all hypopneas cause a pressure increase. In this hypothetical Remstar case, when factory-defaulted hypopnea response is enabled (w/ "RH2" on), initial hypopneas still receive no pressure; nor do any hypopneas receive pressure once NRAH criteria has been met.
I see IFL2 as a switch to alternately disable hypopnea response altogether, or to allow a "selective" hypopnea response to occur according to the 420e algorithm's own internal criteria.
All APAP manufacturers seem to take a conservative approach to hypopnea pressure increase.
Bill, you mentioned above that your FL runs seem worse at higher pressure. Since your LES closure is extremely poor, I wonder if pressurized air-loss through the LES sufficiently distorts your inspiratory wave shape. Specifically I am thinking that just enough breech through the LES can flatten or otherwise distort your inspiratory waveform, returning a false-positive from the 420e's ultra-sensitive FL detection routine. If so this false-detection scenario should be more prolific at higher pressures I would think.NightHawkeye wrote:It was when I raised the minimum pressure that the "runs" began to occur on a more-or-less continuous basis
[quote="A Noun Definition of "Run" That Publisher Houghton Mifflin Company"] "4. A number of things placed or occurring one after the other: chain, consecution, course, order, procession, progression, round, sequence, series, string, succession, suite, train. Informal streak. See order/disorder.[/quote]
The difference between a flow limitation and a flow limitation run in my mind is simplified by the above context-based definition of a run: a run is a "succession". A "flow limitation run" is nothing more than any one of several quantitatively-specified "successions of flow limitations". At least that's the way I like to think of it.
Bear in mind that a respiratory "cycle" is but a breath. It is a breath that is comprised of: 1) an inspiratory phase, 2) an expiratory phase, and 3) any pauses that occur between those two phases. So a "flow limited cycle" is really nothing more than a "flow limited breath". And specifically PB defines a single "flow limitation" or "flow limited cycle" as occurring during that inspiratory part of the complete respiratory cycle or breath.
I definitely agree with that. However, I think this 420e "FL magnifying glass" (regarding such close FL wave-shape scrutiny) is a double-edged sword that Rapoport probably put in place intentionally. I'll try to speculate more about that soon, as long as no one boos my wild and crazy conjecture off the stage....ozij wrote:I think that for some us, the PB mis-identifies flow limited cycles. As a result of that, it has far too many flow limitation runs and response to them pushes the pressure up too much.
By the way, it's great to be able to collaboratively put our heads together on all this. It's really extremely complex stuff IMHO.
- NightHawkeye
- Posts: 2431
- Joined: Thu Dec 29, 2005 11:55 am
- Location: Iowa - The Hawkeye State
-SWS, your hypothesis fits the observed data far better than anything else conjectured in this thread. Perhaps the amount of air getting past the LES wouldn't have to be very large if it were cyclic. I have sensed for a while that a certain amount of air being forced into my gut was then also coming back up and causing a certain amount of mouth leakage. Peggy's data is definitely cyclic and she too suffers aerophagia. It wouldn't take too much more to convince me of the validity of your hypothesis, -SWS.-SWS wrote:Bill, you mentioned above that your FL runs seem worse at higher pressure. Since your LES closure is extremely poor, I wonder if air-loss through the LES sufficiently distorts your inspiratory wave shape. Specifically I am thinking that just enough breech through the LES can flatten or otherwise distort your inspiratory waveform, causing a false-positive for FL detection. If so this false-detection scenario should be more prolific at higher pressures I would think.
My earlier charts didn't show any cyclic tendency, so I expanded the data from the past two nights and posted below:
Sessions 13 and 14 are the "night from hell" in Denver when I couldn't stop mouth-breathing. I kept waking up, but would go right back to sleep and start mouth-breathing all over again. Sessions 15 and 16 are from last night back at home. The night with, by far, the most apneas and central apneas was the night in Denver after I ate a large expensive meal, whereas last night I was recovering from the gluttony and ate little in the evening. Judging from this single example, gluttony is contra-indicated for my apnea condition. .
After thinking your hypothesis through a little while, -SWS, it still seems to provide a good explanation for the observed data.
Regards,
Bill
ozij wrote:Friends,
I've just lost almost 2 hours of work trying to compile something on this subject - due to a power failure.
pjwalman was worried about central apneas, had NR (non-resopnsive, therefore suspected central) apneas on a Respironics, and was loaned a PB by Rested Gal so she could see if that machine showed her having central apneas.
The first 2 nights settings ("setting no. 2"):
Peggy's first 2 nights on the PB420E had the following setting
Mode : Pilot : A+AV+IFL2
Min. pressure : 10.0 cmH2O
Initial pressure : 10.0 cmH2O
Max. pressure : 20.0 cmH2O
Max. press. for command on Apnea : 10.0 cmH2O
Ramp duration : 0 min
The results for the sessions when the machine was in use:
Events :
Index/h Apneas : 0.8
Index/h Apneas/CA : 0.6
Index/h Hypopneas : 3.1
Flow limited apneas Hypopneas: 0.5
Number Runs (FL): 230
Index/h Runs (FL): 53.1
And 53% flow limited breaths.
Each of 2 nights sessions had concentrated obstructive events, to which the machine responded sluggishly. There was no chance was those sustained obstructions could be healthy.
My reasoning was that Peggy has far more hyponeas than apneas (PSG and present data), IFL1 off really cuts response to hypopneas, so I suggested she turn IFL1 on and cap the pressure - with the amount of flow lmitation runs she had, I was afraid it would go stratospheric otherwise. I chose 14 because that's what seemed to stabilize her breathing on both nights. She was not having pressure induced apneas, and she was having (to my mind) unnecessary apneas.
Compare the slow respond to the hypopnea buch in session 186 (alas, no snores to push the pressur along) to the fast rise on the first, where snores came along to help.
And note also, on session 187 how the machine does not respond to the apnea - because the maximum pressure for response on apnea was 10.
This it the next configuration:
Min. pressure : 10.0 cmH2O
Initial pressure : 11.0 cmH2O
Max. pressure : 14.0 cmH2O
Max. press. for command on Apnea : 12.0 cmH2O
The worst night for that period had an AHI of 4.9 - and the pressure hung at 14 most of the first night, it did drop, all the way to 10, and go back up agian, on the second night, which had 0 obstructive events, 0 hypopneas with flow limitation, a few snores and a few apneas/ca. Much better, and aerophagia was better too.
Clearly, those NR events on the Respironics were non responsive obstructive events. We thought she may be dreaming at home, needing higher pressure, (1.5 mins of dreaming during the PSG) and maybe swallowing air during the struggle to breath.
The doc. was right about her central apneas being arousal responses.
I think that for some us, the PB mis-identifies flow limited cycles. As a result of that, it has far too many flow limitation runs and response to them pushes the pressure up too much.
On the other hand, when a person does have more hypopneic events, turning IFL1=off may mean they end up with a non responsive (or sluggish, to say the least) machine.
O.
Yep use those settings should pretty much guarantee no response to anything but snore, it cannot respond to Apnea because the Maximum command on apnea is masked by the 10 cm Initial and Minimum pressure settings. If you uncheck any of the two IFLx boxes that will disable any response to FL either stand alone or combined with hypopnea.
I don't understand what one is trying to accomplish with use of those settings?
She can be assured that the "apnea/CA" seen on line 2 of session 183 are CA's with an open airway where cardiac oscillations were seen, that should be listed on the indice page.
I said when she had her Remstar and EncorePro reports that those "NR" events were Central, if you note the pressure she is at on the 420e in session 183 she is again at approximately 13cm pressure, SAME pressure where NR's showed up on her EncorePro reports on a totally different machine.
So how much more proof does one need?
She needs to LOWER her Initial & Minimum pressure to 8.0 and NOT mask off that Maximum "command on apnea" algorythm and ALLOW it to do its job. If the machine is responding TOO agressively to Flow Limitations (not hypopnea) she needs to turn IFL1 off. IF the machine continues to respond agressively remaining FL's associated with Hypopnea she then needs to "try" IFL2 unchecked.
If you shoot at the events seen with shot-gun settings you will never know exactly what parameter works and what doesn't. The conditions which aggrevate breathing and cause CA's to appear is agressive pressure, even constant CPAP pressure may cause them to appear.
She needs a machine that is smart enough to distinquish the difference between obstructive and central events, while the 42Oe is capable of doing that, you are circumventing it from doing that by use of those settings.
She should click on "Default" button under Settings and restore the machine back to default settings, then move Minimum and Initial pressure to 8.0. Leave command on apnea set at 10 cm. She should uncheck the IFL1 box so pressure returns faster to the Initial or Minimum setting sooner. Hanging on with pressure chasing FL's is not what you want when CA's are firing off, that only aggravates the condition.
You have to ask yourself WHY those CA's show up at 13 cm pressure and they don't at 10 cm? Yeah it hurts when I do that, then well don't do that.
Notice the CA just prior to therapy hour 89h, see the vertical dotted line in front of that indicating the "start" of a new session, that is a Sleep Onset CA, probably nothing you can do about that. But those events at hour 87.5 in session 183 are a train wreck.
The object of this game is to have a lower AHI and fewest events possible, that includes CA's and FL runs.
Having a 53% Flow Limited "session" is not my idea of very restfull sleep.
So far (excluding onset events), we know from her EncorePro reports that at 13-14 cm pressure CA's start showing up either as NR on the Remstar or CA on the 420e, nothing there has changed. So how did the 420e respond to those events in session 183?
Note: The machine does appear to increase pressure in session 183 after your red circle, and where you show it blown up with paint, notice the Apnea on line 1 and Central Apnea on line 2 "align" with each other, I would interpret that to be a "mixed" apnea and a break and another one right after it (the train wreck I referred to).
The pressure can resolve the obstructive apnea but it cannot do anything with the central portion left over.
IF I had to guess I'd say she has CSDB based upon those mixed apnea seen and how she responds to CPAP pressure.
First thing I would try is a mask that retains more CO2, flush out or exhaust out too much CO2 and the body's only response it can take is to stop breathing so it retains more CO2. Trying to fight that body response with conventional autopap may be frutile.
She would be better off using a lower pressure and allowing those Apnea that show up show up. This concept of setting pressure up like CPAP ain't gonna work with her condition cause CPAP won't work either, that is why they call it complex.
But I guarantee you if the machine is set up as I suggested and she used a Soyala mask that retains more CO2 she will see the best AHI she's ever seen and sleep like a baby.
Central apnea is a natural body response, if you manipulate breathing with a mechanical device in an adverse way it will adversely respond. In her case too much CO2 is being washed out so the body does the only thing it can that is stop breathing. If she is a shallow breather you are only spinning your wheels trying to address those Flow Limitations cause she's really breathing.
That's my opinion and I'm sticking to it, prove me wrong, I'd love to hear it
Last edited by Snoredog on Wed May 21, 2008 10:11 pm, edited 1 time in total.
someday science will catch up to what I'm saying...
Agreed - and can be seen clearly in the following chart (Tangents /Cathy's) just after hour 66. That hypopnea is long enough after the previous event to be left standing, and next pressure response is to a runs and snore combination.-SWS wrote: So here's the way I interpret the above:
1) Standalone Hypopneas that are unaccompanied by flow limitation should never cause the 420e to increase pressure (regardless of any IFL settings),
Agreed.2) Turning off IFL1 should halt pressure increases to Flow Limitation Runs (but have nothing to do with hypopneas),
An amplitude decreased hypopnea, in the context of a flow limitation run, is responded to and the pressure is raised more than it is to a "stand alone" run. Unlike an apnea/ca which causes a stop, this kind of suspect apnea does not. See first hypopnea after hour 65, and (presumably) single run just before hour 67.
I was trying to say that turning off IFL1 may disable response to amplitude decrease hypopneas that may have been responded to when IFL1=on because they appeared within a run. Edit: that should be a series of runs. Since the detailed record is a representeation based on a minute's data, we don't get a breath by breath response breakdown. But look at the cycles squiggles near the hypopnea not responded to and compare to the area of the one that did elicit response (in the above chart).
Agreed3) Turning off IFL2 will halt pressure increases to any and all hypopneas (I may need to reconsider/revise this---any help appreciated),
Agreed.4) Turning on IFL2 does not at all guarantee that all "H + FL" meets the 420e pressure-increase criteria within the 420e algorithm
To exemplify that last interpretive point, imagine that we place a similar soft-switch or trigger for hypopneas in the Respironics algorithm, while leaving the algorithm otherwise intact. Let's call that trigger or soft-switch "RH2". As patients or clinicians we might turn "RH2" off to ensure the Remstar does not respond to any hypopneas whatsoever. But if we turn "RH2" on, hypopnea response reverts to factory defaults: not all hypopneas cause a pressure increase. In this hypothetical Remstar case, when factory-defaulted hypopnea response is enabled (w/ "RH2" on), initial hypopneas still receive no pressure; nor do any hypopneas receive pressure once NRAH criteria has been met.
I see IFL2 as a switch to alternately disable hypopnea response altogether, or to allow a "selective" hypopnea response to occur according to the 420e algorithm's own internal criteria.
All APAP manufacturers seem to take a conservative approach to hypopnea pressure increase.
Agreed. And remember how Derek (with a preponderance of hypops) found he did much better on the Respironics' fixed mode than on auto.
Interesting, and making sense.Bill, you mentioned above that your FL runs seem worse at higher pressure. Since your LES closure is extremely poor, I wonder if pressurized air-loss through the LES sufficiently distorts your inspiratory wave shape. Specifically I am thinking that just enough breech through the LES can flatten or otherwise distort your inspiratory waveform, returning a false-positive from the 420e's ultra-sensitive FL detection routine. If so this false-detection scenario should be more prolific at higher pressures I would think.NightHawkeye wrote:It was when I raised the minimum pressure that the "runs" began to occur on a more-or-less continuous basis
Clapping.I definitely agree with that. However, I think this 420e "FL magnifying glass" (regarding such close FL wave-shape scrutiny) is a double-edged sword that Rapoport probably put in place intentionally. I'll try to speculate more about that soon, as long as no one boos my wild and crazy conjecture off the stage....ozij wrote:I think that for some us, the PB mis-identifies flow limited cycles. As a result of that, it has far too many flow limitation runs and response to them pushes the pressure up too much.
http://ajrccm.atsjournals.org/cgi/conte ... /150/2/475
Am. J. Respir. Crit. Care Med., Vol 150, No. 2, 08 1994, 475-480.
Optimizing flow contour (IFL1=on?)may be an alternative to eliminating apneas in evaluation of the optimal therapeutic level of CPAP in OSAS (IFL1=off?).Flow limitation as a noninvasive assessment of residual upper-airway resistance during continuous positive airway pressure therapy of obstructive sleep apnea
R Condos, RG Norman, I Krishnasamy, N Peduzzi, RM Goldring and DM Rapoport
Department of Medicine, New York University Medical Center, New York 10016.
Many patients with obstructive sleep apnea syndrome (OSAS), despite therapy with nasal continuous positive airway pressure (CPAP), have persisting daytime somnolence that may be due to a persistently elevated upper-airway resistance associated with electroencephalographic (EEG) arousals. We tested the hypothesis that elevated upper-airway resistance can be inferred from the contour of the inspiratory flow tracing obtained from a conventional CPAP circuit. This may provide a noninvasive method for determining optimal CPAP. Data were collected during a CPAP titration of an upper-airway model and in eight patients with OSAS. Estimated inspiratory resistance was calculated from esophageal pressure, CPAP mask pressure, and inspiratory flow. At high CPAP, resistance was low and inspiratory flow contour was found to be rounded. At low CPAP, resistance was high and flow contour developed a plateau suggesting flow limitation. We also noted that the CPAP pressure at which high resistance developed, and at which flow limitation appeared, showed hysteresis. We conclude that when respiration is stable, the contour of inspiratory flow tracing from a CPAP system can be used to infer the presence of elevated upper- airway resistance and flow limitation. Optimizing flow contour may be an alternative to eliminating apneas in evaluation of the optimal therapeutic level of CPAP in OSAS.
Two ways of doing the therapy? Micro responses to correct the contours?
Rapaport seems to working on his algorithm -
http://patft.uspto.gov/netacgi/nph-Pars ... EF/6488634
This a new (2006) application
http://www.google.com/patents?id=h9KXAA ... dq=6488634
_________________
CPAPopedia Keywords Contained In This Post (Click For Definition): cpap mask, 420E, respironics, Titration, CPAP, Hypopnea, auto, APAP
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
Last edited by ozij on Thu May 22, 2008 2:16 am, edited 1 time in total.
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Bill: Sessions 15 and 16 look a whole lot better than 13 and 14, I wouldn't change my diet for any cpap machine
I wonder if the altitude of Denver had more to do than anything on those nights from hell? What is the altitude at home?
That machine is supposed to be auto-adjusting but my top-fuel dragster doesn't run so well there either.
I wonder if the altitude of Denver had more to do than anything on those nights from hell? What is the altitude at home?
That machine is supposed to be auto-adjusting but my top-fuel dragster doesn't run so well there either.
someday science will catch up to what I'm saying...
Ozij: I think what we are failing to account for when dissecting weather or not the machine has responded to an particular event is the "waits" and timing parameters the machine has to follow based upon its algorithmic flow chart.
If you observe Figure 10 in the 2006 Patent link (page 6 of 13 in the drawings section), you will see some of those waits and pauses, some are 30 seconds long, others are 2 minutes. So if the machine doesn't "appear" to respond to a particular event it could very well be some of those intentional pauses such as shown in Figure 10's flow chart decision tree on manipulation of pressure.
If you observe Figure 10 in the 2006 Patent link (page 6 of 13 in the drawings section), you will see some of those waits and pauses, some are 30 seconds long, others are 2 minutes. So if the machine doesn't "appear" to respond to a particular event it could very well be some of those intentional pauses such as shown in Figure 10's flow chart decision tree on manipulation of pressure.
someday science will catch up to what I'm saying...
I edited something in my above post, here it is again.
I was trying to say that turning off IFL1 may disable response to amplitude decrease hypopneas that may have been responded to when IFL1=on because they appeared within a run. Edit: that should be a series of runs. Since the detailed record is a representeation based on a minute's data, we don't get a breath by breath response breakdown. But look at the cycles squiggles near the hypopnea not responded to and compare to the area of the one that did elicit response (in the above chart).
More about flow limitation runs, from the patents, all emphasis mine, (you can skip the non underlined text):
http://www.google.com/patents?id=-Q8KAA ... dq=6488634
Somtimes (Always?) IFL1 follows the slope method - depending on percentage of flow limited breaths?
When a person has a larger percentage of flow limited breaths (etiology unknown) and IFL is on, Max. is meant to be be capped?.
Facts:
My PSG - and in general 420E recommended pressure with IFL1=off is 7.
For RG, the PSG, and in general recommended pressure with IFL1=off was 9.
O.
I was trying to say that turning off IFL1 may disable response to amplitude decrease hypopneas that may have been responded to when IFL1=on because they appeared within a run. Edit: that should be a series of runs. Since the detailed record is a representeation based on a minute's data, we don't get a breath by breath response breakdown. But look at the cycles squiggles near the hypopnea not responded to and compare to the area of the one that did elicit response (in the above chart).
More about flow limitation runs, from the patents, all emphasis mine, (you can skip the non underlined text):
http://www.google.com/patents?id=-Q8KAA ... dq=6488634
Wild assumptions:"In particular, the invention relates to a breathing device and method of use to adjust a controlled positive pressure to the airway of a patient by detecting flow limitation from analysis of an inspiratory flow waveform.
The system calculates the relative flow magnitude index as the peak flow of the inspiratory flow waveform minus the peak flow of the previous inspiratory flow waveforms showing flow-limitation divided by the running average of the peak flows of the non-limited breaths minus the average of the flow-limited breaths. This parameter is calculated as: ##EQU1##
WHERE:
FLOW is the peak flow rate of the current breath
MIN is an average of the peak flow of the 20 most recent flow limited breaths.
MAX is an average of the peak flow of the 20 most recent normal breaths.
This results in a parameter or index which ranges from 0 (flow limited) to 1 (normal).
The four shape detection parameters described above are calculated for the current valid breath and the values are combined using a mathematical function, such as a logistic regression sum. Similarly, weighting factors may be used, wherein the weight given to one or more of the indexes may be zero, positive or negative. The combined values provide a flow limitation parameter which has a value between 0 and 1 that characterizes the likelihood that the current breath has a shape characteristic of flow-limitation. The value of the flow limitation parameter is further modified based on the value of the preceding breaths' flow limitation parameters used as a prior probability, allowing calculation of a posterior probability.
The four shape detection parameters (sinusoidal index, flatness index, respiratory effort index and relative flow magnitude index) are used in a mathematical function to determine a likelihood of flow limitation using a logistic regression equation: ##EQU2##
Where "p" is the probability of flow limitation; "e" is the base of the natural logarithms; X1, X2, X3 and X4 are the shape detection parameters; B0, B1, B2, B3 and B4 are the weighting coefficients (which may include zero) and
The probability of flow limitation (p) has a limited range from 0 (flow limitation) to 1 (normal) and is valid for all values of the function f(x).
FIG. 16 shows the prior probability factor which is applied to the initial value of the flow limitation parameter calculated from the shape parameters to yield a final value for the current valid breath. The prior probability factors are used to modify the flow limitation parameter based on previous breath's value for flow limitation. The underlined value is an estimate of the best value to be used as a multiplicative or additive to the index. Thus, the flow limitation parameter is made more important when other flow limited breaths have been detected. Similarly, the index is made less "flow limited" if the present occurrence is an isolated incident.
If the flow limitation parameter is between 1 and a predetermined normal reference value, e.g., 0.65-0.8, then the breath is classified as "normal." If the flow limitation parameter is between 0 and a predetermined flow limited reference value, e.g., 0.4, then the breath is classified as "flow limited." If the flow limitation parameter is between the normal and flow limited reference values, then the breath is classified as "intermediate."
As each valid breath is identified, its likelihood of being flow limited is calculated. The flow limitation parameter approaches a value of 1 for a normal breath and 0 for a flow limited breath. In the method of the present invention, a decision is made as to whether to adjust the controlled positive pressure. This decision is dependent on three factors:
1) the value of the flow limitation parameter for the current breath;
2) the value of the flow limitation parameters in the preceding interval (several breaths);
3) whether the controlled positive pressure has been adjusted (and the direction) in the preceding interval of time.
Generally, if flow limitation is detected, the controlled positive pressure will be raised. Similarly, if no flow limitation is detected for an interval of time, then the controlled positive pressure is lowered to test for the development of flow limitation. The desired effect of the method of the present invention is for the controlled positive pressure to remain slightly above or below the optimal positive pressure despite changes in the optimal therapeutic level of pressure which may occur over time.
<snip> [description of decision tree comes here, O.]
Alternatively, the controlled positive pressure may be continuously adjusted at a rate set by a slope parameter, e.g., 0.1 cm per two seconds. The slope parameter and its sign would then be updated based on each breath's flow limitation parameter. In no event can the controlled positive pressure be set below the low limit or above the high limit reference values.
Somtimes (Always?) IFL1 follows the slope method - depending on percentage of flow limited breaths?
When a person has a larger percentage of flow limited breaths (etiology unknown) and IFL is on, Max. is meant to be be capped?.
Facts:
My PSG - and in general 420E recommended pressure with IFL1=off is 7.
For RG, the PSG, and in general recommended pressure with IFL1=off was 9.
O.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023