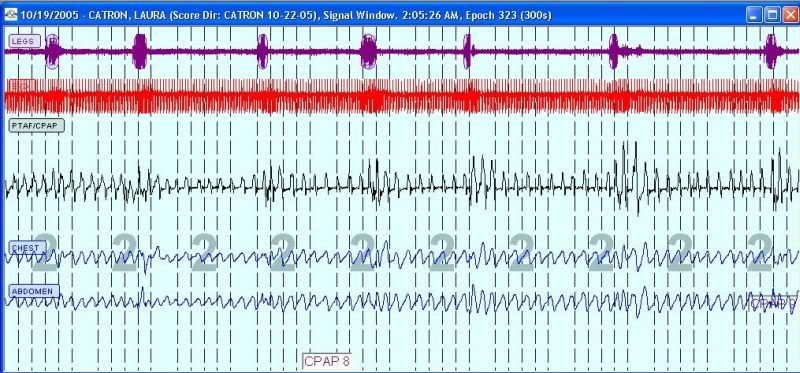
It sure is starting to sound like the ASV is, overall, your better modality between those two. AHI certainly improves with ASV modality---despite tidal volumes showing more variation. More importantly, it seems that you report better daytime symptoms when using the ASV versus CPAP.blizzardboy wrote:So last night (http://users.adam.com.au/sixsome/ASV/0510/051910/) I did an experiment comparing fixed CPAP@9.6 to ASV with EEP=9.4 and PS=4->9. Switching at 0330, when I awoke temporarily, there is quite a dramatic difference in my response to the two settings. I am particularly interested in the increase in baseline resp rate and reduction in resp variation following transfer to ASV. Please note that when I awoke this morning I had no joint pain. Having the ASV setup like that reminded my of when I used the Bipap ASV machine during my trial period, in that I could feel a more dramatic dump of air from my lungs when the machine dropped back to the EEP phase of the cycle. Also interesting to note that I first experienced joint pain when I went onto the S9 part of my trial period, which immediately followed my trial of the Bipap ASV.
Well, Muffy usually gives us good advice IMO. I would want the complete PFT as well if I were you.blizzardboy wrote:One thing that I hadn't thought to mention was that between the ages of 15 until 27 I suffered from chronic lungs infections (at least 2 per year). During this period I had regulary bouts of acute stomach pain and associated vomiting and nausea, once causing me to be hospitalised. I had a tests over this time but no-one ever found a cause. Finally, at the age of 27, during a work trip to Germany, I had a similar bout of stomach pain and vomiting but this time I got really sick. I crawled through the suburb I was living in a eventually located a doctor who proceeded to poke my appendix and nearly sent me through the roof. I was rushed to hospital and had an emergency appendectomy. Since that time (11 years) I haven't had one bout of stomach pain or a lung infection. I just wonder if 12 or so years of lung infections has taken its toll on my lungs some how? Maybe not on MVV, but on gas exchange efficiency?
Anyhow, let's see what comes of a comprehensive pulmonary function examination. I am now determined to make this happen!
Your outstanding slight flow limitations above 10cm might not even pose a significant sleep problem for you by the way of outstanding RERA's. And there's always the chance that attempting to address those flow limitations with higher pressures might create more machine-sourced problems or arousals than resolved. I suppose I would eventually get around to experimenting with higher pressures---since your doctor already approved that---to see if eliminating presumed flow limitations above 10cm enhanced daytime symptoms or slightly deteriorated daytime symptoms.blizzardboy wrote:So maybe the issues at play are (1) I need sufficient base pressure to keep my airway open and then (2) I need enough differential between IP and EP to ensure adequate ventilation of my lungs. Let's see what comes of it all.
Note that flow limitations occur during inspiration. So they can be addressed with either base pressure (EEP) or IPAP. The current Resmed Adapt SV titration protocol prefers getting them with IPAP (thus increasing min PS as your doctor suggested). By contrast, the Respironics protocol starts with CPAP as base, and thus EPAP (EEP equivalent) increases are necessary to address those flow limitations by virtue of the CPAP base modality itself. Despite the Adapt SV suggested protocol preferring IPAP increases to address outstanding flow limitations, we can see in this excerpt that Dr. Brown's team chose to address them with EEP increases: viewtopic.php?f=1&t=51063&p=478152&hilit=brown#p478152