http://pulmccm.org/main/2014/randomized ... a-70-nejm/
Hypoglossal Nerve Stimulation Markedly Improves OSA
An estimated 15% of men and 6% of women in the U.S. have clinically significant obstructive sleep apnea, meaning it worsens their daytime cognitive functioning, cardiovascular risk, or both. In obstructive sleep apnea, muscle tone in the soft tissues of the pharynx (throat) is insufficient to prevent them from intermittently collapsing during sleep, usually because of obesity. With each closure of the upper airway (failed breath, or apnea), hypoxemia and heart strain can occur, relieved when the sleeping brain arouses itself just enough to “buzz” the pharyngeal muscle tissues with enough nerve stimulation to restore muscle tone, airway patency and airflow. Because this almost all happens without frank awakenings, most people with obstructive sleep apnea are unaware of their nocturnal troubles or their severity.
Continuous positive airway pressure delivered by mask to the nose or face can dramatically improve obstructive sleep apnea, and probably reduces the risk for cardiovascular complications in severe OSA (this part may never be proven: the benefit has been suggested strongly enough in observational studies that long-term randomization to placebo/sham would be considered unethical for severe OSA). However, most people with obstructive sleep apnea are not treated at all, and fewer still wear CPAP consistently enough to get its full benefit (which probably requires 7 hours a night). Custom oral appliances are less effective, and have always been a “boutique,” cottage industry, never a plausible public health solution.
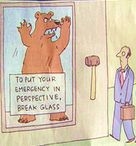
So we have a chronic, largely incurable medical condition affecting a large proportion of U.S. citizens, most of whom can’t or won’t use the best available noninvasive treatment. A glass-half-empty person might get mopey and whine about the human consequences of the obesity epidemic, perverse incentives in U.S. food policy, blah, blah, blah. But not Medtronic, one of the world’s largest device manufacturers best known for its implantable cardiac defibrillators and pacemakers.
Medtronic’s engineers put together the Inspire I, an implantable hypoglossal nerve stimulator, with a lead in the base of the tongue that triggers when an implanted intrathoracic pressure sensor detects inspiratory efforts. Back around 1999, Alan Schwartz et al implanted the Inspire I device in 8 patients with severe obstructive sleep apnea. It worked brilliantly, improving the apnea-hypopnea index (AHI) by >50% without adverse effects at 6 months, although five of the devices stopped working (it was a prototype). Sensing opportunity, Medtronic spun the company off as Inspire Medical Systems, but remains its largest investor, according to Inspire’s website. Several other small trials have demonstrated the feasibility of hypoglossal nerve stimulation since then; at least one negative trial has reportedly occurred, but is apparently unpublished.
This month, Patrick Strollo, Kingman Strohl et al report the results of the STAR Trial, a multicenter cohort study to test the latest version of the Inspire device on a larger group of people with obstructive sleep apnea, in the New England Journal of Medicine.
What They Did
Investigators enrolled subjects aged 31 to 80 (mean 54) with moderate-to-severe OSA (mean AHI ~32) and a history of nonadherence with CPAP. Most were men, overweight but not obese (mean BMI 28; patients with BMI over 32 were excluded). All screened patients had to undergo upper endoscopy with airway visualization during sedation-induced sleep, excluding those unlikely to benefit from nerve stimulation.
They then surgically implanted the Inspire device into 126 patients, usually during an overnight stay in the hospital:
sleep review randomized controlled trials n engl j med review cardiovascular disease review Implantable tongue buzzer improves obstructive sleep apnea by 70% (NEJM)
Patients were followed for a year, with the primary outcomes of AHI and oxygen desaturation index (ODI, or number of times per hour oxygen saturation falls >= 4% from baseline). There was no control group; patients were their own controls (before/after treatment).
The study was funded by Inspire Medical Systems, but with significant scholarly independence by the authors and participation by the FDA in trial design.
What They Found
At 12 months, the median AHI score fell by 68% (from median 29 to 9) and the ODI by 70% (from 25 to 7). Also,
•Two-thirds of patients had at least a 50% reduction in AHI to a final score of <20 per hour.
•75% of patients had a reduction of at least 25% in their ODI score.
•Epworth Sleepiness Scale scores also fell by ~2 points, to the normal range (<10), in most patients.
Authors then selected 46 of the patients who responded best to therapy, and randomized half of them to have their devices turned off for a week. Their AHI scores shot up (~8 to 26) while the therapy-continuers’ scores rose by 1.7/hour; ODI scores followed a similar pattern. (Why do this? To rule out improvement due to time, weight loss, diet, etc., since there were no true controls.)
Two patients experienced severe discomfort requiring the device to be surgically repositioned. 18% had temporary tongue weakness post-op, which resolved. 40% of the patients reported discomfort during stimulation. Also, 20% of patients had tongue soreness or abrasion of their tongue, as the muscle stimulation caused the tongue to repetitively slide along the bottom teeth.
What It Means
I had heard that wearable devices were the hottest new trend in tech, but I wasn’t expecting this. Will this be what you move up to if the FitBit doesn’t do the trick?
But seriously, folks. There are a lot of people with untreated severe obstructive sleep apnea out there who just can’t tolerate CPAP, a few of whom might choose what could be a “one and done” surgical procedure to improve their daytime functioning or reduce their high cardiovascular risk. People with previous MIs or strokes, for example, might be considered good candidates. Although the Inspire device didn’t “cure” obstructive sleep apnea (reduce AHI to the normal range), neither does CPAP, in most people with severe OSA (a substantial reduction in AHI is considered success). These are impressive reductions in apneas and overnight hypoxemia, and assuming longer-term safety, the device looks like a successful treatment for OSA — making it the first new therapy for the condition since CPAP was first tested in 1980.
It should also be noted that a competing company’s hypoglossal stimulator (Apnex Medical) did not show a benefit in its own randomized trial, according to the NEJM editorialist (no reference provided; these negative trials often don’t get published). Apnex went bust shortly after that trial concluded. The Inspire device, on the other hand, is already approved and in use in Europe; the FDA is currently reviewing safety and efficacy data to decide approval in the U.S.
Health care penny-pinchers may balk at the likely five-figure price tag the Inspire device will bear (when combined with fees for a surgery and overnight hospital stay) and Medtronic’s 21% profit margin for its devices, but that may be a tempest in a teapot. I’m not predicting a rush by patients with sleep apnea to get this device implanted in their bodies; unlike sudden cardiac death, OSA just isn’t scary enough to induce most people to undergo endoscopy and surgery. Also, after considering the health care costs of long-term DME contracts for CPAP, the device may not be as expensive as it first appears.
Nevertheless, for the foreseeable future (assuming FDA approval), I see this as a niche product, implanted into two categories of CPAP-averse patients: high-functioning people with significant impairment from OSA who see it as a better alternative to “UPPP” surgery (which has a much weaker evidence base); and people at high cardiovascular risk who view the procedure as potentially lifesaving. The large majority of people with OSA who don’t use CPAP seem to me to feel the hassle or discomfort outweighs the potential benefits; their curiosity about this procedure will end upon hearing the phrase “surgically implanted electrode.”
Patrick J. Strollo, Kingman P. Strohl, et al. Upper-Airway Stimulation for Obstructive Sleep Apnea. N Engl J Med 2014; 370:139-149. DOI: 10.1056/NEJMoa1308659
Implantable tongue-buzzer improves obstructive sleep apnea b
-
ScubaSleeper
- Posts: 5
- Joined: Fri Jan 17, 2014 4:02 am
Re: Implantable tongue-buzzer improves obstructive sleep apnea b
Hmmm...interesting, something to watch. Thanks.
_________________
| Machine: ResMed AirSense™ 10 AutoSet™ CPAP Machine with HumidAir™ Heated Humidifier |
| Mask: ResMed AirFit N30 Nasal CPAP Mask with Headgear |
Re: Implantable tongue-buzzer improves obstructive sleep apnea b
The study is fully described here:
http://www.nejm.org/doi/full/10.1056/NEJMoa1308659
Results are not a miracle but encouraging, I think.
http://www.nejm.org/doi/full/10.1056/NEJMoa1308659
Results are not a miracle but encouraging, I think.
_________________
| Mask: ComfortGel Blue Nasal CPAP Mask with Headgear |
| Additional Comments: Breas iSleep 25 (bilevel) with its own humidifier |
Re: Implantable tongue-buzzer improves obstructive sleep apnea b
A while back we had a couple of forum members who had this procedure and we got some input on it but haven't had any follow up in a long time...
If you search the forum for hpyoglossal you should be able to find the prior discussion.
I think those members were part of an initial field study. Guinea pigs sort of.
If you search the forum for hpyoglossal you should be able to find the prior discussion.
I think those members were part of an initial field study. Guinea pigs sort of.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
- Sir NoddinOff
- Posts: 4190
- Joined: Mon May 14, 2012 5:30 pm
- Location: California
Re: Implantable tongue-buzzer improves obstructive sleep apnea b
Good stuff. Thanks scubasleeper et al. Years from now there may well be a piezo electric type of tissue stent that can be implanted in the throat (or even grown in the throat) that would provide a supporting lattice capable of opening one's airway 100%. No more CPAP machine.
_________________
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Additional Comments: Sleepyhead software v.0.9.8.1 Open GL and Encore Pro v2.2. |
I like my ResMed AirFit F10 FFM - reasonably low leaks for my ASV therapy. I'm currently using a PR S1 AutoSV 960P Advanced. I also keep a ResMed S9 Adapt as backup. I use a heated Hibernite hose. Still rockin' with Win 7 by using GWX to stop Win 10.
Re: Implantable tongue-buzzer improves obstructive sleep apnea b
When they develope the technology to transport medical devices in and out of my body, without surgery, maybe. One invasion of my body for implant wasone too many. Jim
Use data to optimize your xPAP treatment!
"The art of medicine consists in amusing the patient while nature cures the disease." Voltaire
"The art of medicine consists in amusing the patient while nature cures the disease." Voltaire
Re: Implantable tongue-buzzer improves obstructive sleep apnea b
Great post. Ecouraging. Awhile back I read somewhere about an implant that could/might also prevent central apneas. Would this likely do that as well?
Sir NoddinOff:
"Good stuff. Thanks scubasleeper et al. Years from now there may well be a piezo electric type of tissue stent that can be implanted in the throat (or even grown in the throat) that would provide a supporting lattice capable of opening one's airway 100%. No more CPAP machine"
I hope you're right. Maybe one day folks will look back on this as the "cpap era." A sort of iron lung stage in the early development of the therapy.
The sooner the better!
Sir NoddinOff:
"Good stuff. Thanks scubasleeper et al. Years from now there may well be a piezo electric type of tissue stent that can be implanted in the throat (or even grown in the throat) that would provide a supporting lattice capable of opening one's airway 100%. No more CPAP machine"
I hope you're right. Maybe one day folks will look back on this as the "cpap era." A sort of iron lung stage in the early development of the therapy.
The sooner the better!
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: ResScan 4.3 software, 50D+ Oximeter |