Post
by lostsheep » Wed Nov 07, 2012 10:54 pm
A forum member inquired as to my status, so here's an updated summary of my experience so far (with some repeat of previous posts):
I've now been on the VPAP for about 5 weeks. Before the VPAP I used a CPAP, mostly set at 7 inH2O. After 6 months on CPAP I wasn't feeling energetic at all, and I could see that my breathing waveforms often looked a bit flattened or jagged. From Dr. Krakow (web info) I learned that this might indicate sub-optimal therapy. My hope with trying VPAP was that I could go to a higher pressure, and get more therapeutic benefit.
Looking back at my original lab titration, there was a mention of centrals showing up with increased pressure. I think that is why it was prescribed only 7 inH2O. But I wanted to see if I could adapt to more pressure with some time on VPAP.
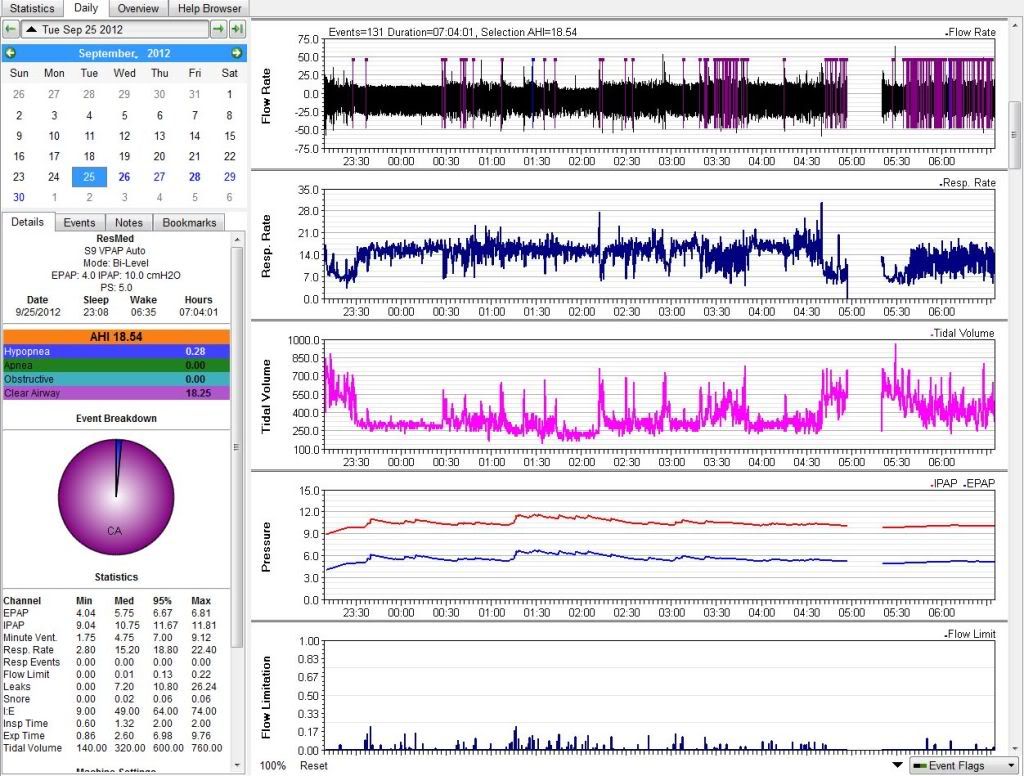
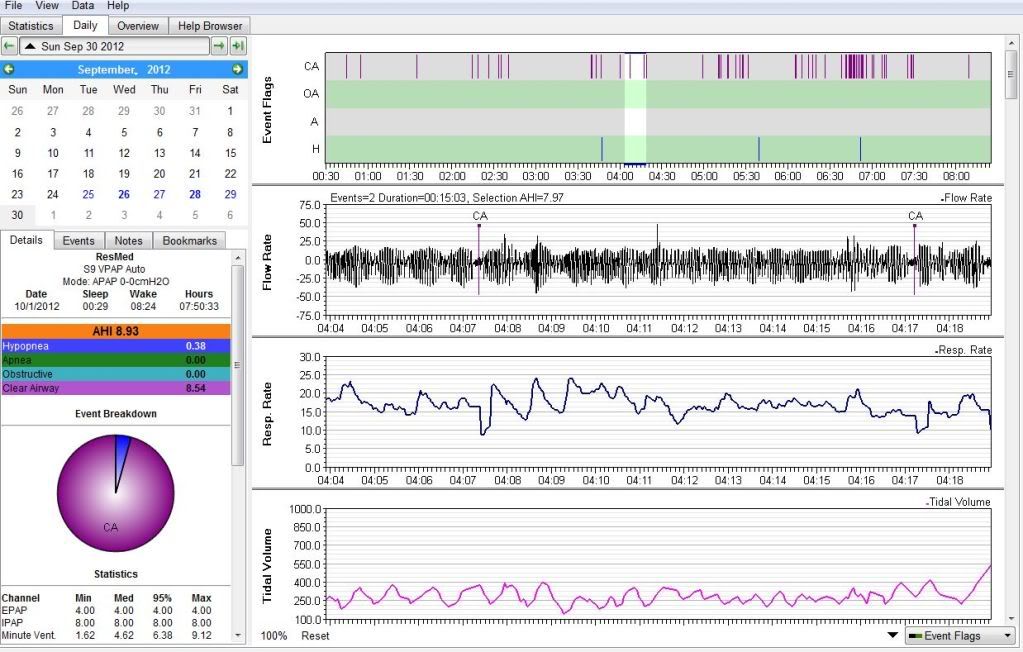
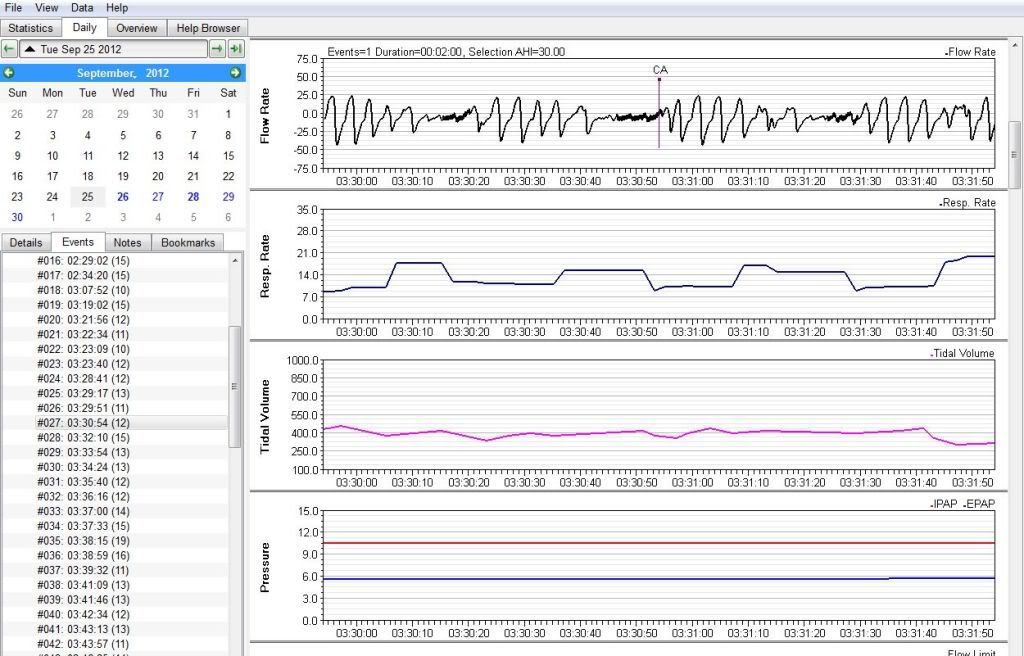
The first night, with VPAP on auto mode, I saw pressure go up to something like 10 or 12, with lots of periodic breathing and a huge incidence of centrals (shown in previous post). I felt terrible the next day. I then set the pressure to constant 8/4, and have left it there ever since. About a week into this, I discovered that I really like the "easy breath" setting. I'm reasonably comfy with my current mask so it feels OK when I go to sleep - well, enough that I don't lie awake if I'm tired. Should be all good, right?
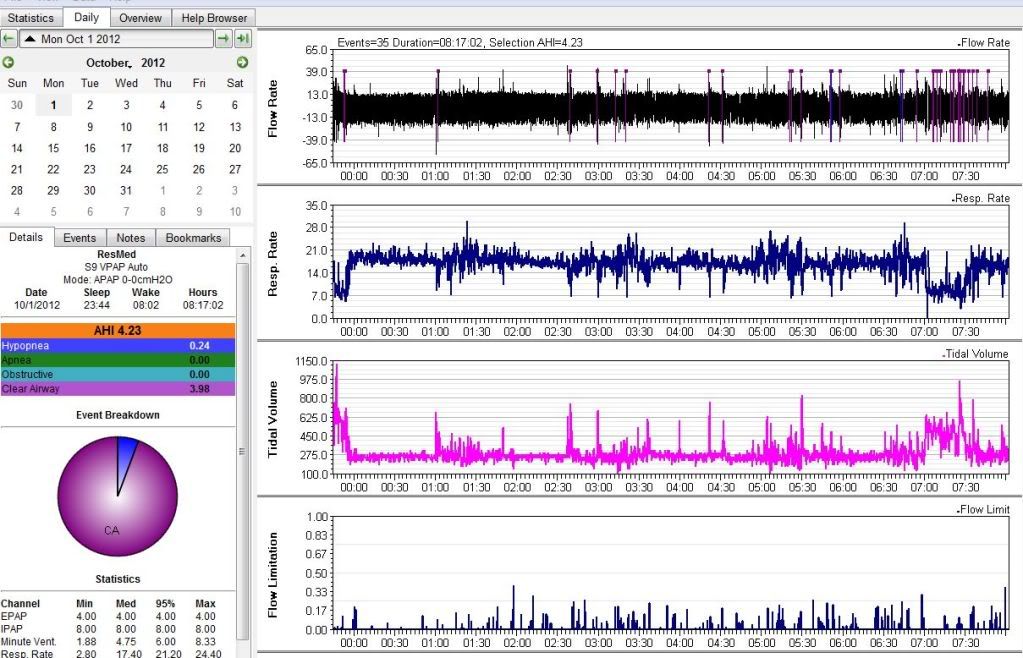
In the morning I typically see AHI's from 3-6, almost all CA's, and I've noticed there is a relationship between the AHI and and how I feel in the AM - and pretty much all day. But I never really feel right. I also notice a dull headache some mornings. Typically I am slow to wake (which is NOT me), and don't feel like I am well rested - sort of mentally foggy, sometimes bad enough that I want to nap. I have no physical stamina now - I get tired from just a few hours of normal exertion.
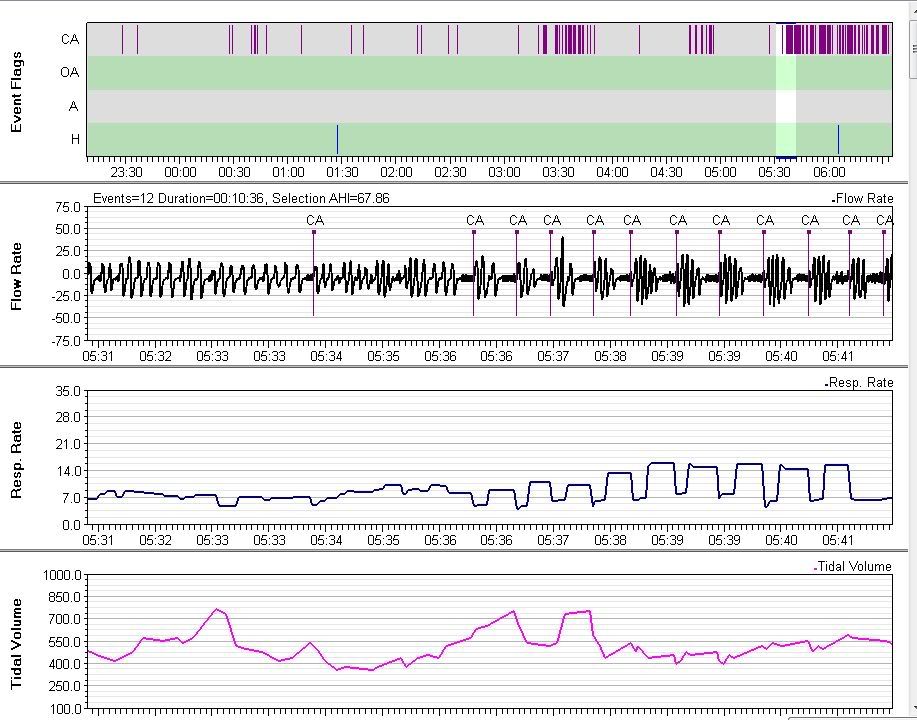
When I look at the data now there is still some periodic breathing, but I'd say most of the night it looks fairly regular. Also, when looking at CA events I notice that oftentimes, a few breaths before the breathing pause (flagged as a central), my breathing rate transitions to resemble the wake-state. So maybe something is going wrong to disturb my sleep - or it could just be part of the periodic breathing thing. Of course I don't remember any of this.
I wonder if I'm having an issue with pressure therapy in general, perhaps CO2 overload (hypercapnia). This has been vaguely suggested by both an RT and sleep doctor.
Recently I tried sleeping without the VPAP for comparison - first time in 7 months. (I'm staying on my side, as I know I can get at least some REM sleep this way. I'm not too worried about big desats - my main issue w/o XPAP seems to be poor sleep architecture.) I only did it for one night, but it seems I did wake up more alert (and no gas that day ). No, I haven't decided to sack the VPAP over the long term, but I am becoming skeptical. It seems this therapy solves one problem while causing another.
I was offered a trial period with ASV, but that seems even more imposing for my brain/body.
I've decided to get a second opinion, which probably involves a follow-up sleep study & titration. I made an appointment with a research hospital (National Jewish) in Denver, as I'm told they are quite capable and have the respiratory expertise to figure out therapy issues. Even though I have a sleep doctor that I like, I am initiating the next step.