Hi SWS, Kiralynx, and any other ventilator users,
I've got a good bit of data to insert so let's proceed:
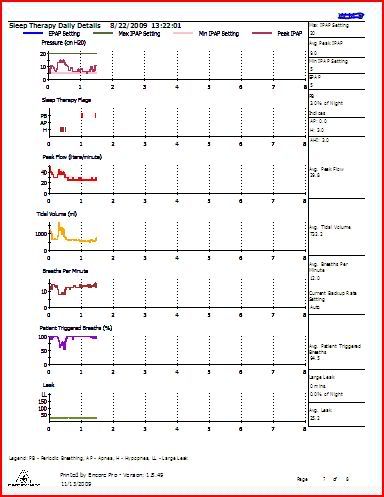
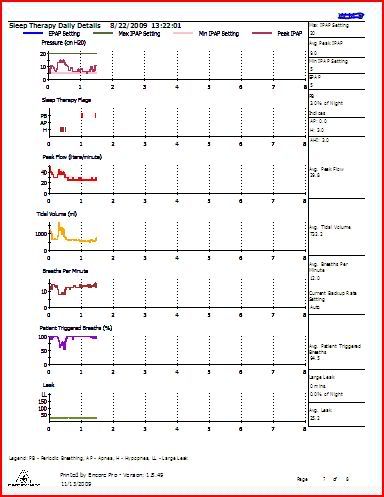
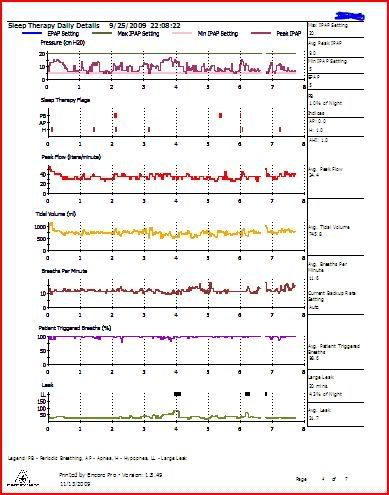
This report from 8-22 shows a nap, not a full night. What was interesting about this one was the fairly complete decoupling of the hypopneas and the periodic breathing. Note the time gap between the events. I suppose you could say this is an example of PB without hypopnea. Or, an example of PB not triggered by hypopneas. Mask was the ResMed Mirage Micro.
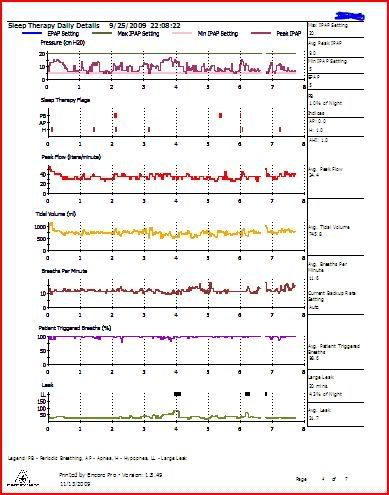
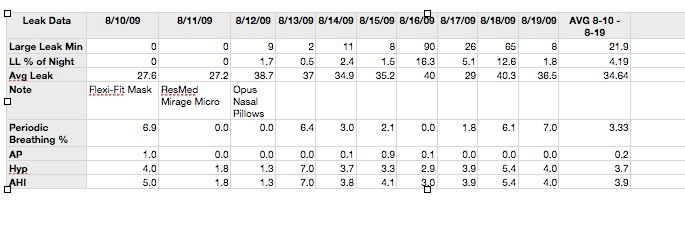
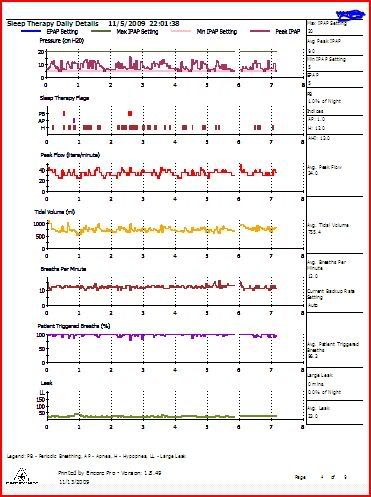
Here is a different example from just over a month later:
On this report date the PB seems incidental to the hypopneas. Apneas are 0, AHI 1.0. Large leaks are excessive - restless night?? Mask was the ResMed Mirage Micro.
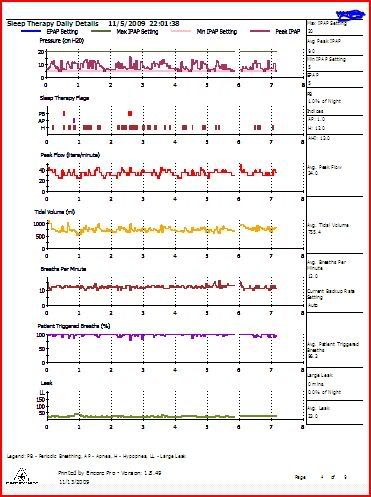
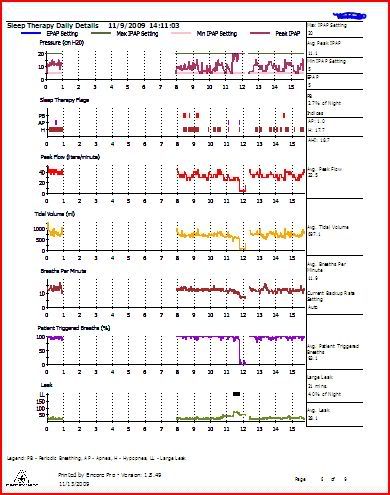
Next, we skip ahead to November 5:
Here, the hypopneas are taking over! I have some reports with even more hypopneas than this. Yet, with all these hypopneas, periodic breathing is not a prominent factor. I tried as you suggested SWS, to find a report with lavish PB and low hypopneas, but I don't seem to generate that rare a bird. I do, however, recently produce loads of hypopneas with some PB.
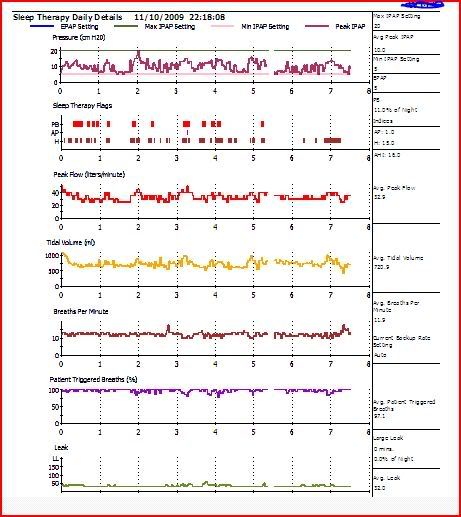
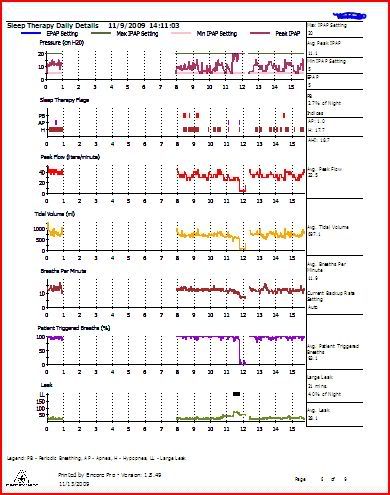
My final exhibit is for the night of November 9, the night before my first report, above, which started this whole conversation:
This report shows some clear hypopnea clusters upon first donning re-donning the mask, which in this case is the Swift LT nasal pillows.
I'm thinking my brain doesn't reset for the right amount of CO2 when I'm dozing off, or some other part of that complex mechanism isn't working properly.
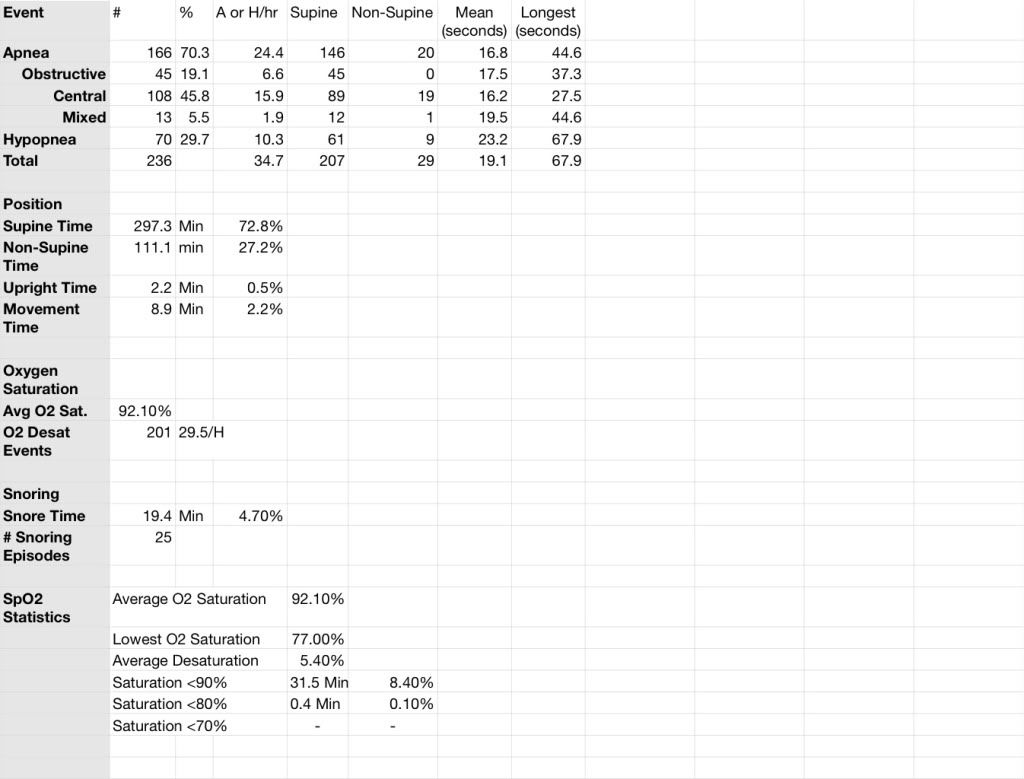
So, you now have four reports from fairly early to pretty recent. Hopefully this will allow for a more complete view than the single data point in my first message. To round this out, here is some data I extracted from my original sleep report.
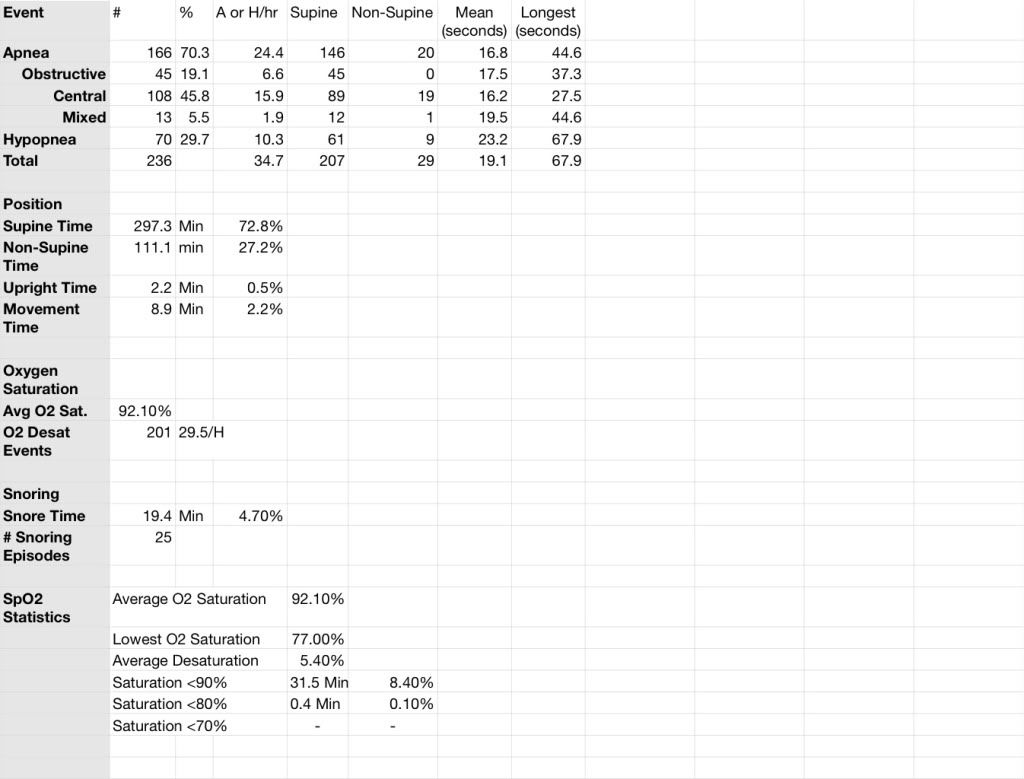
I am sorry, but it is very hard to get everything to line up when you do a spreadsheet. A little study should reveal what everything means. Questions? Ask away, and I'll try to answer. Oh yes, this was an "at home" sleep study, not a full sleep study done in a lab.
I get to see one of the RTs at Kaiser on the 24th. I am to get a pulse oximeter for one night to see what my O2 saturation levels are doing. Since I was never titrated on my ventilator, she may be willing to reset some parameters. SWS, your suggestions will certainly play a part in our conversation. I think she is expecting to download my smart card and get the standard seven days of data. What will she say when she sees my notebook with reports for almost every night and nap since I started in August?
Let me know what you think of all this data. Of course, if there is anything else that will help, let me know and I'll try to provide it.
Thank you in advance, and
Happy Naps,
Mr Capers