- 24 years old, Male, muscular build, not overweight
- No history of gut issues prior to CPAP
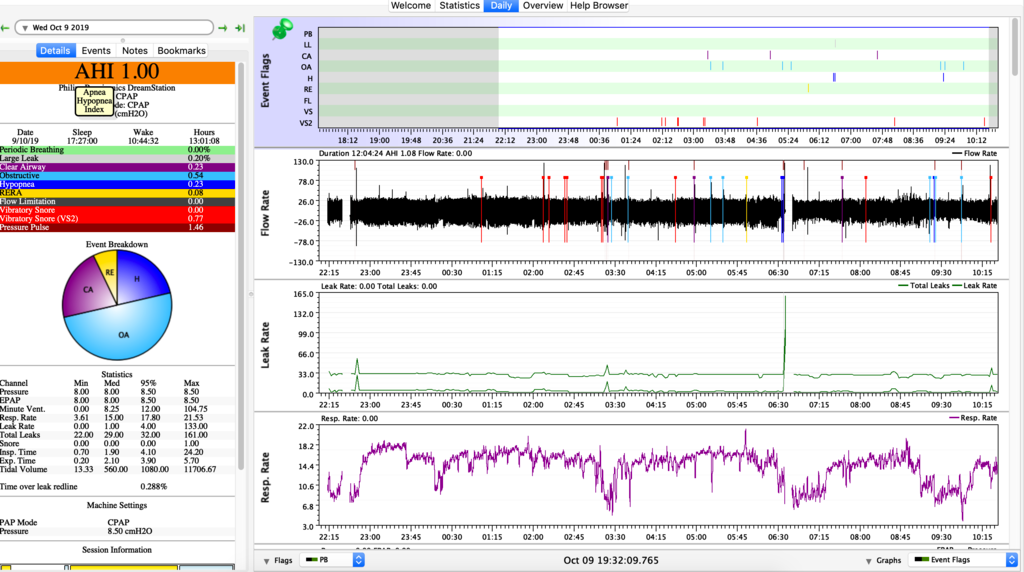
- Current pressure - 8 - No CFLEX
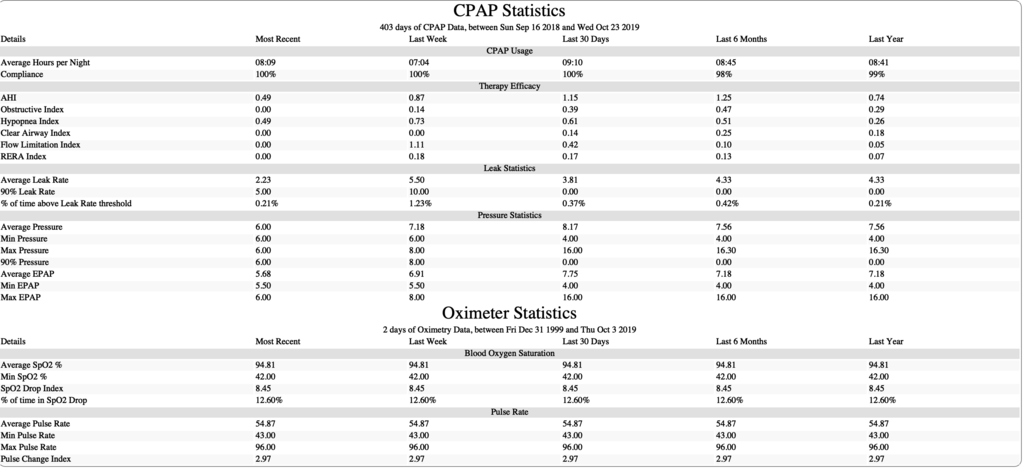
- Used CPAP for a few years
Main issues
- Cognitive issues, bloating, anxiety & depression, bloating when I use CPAP
- Mind feels blank. Suspected circulatory issues due to hyperventilation. Hyperventilation exacerbated by air swallowing/aerophagia?
Overview
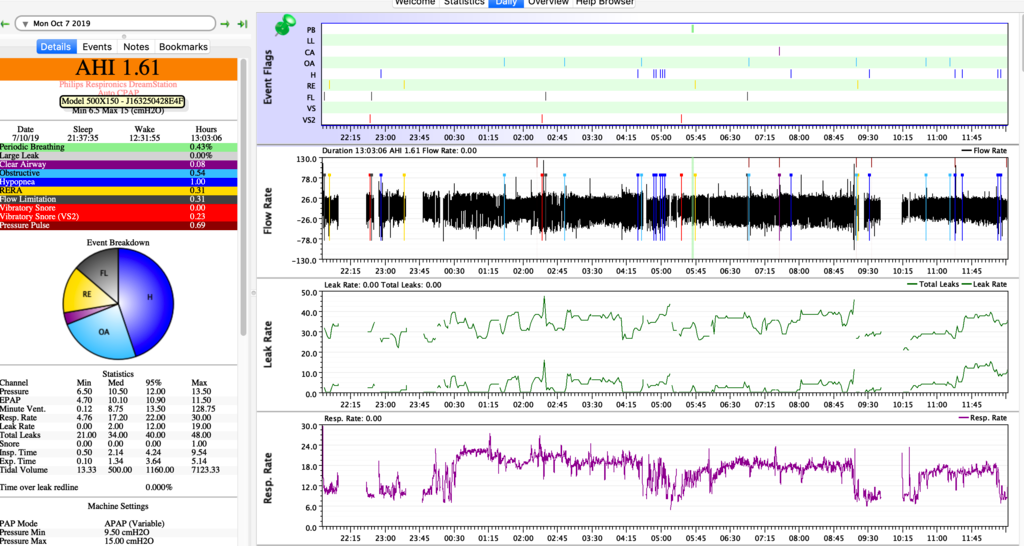
Ever since I have started CPAP my life has been going downhill. Within the first week, I started to experience extreme bloating, this led to me starting to react to foods and get brain fog really bad. The only way this could be controlled was through simply not eating. I quickly lost ALOT of weight due to being unable to sleep with any food in my stomach. I have played around with every pressure from 6 upto 15. Tried Aflex 1,2,3 and clfex 1,2,3 and epr 1,2,3. I have used a mandibular splint and all my issues dissapear but leave me with the usual sleep apnea oxygen-deprived state. But without any bloating. I simply cannot get the bloating to go away. Ive done every diet from Carnivore to paleo, vegan and intermittent fasting.
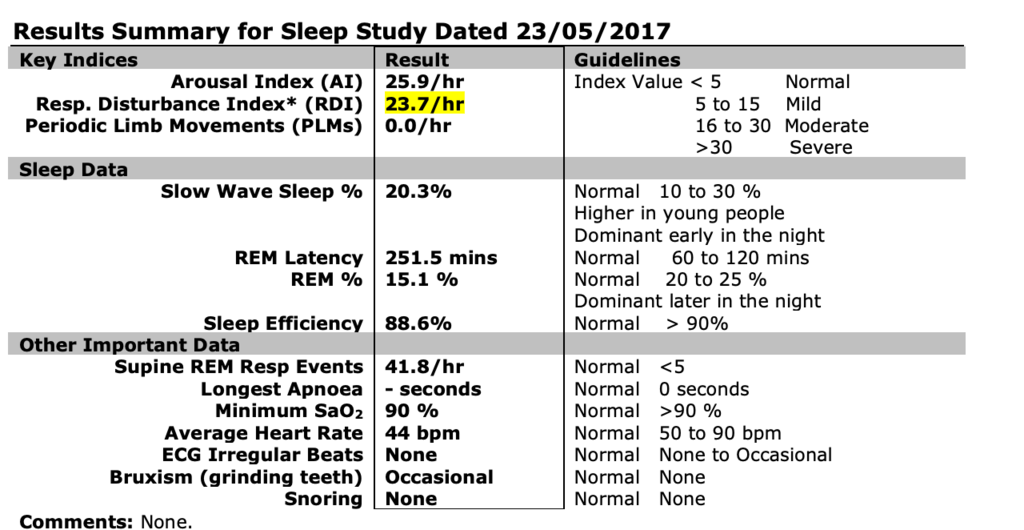
I want to understand why this keeps happening. My sleep apnea stems from a small jaw and law tongue. UARS? my airway feels extremely narrow and I even have issues breathing properly during the day. I don't know if this is from the cpap or not but I tend to breathe very shallow and rapidly and not belly breathe. I feel like the design of my airways force me to take rapid inhales in order for air to pass through my narrow airway, this in turn may lead to acid from the stomach to enter the upper oesophagus inflaming and narrowing my airway further. I'm unsure.
I have experimented by reducing the leake rate of my mask (phillips fitlife full face mask) by slightly covering a valve, to my surprise this led to a more unrestful sleep but my cognitive dulling and numbess reduced quite a bit. Perhaps I am blowing off to much co2? low co2 reduces cerebral circulation in the pre front cortex which is where all my issues lie. Its as if I do not have an executive functioning system. I feel brain dead and apathetic and do not want to do anything. Yet a night off the machine my goal oriented mind returns. I am so confused and do not know what to do. Cerebral vasoconstriction is the result of blowing off too much co2. Another symptom is that I cannot feel any mind altering substances such as coffee. Zero effect at all. It's as if nothing can pass my blood brain barrier due to the circulatory issues. Yet a night off and boom and i get mind back again!! Don't know what to make of this.
Ive already undergone radiofrequency ablation to reduce tongue and it didnt work at all - spent 8k. A mandibular device - 2k. And am now considering jaw surgery.
Am i intolerant to co2? causing me to breathe in such a way that gets rid of it? should try and become accustom to co2 with reduced breathing?? Ive had small success reducing my inhale and exhale by putting some tape on my nostrils. I feel like the issue stems from my breathing, which effects my stomach. Causing a negative feedback loop leading to cerebral vasoconstriction through hyperventilation.
If anyone has ANY idea or has heard of a similar issue please let me know.
------------------------------------
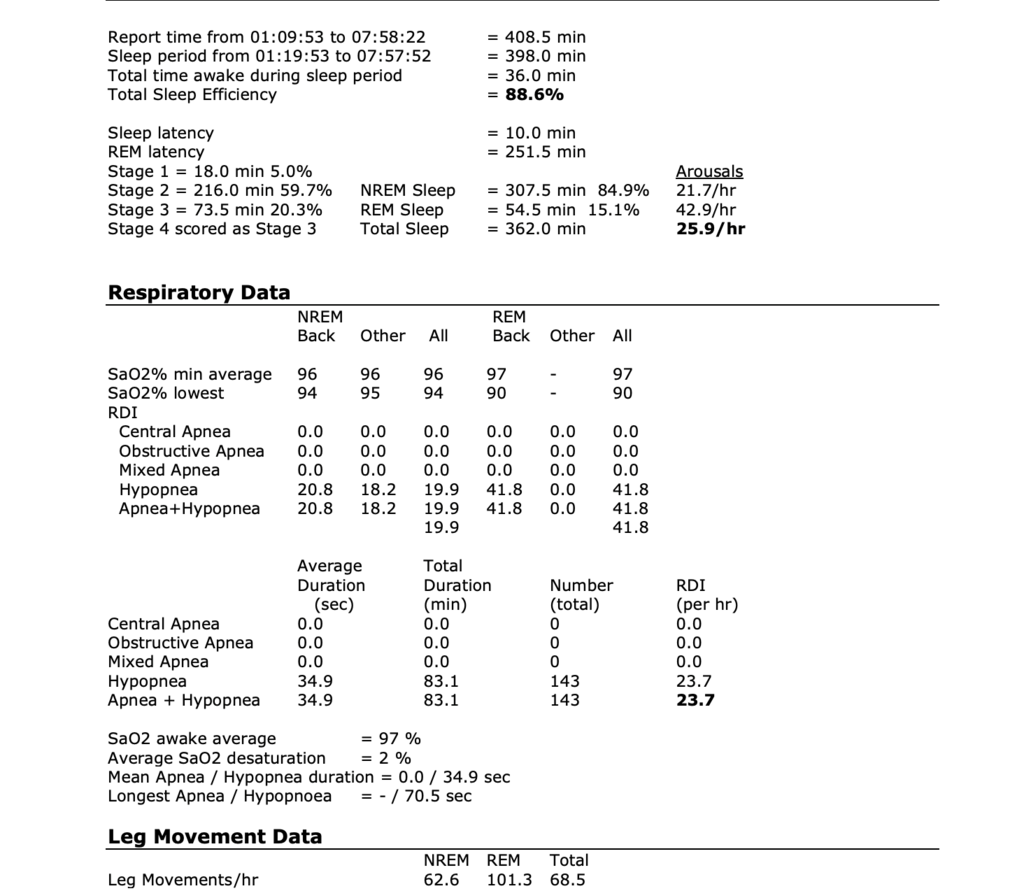
Sleepyhead data - Sleep study results - sleepyhead overview (+ oximetry data for 1 night)