Who else has primarily hypopneas? UARS?
Who else has primarily hypopneas? UARS?
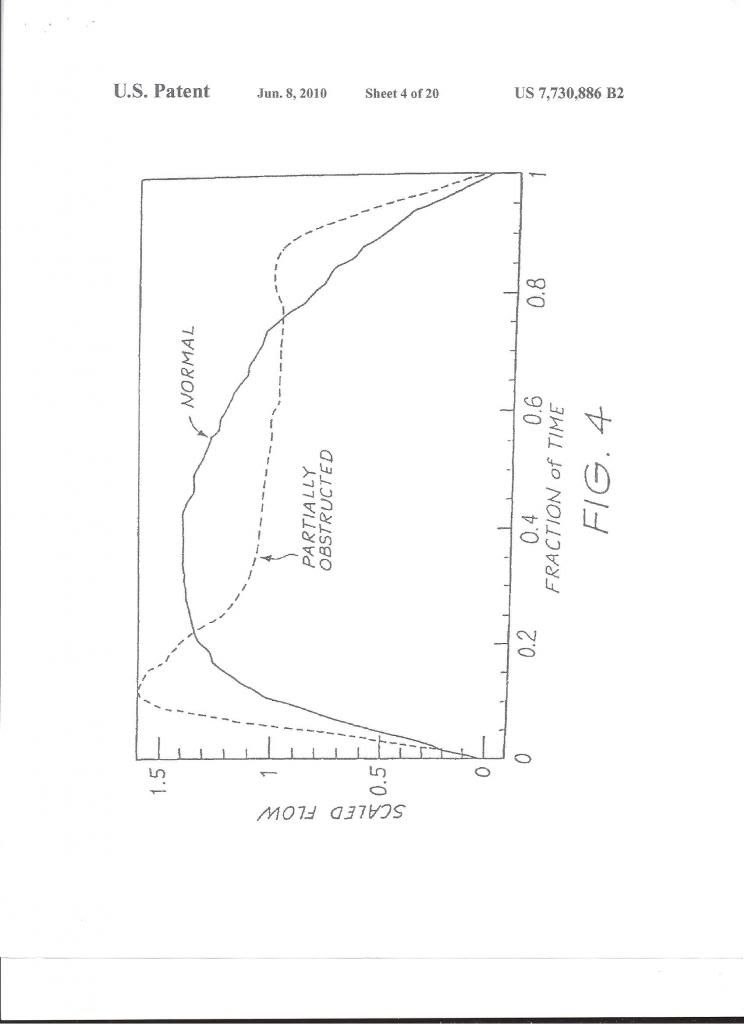
From discussions the past few days, I can't help but wonder whether my experience with OSA is substantially different than others around here. My apnea index is under 5 but my hypopnea index is about 50. I found this nice chart on a presentation showing the physiological effect of apneas, hypopneas, and UARS and couldn't help but notice that hypopneas look almost nothing like apneas.
Are hypopneas and apneas grouped together into one syndrome solely for historical reasons? If so, then would you all agree that there's really two distinct disorders here: apnea syndrome (central, obstructive, or mixed) and resistance syndrome (hypopneas or UARS)? I'm guessing the physiological impact is quite different. To me it seems that apneas cause acute tissue death via oxidative stress while resistance syndromes cause stress disorders, which could mean cell death via totally different means (autoimmune disorders, autonomic dysfunction, etc). Both are still systemic diseases of course and have similar causes.
Are hypopneas and apneas grouped together into one syndrome solely for historical reasons? If so, then would you all agree that there's really two distinct disorders here: apnea syndrome (central, obstructive, or mixed) and resistance syndrome (hypopneas or UARS)? I'm guessing the physiological impact is quite different. To me it seems that apneas cause acute tissue death via oxidative stress while resistance syndromes cause stress disorders, which could mean cell death via totally different means (autoimmune disorders, autonomic dysfunction, etc). Both are still systemic diseases of course and have similar causes.
Re: Who else has primarily hypopneas? UARS?
The hypopneas disturb your sleep causing you to arouse to resolve the issue. The big issue is insurance companies do not pay for PAP if you have hypopneas, which sucks because you feel horrible. Not sure about the grouping.
I've had problems since Nov 2011. My AHI is very similar to yours. First sleep study was a failure due to insomnia, but hypoxemia was diagnosed. Decided to try to lose some weight instead of taking the oxygen. Guess what, did lose about 10 lbs, but didn't help and fell back into my old routine. This spring my co-workers were ready to string me up due to irritability and inability to perform at my job. Found a family member's old cpap beast, cleaned it up and not he first night at around 7cm/H2O, I had what I consider the best sleep of my life. Had a second sleep study and had very mild apnea with mostly hypopneas and nocturnal hypoxemia. I cannot recall the numbers from the study. Sleep Dr. dx UARS and oxygen. You don't need CPAP, you need oxygen and ENT to fix your septum. Saw ENT. Had a septoplasty and did well for a few months, even returned the oxygen concentrator. Around September, I had a home study that showed my ahi had worsened since the last study despite the septoplasty and I was still hypoxemic. Started with Auto CPAP which I have been very compliant with, 4-15 CM now narrowed down to 6-10. I was still hypoxemic on the auto pap, so I had to get a concentrator to bleed in a couple of liters at night. My BMI is around 30, I feel like the dx was OHS and the UARS was not as big of an issue. Fortunately I did well with the septoplasty. It was four days of hell with the stents but once the were out, it was very worth it. Others have a horrible time with the procedure and regret it.
What every you do, get help. Do you have a recommendation for treatment?
At this point, I have accepted the need for cpap and the oxygen and just want to recover and enjoy my life.
I've had problems since Nov 2011. My AHI is very similar to yours. First sleep study was a failure due to insomnia, but hypoxemia was diagnosed. Decided to try to lose some weight instead of taking the oxygen. Guess what, did lose about 10 lbs, but didn't help and fell back into my old routine. This spring my co-workers were ready to string me up due to irritability and inability to perform at my job. Found a family member's old cpap beast, cleaned it up and not he first night at around 7cm/H2O, I had what I consider the best sleep of my life. Had a second sleep study and had very mild apnea with mostly hypopneas and nocturnal hypoxemia. I cannot recall the numbers from the study. Sleep Dr. dx UARS and oxygen. You don't need CPAP, you need oxygen and ENT to fix your septum. Saw ENT. Had a septoplasty and did well for a few months, even returned the oxygen concentrator. Around September, I had a home study that showed my ahi had worsened since the last study despite the septoplasty and I was still hypoxemic. Started with Auto CPAP which I have been very compliant with, 4-15 CM now narrowed down to 6-10. I was still hypoxemic on the auto pap, so I had to get a concentrator to bleed in a couple of liters at night. My BMI is around 30, I feel like the dx was OHS and the UARS was not as big of an issue. Fortunately I did well with the septoplasty. It was four days of hell with the stents but once the were out, it was very worth it. Others have a horrible time with the procedure and regret it.
What every you do, get help. Do you have a recommendation for treatment?
At this point, I have accepted the need for cpap and the oxygen and just want to recover and enjoy my life.
_________________
| Machine: PR System One REMStar 60 Series Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
Re: Who else has primarily hypopneas? UARS?
My sleep study showed mostly hypopneas and hypoxia. Wikipedia seems to indicate that UARS is separate from hypopneas. How was your UARS diagnosed?
_________________
| Mask: Pilairo Q Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
Re: Who else has primarily hypopneas? UARS?
I was "diagnosed" with mild OSA, probably so that insurance would cover xPAP (my insurance will not cover UARS). However, based on the results of the study and the way that it was run, I have UARS. I had no apneas, a few hypopneas and a large number of respiratory distress arousals. I also never got below 92% O2 sat and the doctor was surprised it got that low. I should also add that my sleep studies included Pes measurements, which is the gold standard for differentiating UARS from OSA.
If you read some of the papers that are available on the Internet, there seem to be two schools of thought. One says that UARS, Hypopneas, and OSA are a continuum of sleep disordered breathing of increasing severity. Even the original paper on UARS speculated that patients might eventually move from UARS on to OSA as they age and gain weight.
The other position is that they are two different syndromes with different patient populations. With OSA, the patient population tends to older, over weight males. There is even a guideline based on neck size. For UARS, the population is claimed to have more females, be younger, lower BMI and smaller neck and jaw size. As you indicated, UARS is also supposed to be associated more with autoimmune and autonomic disorders while OSA tends to be associated more with heart issues.
Personally, I tend to believe that they may both be right, but that I fall into the second position because the body type and associated conditions fit me to a tee (other than being young and female).
If you read some of the papers that are available on the Internet, there seem to be two schools of thought. One says that UARS, Hypopneas, and OSA are a continuum of sleep disordered breathing of increasing severity. Even the original paper on UARS speculated that patients might eventually move from UARS on to OSA as they age and gain weight.
The other position is that they are two different syndromes with different patient populations. With OSA, the patient population tends to older, over weight males. There is even a guideline based on neck size. For UARS, the population is claimed to have more females, be younger, lower BMI and smaller neck and jaw size. As you indicated, UARS is also supposed to be associated more with autoimmune and autonomic disorders while OSA tends to be associated more with heart issues.
Personally, I tend to believe that they may both be right, but that I fall into the second position because the body type and associated conditions fit me to a tee (other than being young and female).
_________________
| Mask: SleepWeaver Anew™ Full Face Mask with Headgear |
| Additional Comments: Pressure 9-12, Sleepyhead V9.3-0 |
Re: Who else has primarily hypopneas? UARS?
I am going to post the Chest article about URS that I posted here before in a new thread and it will include illustrations too and it will be a stand alone thread. It will be something that I and others could refer to.
Let me try it here again:
http://69.36.35.38/accp/pccsu/upper-air ... e?page=0,3
Let me try it here again:
http://69.36.35.38/accp/pccsu/upper-air ... e?page=0,3
_________________
| Humidifier | ||||
 | ||||
| Additional Comments: CareFusion chinstrap. Quite stiff and not smooth. Not for delicate faces. | ||||
Last edited by penuel on Tue Jan 14, 2014 3:15 pm, edited 4 times in total.
How to get around ResScan 3.12: http://montfordhouse.com/cpap/resscan_tutorial/
-
sawinglogz
- Posts: 400
- Joined: Mon Aug 27, 2012 12:53 pm
Re: Who else has primarily hypopneas? UARS?
Interesting question. I was AHI=18, all hypopneas, 108 events during the diagnostic study. That was enough to classify me as "moderate obstructive sleep apnea." Thank goodness, since I can't sleep without my ASV!
I'm not sure what a more nuanced diagnosis of UARS would accomplish, since in a brief skim of that article I didn't notice any treatments that I wouldn't also try for OSA?
I'm not sure what a more nuanced diagnosis of UARS would accomplish, since in a brief skim of that article I didn't notice any treatments that I wouldn't also try for OSA?
Re: Who else has primarily hypopneas? UARS?
When I had my titration study done with the Pes, the pressures measured clearly showed widely varying inhalation pressures until they reached 9cm, at which point my airway was apparently splinted open and the UARS conditions disappeared. A detailed examination of the shape of the inhalation flow curve might have shown the same changes, but that would have been subject to interpretation whereas the PeS graph was very clear.sawinglogz
I'm not sure what a more nuanced diagnosis of UARS would accomplish, since in a brief skim of that article I didn't notice any treatments that I wouldn't also try for OSA?
As for what this meant versus a standard OSA style result, when I first started with my aPAP the machine routinely had me at 7.5 or 8 cm because it was not sensitive enough to detect my RERAs, even though I had followed the manufacturer's recommended adjustment to the algorithm to make the hypopnea detection more senstive to RERAs. I now have it set so that it starts at my prescribed 9cm.
_________________
| Mask: SleepWeaver Anew™ Full Face Mask with Headgear |
| Additional Comments: Pressure 9-12, Sleepyhead V9.3-0 |
Re: Who else has primarily hypopneas? UARS?
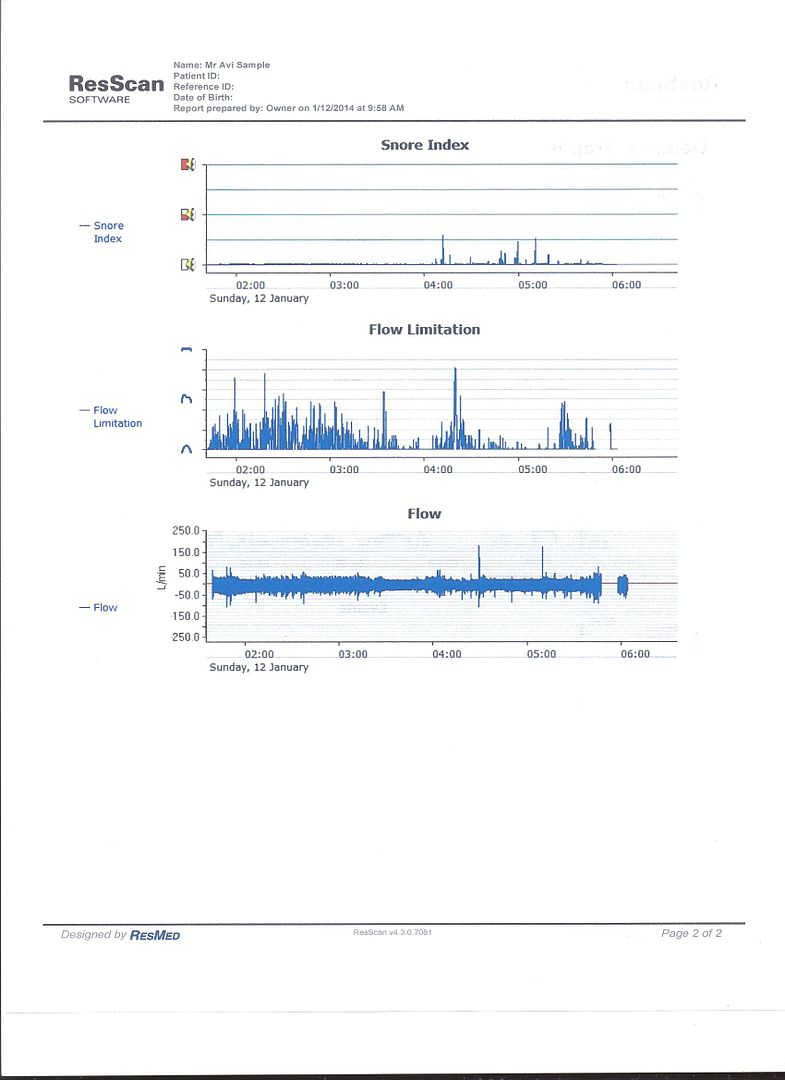
My S9 Autoset deals with UARS by checking the flatness of the respirations waves. It gathers the info in a moving window and if the out of flatness continuous then it raises the pressure somewhat, assuming that no central apnea (open airway) interferes:
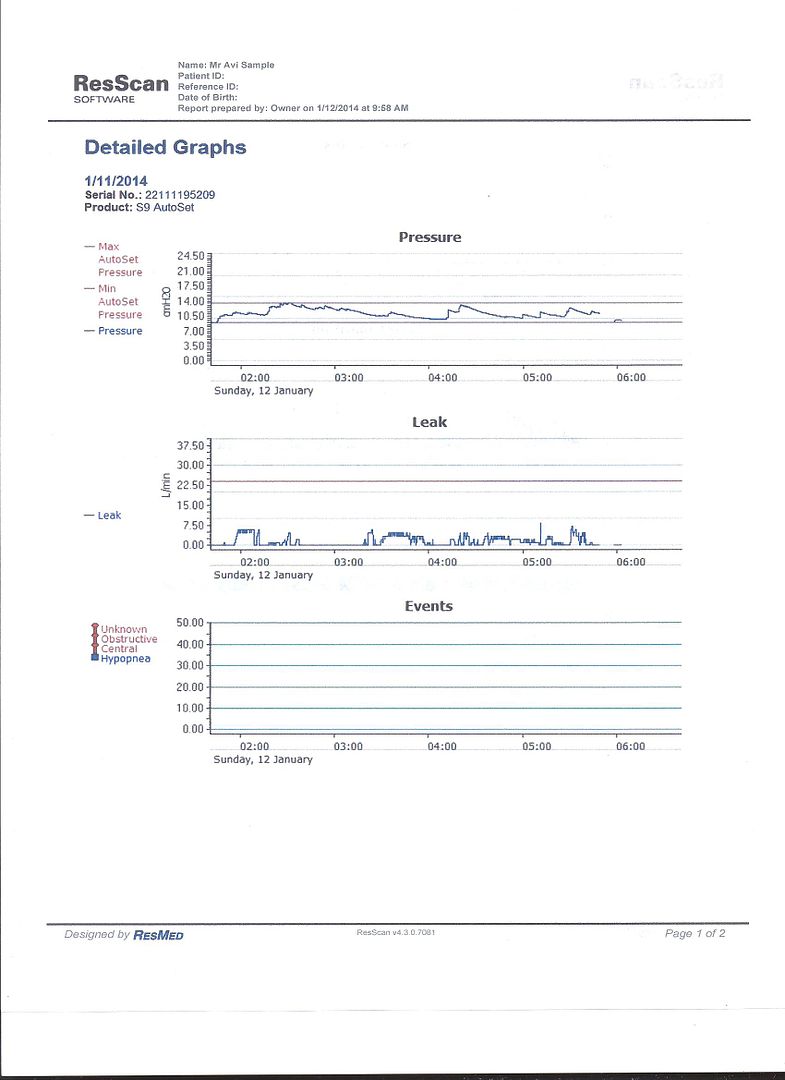
It does a pretty good job reducing the Flow Limitation (which includes the UARS. But not eliminates it completely):
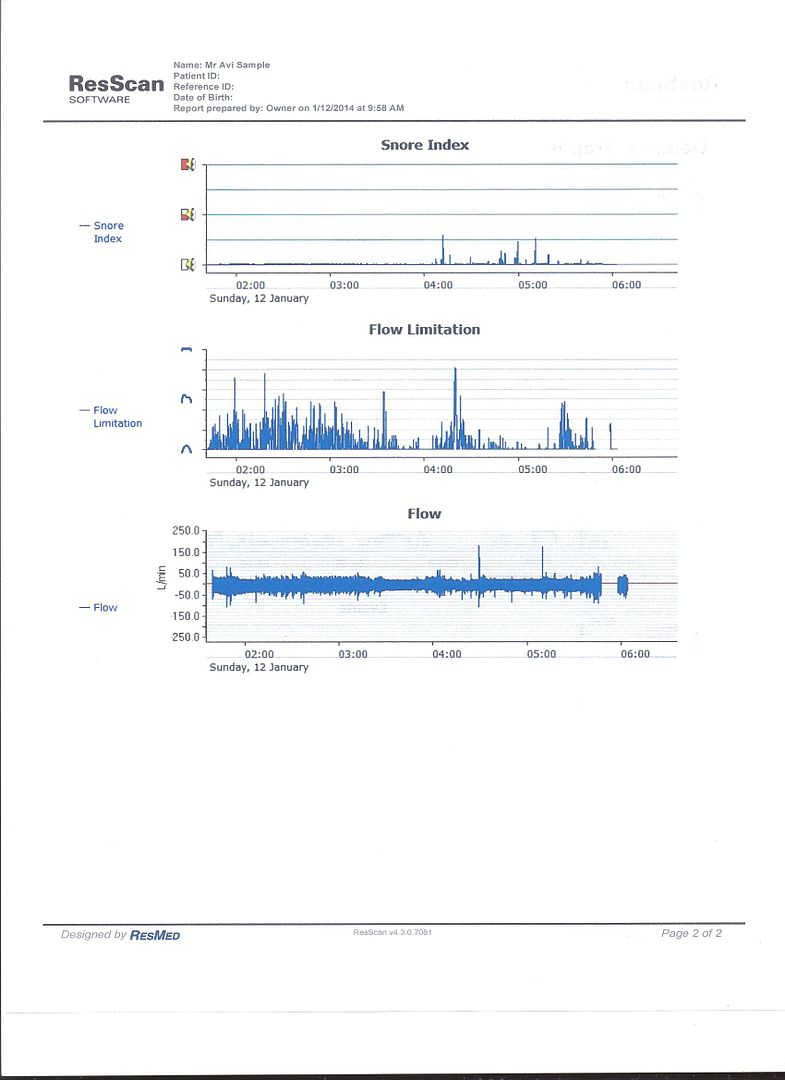
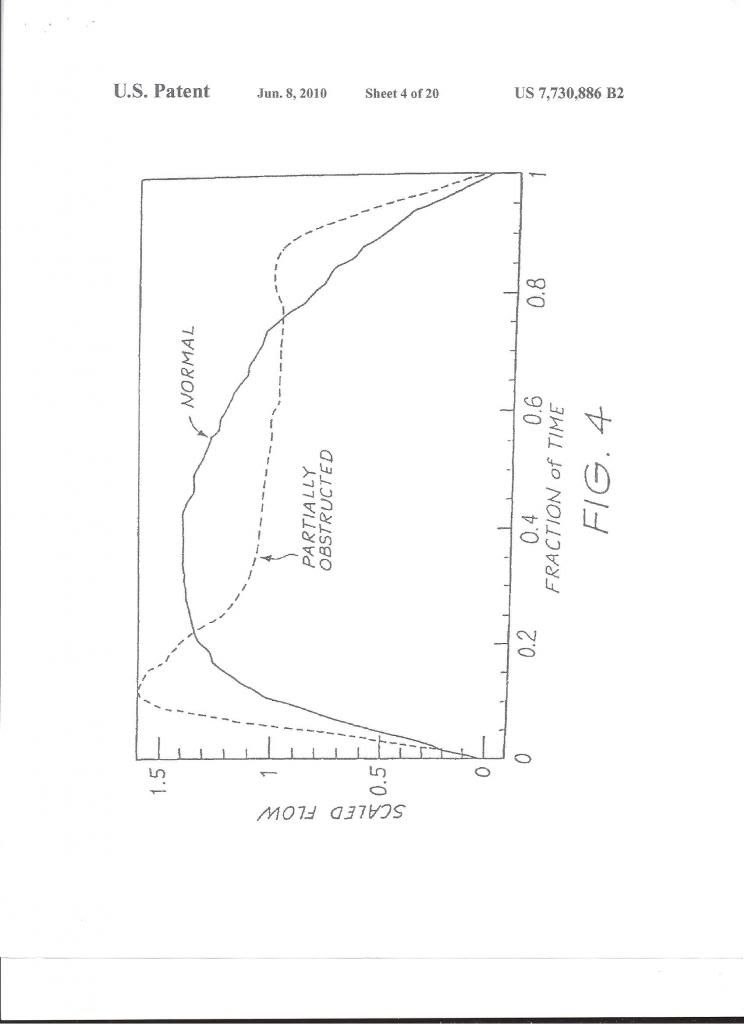
This is the way that Resmed's machines deal with the Shape Factor of the respiration waves' shapes. The machines have
a fix methodology to process the decisions if to raise pressure:
These are my Stats for the recent full year. It does not include Flow Limitations values:

It does a pretty good job reducing the Flow Limitation (which includes the UARS. But not eliminates it completely):
This is the way that Resmed's machines deal with the Shape Factor of the respiration waves' shapes. The machines have
a fix methodology to process the decisions if to raise pressure:
These are my Stats for the recent full year. It does not include Flow Limitations values:

_________________
| Humidifier | ||||
 | ||||
| Additional Comments: CareFusion chinstrap. Quite stiff and not smooth. Not for delicate faces. | ||||
How to get around ResScan 3.12: http://montfordhouse.com/cpap/resscan_tutorial/
Re: Who else has primarily hypopneas? UARS?
Reacts Philips algorithm also in FL?
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: APAP 7,8 - 20 EPR 3 No Ramp ResScan 5.1 SleepyHead 0.9.8.1 |
Everything I write I translate through Google Translate.
Hope you have patience with that, sometimes it can get a little crazy.
/Lazer1234
Hope you have patience with that, sometimes it can get a little crazy.
/Lazer1234
Re: Who else has primarily hypopneas? UARS?
Check this thread:newpapper wrote:My sleep study showed mostly hypopneas and hypoxia. Wikipedia seems to indicate that UARS is separate from hypopneas. How was your UARS diagnosed?
viewtopic.php?f=1&t=57791&st=0&sk=t&sd=a
_________________
| Humidifier | ||||
 | ||||
| Additional Comments: CareFusion chinstrap. Quite stiff and not smooth. Not for delicate faces. | ||||
How to get around ResScan 3.12: http://montfordhouse.com/cpap/resscan_tutorial/
Re: Who else has primarily hypopneas? UARS?
My PSG showed an AHI of 4.9, mostly hypopneas and central apneas (only 1 obstructive all night). I had more RERAs and a lot of spontaneous arousals -- the RDI was 12.1 and the total arousal index was 34.1. I wasn't tested specifically for UARS but that's what the reporting doctor speculated and I certainly seem to fit the profile. I have been using an S9 Autoset for one month and my AHI has jumped a lot -- nearly all centrals, and mostly apparently sleep onset -- the overall AHI is hovering around 10 but they come in bunches, with peaks going up to 40. I'm also waking up a lot and having a hard time going back to sleep. I'm less sleepy than when I started but still nothing like what I think would approach "normal."
I didn't know the Autoset could be set to detect RERAs, how would I do this? Would that likely help with the centrals? On the current settings the pressure is staying around 6, the highest it goes is about 10. This doesn't seem to be cutting it. I am concerned that the high number of centrals means I really need an ASV -- which would be out of pocket but would be worth it if I stopped being tired.
I didn't know the Autoset could be set to detect RERAs, how would I do this? Would that likely help with the centrals? On the current settings the pressure is staying around 6, the highest it goes is about 10. This doesn't seem to be cutting it. I am concerned that the high number of centrals means I really need an ASV -- which would be out of pocket but would be worth it if I stopped being tired.
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
Re: Who else has primarily hypopneas? UARS?
mimico, how do you know that you had more RERAs? The S9 machine reports Flow Limitation (FL) and not RERAs. But RERAs and UARS are included in the FL that the S9 reports. For FL you don't need an ASV but you may need it if you have Central Sleep Apnea Syndrome.
_________________
| Humidifier | ||||
 | ||||
| Additional Comments: CareFusion chinstrap. Quite stiff and not smooth. Not for delicate faces. | ||||
How to get around ResScan 3.12: http://montfordhouse.com/cpap/resscan_tutorial/
Re: Who else has primarily hypopneas? UARS?
Sorry, I should have specified. The PSG showed (with a total sleep time of 440.2 min):
11 Central apneas (index 1.5)
1 Obstructive apnea (index 0.1)
1 Mixed apnea (index 0.1)
23 hypopneas (index 3.1)
52 RERAS (index 7.1)
162 spontaneous arousals (index 17.1)
250 total arousals (index 34.1)
The indexes soared when I was on my back, to 47.1 AHI and 68.6 RDI, but I never sleep on my back (for obvious reasons)
Despite the single OSA, my sleep doctor (who is a pulmonologist and not certified in sleep med) and respiratory therapist are locked into a diagnosis of OSA, which is probably to my advantage since Kaiser is paying for them and the study, though not for the equipment. UARS barely seems to register for them. They are very nice and doing their best to be helpful but I have gotten so much more helpful information here (thank you, everyone!). I did talk to both the doc and the RT about the central apneas today, and we agreed to revisit that in a couple of weeks.
I have been downloading the data into both Sleepyhead and ResScan. In addition to the Central Apneas it shows a huge number of flow limitations -- presumably those are also RERAs? (no way to tell without EEG info). I am thinking I will try bumping the minimum pressure to 6 and then slowly raising it and seeing what that does. I tried it during a nap and found it easier to breathe and, short time that it was, had an AHI of 0.0. I have the EPR set to max (which is 3) and exhaling at 6 is a little effortful but not bad. Hopefully I can stay with relatively low pressures and not have to spring for a bilevel. As for the centrals, time will tell.
11 Central apneas (index 1.5)
1 Obstructive apnea (index 0.1)
1 Mixed apnea (index 0.1)
23 hypopneas (index 3.1)
52 RERAS (index 7.1)
162 spontaneous arousals (index 17.1)
250 total arousals (index 34.1)
The indexes soared when I was on my back, to 47.1 AHI and 68.6 RDI, but I never sleep on my back (for obvious reasons)
Despite the single OSA, my sleep doctor (who is a pulmonologist and not certified in sleep med) and respiratory therapist are locked into a diagnosis of OSA, which is probably to my advantage since Kaiser is paying for them and the study, though not for the equipment. UARS barely seems to register for them. They are very nice and doing their best to be helpful but I have gotten so much more helpful information here (thank you, everyone!). I did talk to both the doc and the RT about the central apneas today, and we agreed to revisit that in a couple of weeks.
I have been downloading the data into both Sleepyhead and ResScan. In addition to the Central Apneas it shows a huge number of flow limitations -- presumably those are also RERAs? (no way to tell without EEG info). I am thinking I will try bumping the minimum pressure to 6 and then slowly raising it and seeing what that does. I tried it during a nap and found it easier to breathe and, short time that it was, had an AHI of 0.0. I have the EPR set to max (which is 3) and exhaling at 6 is a little effortful but not bad. Hopefully I can stay with relatively low pressures and not have to spring for a bilevel. As for the centrals, time will tell.
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |












