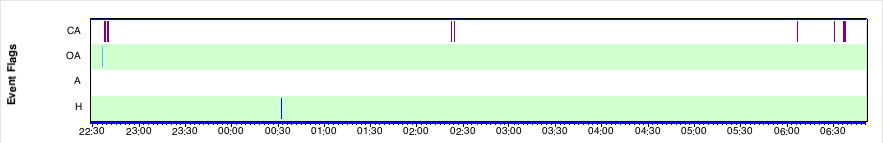
Oddprofessor wrote:Would you look at this?? It's a 9-minute segment from a last night. During the entire night I had 56 CA events, 4 Hypopnia, and 7 Obstructive Apneas. It looks like my breathing just gets shallower and shallower until it stops, then it starts and does the same thing, over and over. There are similar clusters later in the night. What is going on here?
Vicki
Have you ever heard of feedback? When you use a microphone sometimes the gain for the microphone channel gets so high that the energy from the speaker is picked up in the microphone. At first you will hear a tone. Often the tone will become louder. At a certain point it will turn into a screech because there is not enough “room” for the system to go any louder and so the system produces harmonics as well.
In a looped (e.g. speaker talks to microphone) system if gain becomes positive the system will go into oscillation (produces a tone). If gain becomes yet higher it will tend to produce square waves (the screech – tone with harmonics due to reaching the limits of the system).
Breathing is supposed to be a negative total gain servo controlled system. The output of the system is the effort you make to breath. The inputs to the system come from sensors in your body which look at blood gas levels. We have sensors which see deoxygenated red blood cells. We have sensors which know if the carbon dioxide levels are getting too high. There are several of them outside and inside the brain. If carbon dioxide levels in the blood reach a certain point breathing is increased. If the blood oxygen levels become too low breathing is increased. But the system is also sensitive to some outside forces as well.
For example an assault upon me in my past frayed my nerves. I ended up breathing too much during the day. Stress levels do play a part in how much we breath.
As well the pressure of CPAP plays a part. It makes it easier to breath in. It is like adding an assist to inhale. So the system has a little “plus” factor added to “breathing control system gain” when using CPAP.
Everything will be stable as long as the total system gain is below one. But if it goes above one, well, too much signal to breath is present – so the blood oxygen becomes over-oxygenated and the carbon dioxide levels become too low. With the gain too high the compensation of this causes a time of too little breathing – which sets up for the next time of over breathing. They call this periodic breathing. Breathing is not held at a level which keeps the gases balanced but is oscillating between to much and too little breathing.
If the gain becomes a bit higher the times of compensation of over breathing run into the floor. They become times of not breathing.
When we use a CPAP if we do not breath for a set time (I think mine is about seven seconds) the machine will send out a sensing pulse. If it hits an obstruction it will show the event as an obstructive apnea. If it does not hit an obstruction it will show it as a “Clear Airway” apnea or “CA”.
Take note of the fact that most of your clusters of “CA” events occur at times when the Flow Rate waveform becomes wider. This indicates that you are using more air during that time. You are moving more air at that time. Then a close up of the times shows that your system is seeking balance by the times of not breathing.
The use of CPAP is adding a new factor into your system. New reflexes need to form to deal with that. Reflexes form over time and many find that the problems you see now become less as they better learn how to use CPAP.
I think it would help to spend some quality time with the machine during the daytime. Some on the bed learning how to breath quietly (learning how to keep the extra gain from making you breath more). And some with distraction such as a book, music, radio, or light TV. I am suspicious that using the conscious mind and state help develop the new breathing reflexes faster.
Anything you can do to reduce stress is likely to help.
Exercise tends to “work out” the breathing systems and I find that it helps with nighttime breathing stability while using CPAP.
Dr. Stasha Gominak has noted that many areas of the brain which deal with breathing control are sensitive to D3 levels. I am finding it easier to breath eucapnically during the day and with greater stability during the night as my D3 levels rise. Those who are working with the D3 hormone (A.K.A. Vitamin D3) (e.g. Dr. Stasha Gominak, Michael F. Holick, Ph.D., M.D., Vitamin D Council) seem to be finding that the very low side of the “normal” range of 30-100 ng/L produces a range of symptoms including OSA, pain, and infection. All believe that a level lower than 50 ng/mL is not good and Dr. Stasha Gominak recommends 60-80 ng/mL for good health. I think you would be wise to have them checked.