My elderly mom is attempting to use a BiPAP machine to get relief from complex sleep apnea. She was diagnosed with sleep apnea about 3 months ago and has been using the machine every night during that period. She still feels very fatigued during the day and we're trying to determine if there is value for her in continuing treatment. Her sleep stats as compiled by Encore Basic have been underwhelming for the most part. When I politely brought that to the attention of her sleep doctor, her doctor opined that the data that Encore returns can be unreliable and that we'd be better off ignoring the stats. Has anyone else experienced a similier situation? I'm doing my best to keep our relationship with this doctor and sleep clinic respectful and polite but I'm not sure where the truth of the matter resides and if our best course forward is to be patient or to seek help elsewhere. I don't want to tussle with the doctor - I just want to help my mom get some relief from her symptoms. Thanks in advance for any thoughts you can share, annecedotal. philisophical or scientific. I'm including a more datailed discription below if you have to time to scan it -
---------------------------
My mom uses a Respironics BiPAPautoSV advanced unit. I have a card reader and Encore Basic (thanks Pugsy!). My mom is 87 and has a number of health issues, including congestive heart failure and multiple back surgeries and deal with stenosis, arthritis, and calcification issues. She takes a lot of medication including a low dosage of opioid pain medication. My mom’s AHI seems to vary significantly from night to night. It can be as high as 39 and as low as 14; the average seems to hover around 25. The ratio of obstructive apneas, centrals, and hypopneas also varies considerably from night to night. During a doctor consultation a couple weeks ago we told the doctor that we weren’t overwhelmed with the results of the treatment to date. My mom still feels really pooped all day and the numbers returned by EncoreBasic seem to indicate a significant amount of ‘event’s’ that might be contributing to her not getting restful sleep. The doctor recommended another sleep study (our third to date). My mom performed the sleep study and we returned to the doctor late last week so she (the doc) could explain the results of the study. Note* - during the study the BiPAP machince was at the same settings that my mom’s machine has been set to. The settings were not changed during the sleep study. The sleep study reported that my mom had no central or obstructive apneas during the night. It stated that she had 51 hypopneas during that night for an AHI of 8.3. This result was better than any mom has experienced sleeping at home, at least according to the values returned by Encore Basic. The doctor said that she thinks the results of the sleep study show that my mom’s treatment is “close to perfect, given her age and general health”. When I pointed out that my mom feels lousy and that her AHI as reported by Encore is considerably higher the doctor became brusque and advised to ignore the data from Encore Basic. Personally, I’d be thrilled to not monitor her stats using Encore if she was feeling better. As she’s not it seems to make sense to try to improve the situation. I’m not sure what to do at this point. For what it’s worth her AHI has been between 24 and 14 (as reported by Encore) in the week since our last consultation... and she's still really tired.
I’m grateful for any thoughts you might have – thanks!
Artimus60
Are Encore sleep statistics credible?
Are Encore sleep statistics credible?
Machine: REMStar BiPAP AutoSV Advanced
Humidifier: REMstar Heated Humidifier
Mask: Mirage Quattro Full Face w/ Headgear
Humidifier: REMstar Heated Humidifier
Mask: Mirage Quattro Full Face w/ Headgear
Re: Are Encore sleep statistics credible?
A little bit of possible pooh poohing off minor maybe unreliable rare event stuff shown on the report...I could live with.
To tell you to ignore all the stuff you are seeing on the Encore reports is irresponsible in my opinion.
The data is reliable up to the machines limitations and the main limitation is with the flagging of clear airway events since the machine doesn't know if we are awake or not....no way can we blame all the events that show up on your mom's reports on being awake or semi awake or sleep stage transition..not with her history of centrals in the non cpap sleep studies.
The obstructive events shown...you can count on those being reliable data.
Unless your mom never sleeps and is totally awake while wearing the mask...those obstructives are the real deal.
Personally, to me it sounds like the doctor doesn't know what else to try and has given up trying and working with you to improve things because let's face it...your mom's situation is difficult.
I would be looking for someone who was willing to work harder and not prone to give up with the going got rough.
To tell you to ignore all the stuff you are seeing on the Encore reports is irresponsible in my opinion.
The data is reliable up to the machines limitations and the main limitation is with the flagging of clear airway events since the machine doesn't know if we are awake or not....no way can we blame all the events that show up on your mom's reports on being awake or semi awake or sleep stage transition..not with her history of centrals in the non cpap sleep studies.
The obstructive events shown...you can count on those being reliable data.
Unless your mom never sleeps and is totally awake while wearing the mask...those obstructives are the real deal.
Personally, to me it sounds like the doctor doesn't know what else to try and has given up trying and working with you to improve things because let's face it...your mom's situation is difficult.
I would be looking for someone who was willing to work harder and not prone to give up with the going got rough.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
Re: Are Encore sleep statistics credible?
Artimus60,
This is something I wrote on a different forum in response to a general question about the accuracy of machine recorded data with some very minor editing to reflect your mother's situation:
Your mom's BiPAP Auto SV machine detects apneas and hypopneas by analyzing the airflow into/out of your lungs. It tracks each breath to establish a running "baseline" for your normal breathing pattern during the last five or ten minutes or so. Whenever the airflow drops by 50% from the running baseline for at least 10 seconds, the machine will flag a hypopnea. Whenever the airflow drops by 80% from the running baseline for at least 10 seconds the machine will score an apnea.
If the machine in your signature is correct, your mother is using a PR BiPAP Auto SV that is not part of the System One family. I don't know if the machine attempts to distinguish between central apneas and obstructive apneas the way the System One machines do. If I recall correctly, it does NOT distinguish between them. In other words, any 10+ second long period of little or no airflow will be flagged as an apena. The Auto SV part of the algorithm is designed to try end the undershoot/overshoot cycle that is involved in Cheyne-Stokes breathing and plays a significant role in severe central sleep apnea and complex apnea. (The undershoot/overshoot cycle is tied to the CO2 levels in the blood. JohnBFisher has written at length about this cycle and it's connections to central sleep apnea. Search through his posts to find out a good understanding of how that Auto SV algorithm is supposed to work. So I won't comment on how accurate the patient triggered breaths data is.
How accurate is a BiPAP's AHI? Well it's accurate enough for trending purposes. But it's not 100% on the spot accurate for any given night. To understand this, you need to know the following two definitions:
As others have noted, a CPAP/BiPAP machine cannot tell when you are asleep and when you are awake. Since the CPAP computes the AHI by simply dividing the number of detected events by the total time the machine was running for the night, that introduces two kinds of obvious errors as compared to an in lab PSG where the EEG is used to determine when you are asleep.
In addition to the two obvious kinds of errors discussed above, there are also algorithm errors. Sometimes the machine will miss what looks like an obvious event---perhaps because the machine thinks it's not quite 10 seconds long. Or perhaps the drop from the current baseline is not quite enough. Sometimes the machine will score an event and you'll look at the data and not see anything that even vaguely resembles an apnea/hypopnea. These errors pop up often enough that if you zoom in on your wave flow data every single night, you're sure to see a few of them each week, but you probably wont see them every night. (But I don't know whether your mom's machine actually records the wave flow or not since it's not a System One.) These random missed events and random extra events tend to cancel each other out in the long run. And so they don't tend to affect the overall trend of the AHI data over the course of several days or weeks.
And so when we consider the machine AHI data as trending data, it is considered accurate enough to be significant, even if any individual night might be off.
For example, if you have one night with an AHI that is up around 9, but your typical AHI is usually between 1.0 and 3.0, that one night is likely just an outlier: It may have been simply been a bad night for your OSA. Or it could be that the data for that night is particularly inaccurate---perhaps because you were very, very restless all night long. But that one night with an AHI of around 9 doesn't really indicate that there's something wrong with your overall therapy because the trend of data is that your machine AHI is consistently below 3.0, which clearly indicates that your real AHI is consistently well below the desired 5.0.
But on the other hand, if you are seeing machine AHI's that are consistently above a 5.0 night after night for several weeks, then there's a good chance that something is not yet "optimized" about your therapy---particularly if you continue to experience daytime sleep apnea symptoms. It could be that your pressure is set too low and too many events are still occurring. It could be that you are in the unlucky 10% of new CPAPers who wind up developing problems with pressure induced central apneas It could mean that your leaks are not under control and you are losing too much pressure for your therapy to be effective. In any case, an AHI that is consistently above 5.0 for a period of several weeks should be brought to your sleep doc's attention.
I'll write more that is directly tied to what you've written about your mom's case in the next post.
This is something I wrote on a different forum in response to a general question about the accuracy of machine recorded data with some very minor editing to reflect your mother's situation:
Your mom's BiPAP Auto SV machine detects apneas and hypopneas by analyzing the airflow into/out of your lungs. It tracks each breath to establish a running "baseline" for your normal breathing pattern during the last five or ten minutes or so. Whenever the airflow drops by 50% from the running baseline for at least 10 seconds, the machine will flag a hypopnea. Whenever the airflow drops by 80% from the running baseline for at least 10 seconds the machine will score an apnea.
If the machine in your signature is correct, your mother is using a PR BiPAP Auto SV that is not part of the System One family. I don't know if the machine attempts to distinguish between central apneas and obstructive apneas the way the System One machines do. If I recall correctly, it does NOT distinguish between them. In other words, any 10+ second long period of little or no airflow will be flagged as an apena. The Auto SV part of the algorithm is designed to try end the undershoot/overshoot cycle that is involved in Cheyne-Stokes breathing and plays a significant role in severe central sleep apnea and complex apnea. (The undershoot/overshoot cycle is tied to the CO2 levels in the blood. JohnBFisher has written at length about this cycle and it's connections to central sleep apnea. Search through his posts to find out a good understanding of how that Auto SV algorithm is supposed to work. So I won't comment on how accurate the patient triggered breaths data is.
How accurate is a BiPAP's AHI? Well it's accurate enough for trending purposes. But it's not 100% on the spot accurate for any given night. To understand this, you need to know the following two definitions:
- In-lab PSG AHI = (number of events scored while you are asleep)/(total time you are asleep) where "you are asleep" is detected by the EEG readings.
- CPAP machine AHI = (number of events recorded during the night)/(total time the machine was running during the night)
As others have noted, a CPAP/BiPAP machine cannot tell when you are asleep and when you are awake. Since the CPAP computes the AHI by simply dividing the number of detected events by the total time the machine was running for the night, that introduces two kinds of obvious errors as compared to an in lab PSG where the EEG is used to determine when you are asleep.
- False events are "apneas" and "hypopneas" that the machine scores when you are actually awake. On a PSG, any "event" that occurs during a time period when the EEG indicates that you are actually awake is NOT counted towards the AHI. The reason is simple: Sleep apnea is a breathing problem that occurs when you are asleep. The control of our sleep breathing is different than the control of our wake breathing. And our wakeful breathing is much less regular than our sleep breathing. We sigh. We hold our breath momentarily when concentrating on something as simple (or complex) as turning over in bed while managing a six foot hose attached to our nose. We consciously take several deep breaths in a row to relax ourselves and then breath much more shallowly for a few more breaths. And some of us have a bit of a tendency to not breathe for a bit when we're transitioning from Wake to Sleep as our body resets the control of breathing. On an in-lab PSG, none of these kinds of "events" count because we're awake when they start. But a CPAP doesn't know that and scores them anyway. The net result of these "false" events is to make the AHI increase a bit because there can be a few more events scored than should/would have been scored on a PSG. And so the numerator of the AHI fraction is higher than it should be, which makes the computed AHI go up.
- Inaccurate estimate of sleep time affects the denominator of the AHI fraction. The presumption by the CPAP makers is that your sleep time and the machine run time will be close enough to each other that the error introduced by using machine run time will be insignificant. And if you are one of those people who falls asleep within 5-15 minutes of going to be and doesn't spend much time awake during the night, that's actually a pretty valid assumption. But if you've got major insomnia and you're lying in bed with the mask on and the machine running for several hours each night, using machine run time instead of total sleep time to compute the AHI can increase the size of the denominator enough to reduce the AHI, perhaps significantly. (If two fractions have the same numerator, the fraction with the larger denominator will be the smaller of the two fractions---i.e. 29/8 is smaller than 29/6.)
In addition to the two obvious kinds of errors discussed above, there are also algorithm errors. Sometimes the machine will miss what looks like an obvious event---perhaps because the machine thinks it's not quite 10 seconds long. Or perhaps the drop from the current baseline is not quite enough. Sometimes the machine will score an event and you'll look at the data and not see anything that even vaguely resembles an apnea/hypopnea. These errors pop up often enough that if you zoom in on your wave flow data every single night, you're sure to see a few of them each week, but you probably wont see them every night. (But I don't know whether your mom's machine actually records the wave flow or not since it's not a System One.) These random missed events and random extra events tend to cancel each other out in the long run. And so they don't tend to affect the overall trend of the AHI data over the course of several days or weeks.
And so when we consider the machine AHI data as trending data, it is considered accurate enough to be significant, even if any individual night might be off.
For example, if you have one night with an AHI that is up around 9, but your typical AHI is usually between 1.0 and 3.0, that one night is likely just an outlier: It may have been simply been a bad night for your OSA. Or it could be that the data for that night is particularly inaccurate---perhaps because you were very, very restless all night long. But that one night with an AHI of around 9 doesn't really indicate that there's something wrong with your overall therapy because the trend of data is that your machine AHI is consistently below 3.0, which clearly indicates that your real AHI is consistently well below the desired 5.0.
But on the other hand, if you are seeing machine AHI's that are consistently above a 5.0 night after night for several weeks, then there's a good chance that something is not yet "optimized" about your therapy---particularly if you continue to experience daytime sleep apnea symptoms. It could be that your pressure is set too low and too many events are still occurring. It could be that you are in the unlucky 10% of new CPAPers who wind up developing problems with pressure induced central apneas It could mean that your leaks are not under control and you are losing too much pressure for your therapy to be effective. In any case, an AHI that is consistently above 5.0 for a period of several weeks should be brought to your sleep doc's attention.
I'll write more that is directly tied to what you've written about your mom's case in the next post.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: Are Encore sleep statistics credible?
Artimus60,
First I want to clarify which machine your mother is actually using.
You signature indicates that it is a REMStar BiPAP AutoSV Advanced, which looks like this:

But to the best of my knowledge that machine does NOT use PP to test the patency of the upper airway, and hence it does not try to distinguish between OAs and CAs. And yet you write that "The ratio of obstructive apneas, centrals, and hypopneas also varies considerably from night to night.", which seems to indicate that the machine your mother is using does distinguish between OAs and CAs. So is her machine actually a PR System One REMstar BiPAP Auto SV Advanced which looks like this:

As I said, I'm confused about which machine your mother is actually using since you talk about it recording centrals.
Now onto addressing some of your questions/concerns about your mom's data. You write:
The importance of how your mom feels during the day cannot be over estimated. Given that she is 87, the focus of any medical treatment should be on whether it can be made to improve the quality of her day to day life. Clearly, the BiPAP therapy is not yet making a positive difference. Whether it's time to throw in the towel and have her just abandon therapy is a question that you and she will need to weigh with or without meaningful input from her doctors. One question that I'd ask your mom is: Are you more tired and exhausted during the day with the BiPAP than you were before you started BiPAP? And weigh her answer against your own observations of her daily behavior---does she seem more tired, more fatigued, more fog brained now than she did during the last three months before she started therapy? Or is she simply feeling about the same degree of lousiness that she was feeling before she started BiPAP?
These are important questions because your mom has a number of chronic medical conditions that can lead to daytime fatigue. If the BiPAP is not making her feel any worse than she did when she first started it, then there's a good chance that it's doing her body some good, but not enough good to overcome the fatigue from all the other medical problems. (And if her therapy were genuinely optimized, it might make a positive difference in how she feels.) But if she's feeling substantially worse now that she's on BiPAP, then it is reasonable to start asking whether she's better off dealing with the symptoms and health risks from untreated OSA or whether she's better off dealing with the additional fatigue being induced by the BiPAP therapy.
Of course---it would help if you could get her therapy truly optimized. And right now, I think you are still asking for ideas on what might be done to optimize her therapy since her numbers still do not look good. You write:
So my main suggestion is: Switch sleep docs if possible. Or at least get a second opinion from a different sleep doc. Fight to have the entire night's data (not just the summary stuff) for all three sleep tests sent to the new doc's office and ask for the tests to be rescored from scratch.
As for other, more mundane and "do-it-yourself" tips, I think you need to try to tease out some additional information from your Mom.
First set of questions for teasing apart whether you should believe the Encore data is valid enough for trending purposes: How restless is your mom during the night on a typical night when she's sleeping in her own bed? Keep in mind that she may say that she falls asleep quickly and never remembers waking up, but that may not be the case. What was the sleep efficiency on each of her three sleep studies??? Has there been any documented improvement in her sleep architecture in the lab?
Second set of questions: For many of us, our sleep varies a lot from night to night. Ask your mom whether she believes the sleep she got in the lab on her last test is representative of the sleep she's getting at home night after night after night. If she thinks that her sleep was not normal for her that night, it probably wasn't normal. It could be that she had a particularly restless night and spent much less time asleep than normal and hence the events that she typically at home simply didn't show up because she was AWAKE for a substantial portion of the night. It could be that she sleep more soundly (for whatever reason) and that any problems with sleep onset instability didn't manifest themselves because she wasn't dozing for large chunks of the night. So if she thinks that her sleep that night was not comparable to the sleep she gets at home every night, it's important to figure out how her sleep was different that night. She'll probably need some careful and thoughtful questions from you to help her remember the details.
These first two sets of questions are important because fragmented sleep and dozing---ie moving back and forth between WAKE and Stage 1/2 SLEEP for long periods during the night do not provide restorative sleep and dozing in particular can badly mess with the machine scored data---particularly if your mom has some sleep onset instability in her breathing. Her BiPAP will dutifully record each and every one of these incidents as either a CA, an H, or even an OA. The person who scores her PSG may well say to themselves while scoring her sleep test: That's a WAKE epoch, so we'll ignore that event over and over and over. Hence the truth could be that her machine is over scoring events, but the lab tech may be underestimating the importance of the sleep onset instability and underscoring some of her events---particularly sleep onset centrals that are routinely discounted as "normal" in most folks, but which can cause a great deal of trouble for a small minority of folks. See some of JohnBFisher's posts about this phenomenon.
Third set of questions: Did your mother experience significant O2 desats on her diagnostic test? Did she experience O2 desats with the scored events on either of the titration tests? If your mom tends to desat with her apneas, then it may well be worth investing in a recording oximeter to see if she's having roughly the same number of O2 desats as Encore indicates she's having events. That kind of data may be critical in figuring out just how bad the apnea remains even with treatment.
Next, given the long list of other issues your mother is dealing with, there are apt to be many other sources of fragmented sleep. And it could be that mostly eliminating the respiratory related arousals has not resulted in real improvement in her overall sleep simply because the other things continue to seriously fragment her sleep. So it's important to find out whether each medication she's on can adversely affect her sleep and how it might adversely affect her sleep. You may be able to use the internet to do some of this research yourself. Or ask the each of the docs who have prescribed medication for her about how that particular medication can affect sleep.
Finally, have Mom's vitamin levels been checked? Has a recent thyroid test been done? In other words, work with Mom's other doc's as well as a sleep doc on tackling what to do about other, non-sleep related causes of the daytime fatigue.
First I want to clarify which machine your mother is actually using.
You signature indicates that it is a REMStar BiPAP AutoSV Advanced, which looks like this:

But to the best of my knowledge that machine does NOT use PP to test the patency of the upper airway, and hence it does not try to distinguish between OAs and CAs. And yet you write that "The ratio of obstructive apneas, centrals, and hypopneas also varies considerably from night to night.", which seems to indicate that the machine your mother is using does distinguish between OAs and CAs. So is her machine actually a PR System One REMstar BiPAP Auto SV Advanced which looks like this:

As I said, I'm confused about which machine your mother is actually using since you talk about it recording centrals.
Now onto addressing some of your questions/concerns about your mom's data. You write:
andArtimus60 wrote:My elderly mom is attempting to use a BiPAP machine to get relief from complex sleep apnea. She was diagnosed with sleep apnea about 3 months ago and has been using the machine every night during that period. She still feels very fatigued during the day and we're trying to determine if there is value for her in continuing treatment.
I wish I could say I was surprised about the doc's attitude. But, alas, I am not.When I pointed out that my mom feels lousy and that her AHI as reported by Encore is considerably higher the doctor became brusque and advised to ignore the data from Encore Basic. Personally, I’d be thrilled to not monitor her stats using Encore if she was feeling better. As she’s not it seems to make sense to try to improve the situation.
The importance of how your mom feels during the day cannot be over estimated. Given that she is 87, the focus of any medical treatment should be on whether it can be made to improve the quality of her day to day life. Clearly, the BiPAP therapy is not yet making a positive difference. Whether it's time to throw in the towel and have her just abandon therapy is a question that you and she will need to weigh with or without meaningful input from her doctors. One question that I'd ask your mom is: Are you more tired and exhausted during the day with the BiPAP than you were before you started BiPAP? And weigh her answer against your own observations of her daily behavior---does she seem more tired, more fatigued, more fog brained now than she did during the last three months before she started therapy? Or is she simply feeling about the same degree of lousiness that she was feeling before she started BiPAP?
These are important questions because your mom has a number of chronic medical conditions that can lead to daytime fatigue. If the BiPAP is not making her feel any worse than she did when she first started it, then there's a good chance that it's doing her body some good, but not enough good to overcome the fatigue from all the other medical problems. (And if her therapy were genuinely optimized, it might make a positive difference in how she feels.) But if she's feeling substantially worse now that she's on BiPAP, then it is reasonable to start asking whether she's better off dealing with the symptoms and health risks from untreated OSA or whether she's better off dealing with the additional fatigue being induced by the BiPAP therapy.
Of course---it would help if you could get her therapy truly optimized. And right now, I think you are still asking for ideas on what might be done to optimize her therapy since her numbers still do not look good. You write:
andHer sleep stats as compiled by Encore Basic have been underwhelming for the most part.
So Encore Basic is showing nightly AHI's in the 14-39 range with a varying composition of OAs and CAs. The sleep study shows no apneas at all and a HI of 8.3. And of course, the gorilla in the room is the fact that Mom does NOT feel any better since starting treatment. And the doc doesn't seem to get it that Mom is not feeling any better.My mom’s AHI seems to vary significantly from night to night. It can be as high as 39 and as low as 14; the average seems to hover around 25. The ratio of obstructive apneas, centrals, and hypopneas also varies considerably from night to night. During a doctor consultation a couple weeks ago we told the doctor that we weren’t overwhelmed with the results of the treatment to date. My mom still feels really pooped all day and the numbers returned by EncoreBasic seem to indicate a significant amount of ‘event’s’ that might be contributing to her not getting restful sleep. The doctor recommended another sleep study (our third to date). My mom performed the sleep study and we returned to the doctor late last week so she (the doc) could explain the results of the study. Note* - during the study the BiPAP machince was at the same settings that my mom’s machine has been set to. The settings were not changed during the sleep study. The sleep study reported that my mom had no central or obstructive apneas during the night. It stated that she had 51 hypopneas during that night for an AHI of 8.3. This result was better than any mom has experienced sleeping at home, at least according to the values returned by Encore Basic. The doctor said that she thinks the results of the sleep study show that my mom’s treatment is “close to perfect, given her age and general health”.
So my main suggestion is: Switch sleep docs if possible. Or at least get a second opinion from a different sleep doc. Fight to have the entire night's data (not just the summary stuff) for all three sleep tests sent to the new doc's office and ask for the tests to be rescored from scratch.
As for other, more mundane and "do-it-yourself" tips, I think you need to try to tease out some additional information from your Mom.
First set of questions for teasing apart whether you should believe the Encore data is valid enough for trending purposes: How restless is your mom during the night on a typical night when she's sleeping in her own bed? Keep in mind that she may say that she falls asleep quickly and never remembers waking up, but that may not be the case. What was the sleep efficiency on each of her three sleep studies??? Has there been any documented improvement in her sleep architecture in the lab?
Second set of questions: For many of us, our sleep varies a lot from night to night. Ask your mom whether she believes the sleep she got in the lab on her last test is representative of the sleep she's getting at home night after night after night. If she thinks that her sleep was not normal for her that night, it probably wasn't normal. It could be that she had a particularly restless night and spent much less time asleep than normal and hence the events that she typically at home simply didn't show up because she was AWAKE for a substantial portion of the night. It could be that she sleep more soundly (for whatever reason) and that any problems with sleep onset instability didn't manifest themselves because she wasn't dozing for large chunks of the night. So if she thinks that her sleep that night was not comparable to the sleep she gets at home every night, it's important to figure out how her sleep was different that night. She'll probably need some careful and thoughtful questions from you to help her remember the details.
These first two sets of questions are important because fragmented sleep and dozing---ie moving back and forth between WAKE and Stage 1/2 SLEEP for long periods during the night do not provide restorative sleep and dozing in particular can badly mess with the machine scored data---particularly if your mom has some sleep onset instability in her breathing. Her BiPAP will dutifully record each and every one of these incidents as either a CA, an H, or even an OA. The person who scores her PSG may well say to themselves while scoring her sleep test: That's a WAKE epoch, so we'll ignore that event over and over and over. Hence the truth could be that her machine is over scoring events, but the lab tech may be underestimating the importance of the sleep onset instability and underscoring some of her events---particularly sleep onset centrals that are routinely discounted as "normal" in most folks, but which can cause a great deal of trouble for a small minority of folks. See some of JohnBFisher's posts about this phenomenon.
Third set of questions: Did your mother experience significant O2 desats on her diagnostic test? Did she experience O2 desats with the scored events on either of the titration tests? If your mom tends to desat with her apneas, then it may well be worth investing in a recording oximeter to see if she's having roughly the same number of O2 desats as Encore indicates she's having events. That kind of data may be critical in figuring out just how bad the apnea remains even with treatment.
Next, given the long list of other issues your mother is dealing with, there are apt to be many other sources of fragmented sleep. And it could be that mostly eliminating the respiratory related arousals has not resulted in real improvement in her overall sleep simply because the other things continue to seriously fragment her sleep. So it's important to find out whether each medication she's on can adversely affect her sleep and how it might adversely affect her sleep. You may be able to use the internet to do some of this research yourself. Or ask the each of the docs who have prescribed medication for her about how that particular medication can affect sleep.
Finally, have Mom's vitamin levels been checked? Has a recent thyroid test been done? In other words, work with Mom's other doc's as well as a sleep doc on tackling what to do about other, non-sleep related causes of the daytime fatigue.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: Are Encore sleep statistics credible?
Pugsy and Robysue,
Thank you for the information and the opinions. I’ll try to provide a little more information:
The device my mom is using is the REMStar BiPAP AutoSV Advanced <the first of the two photos in your reply>, (i.e. not the PR system 1 version). I assumed (quite possible incorrectly) that it differentiated between central and obstructive events because the EncoreBasic program breaks them out as such when you run a report. For what it’s worth, my mom seems to go right to sleep in the evening when she goes to bed. She gets up once or twice to urinate. In the sleep study that I referenced (her most recent study) her sleep efficiently rate was listed as 96.6%. Even though her fatigue remains high she hasn’t struggled much to get used to the machine/mask, etc. She’s had some issues with the bridge of her nose getting a bit red and raw but the mask (or struggling with air pressure) doesn’t keep her up at night for the most part. I wish I could detect a trend in AHI movement but it comes up and down seemingly at without a discernible pattern. It will drop down around 14 for a couple nights, bounce up to the mid 20’s, or go all the way up to approaching 40. Her combined central and obstructive apneas (at least as Encore reports them) will go down 5’ish and her hypopneas will jump up to 25. I guess I was expecting the comfort that seeing some sort of data trend but it’s all over the map. I concur that he fractured sleep could be in part caused by her medication or her other health issues – it sure is a bugger trying to make sense out of it when they’re all tangled up together. My gut tells me that it would be foolish to hang all of her fatigue and fogginess on sleep apnea but I think it’s contributing. I think I’m going to look into getting a second opinion on her sleep disorder. I’d like to do it without slashing and burning our relationship with her current doctor. I know my mom’s ‘case’ is a particularly challenging one and I don’t think her current doctor is fundamentally flawed but I’m wouldn’t exactly describe her as ‘dogged’. Her advice to ignore the data the Encore provides gave me an uneasy feeling. If my mom felt better I’d feel differently but it still feels like her sleep apnea is not being treated.
Thanks again,
Artimus60
Thank you for the information and the opinions. I’ll try to provide a little more information:
The device my mom is using is the REMStar BiPAP AutoSV Advanced <the first of the two photos in your reply>, (i.e. not the PR system 1 version). I assumed (quite possible incorrectly) that it differentiated between central and obstructive events because the EncoreBasic program breaks them out as such when you run a report. For what it’s worth, my mom seems to go right to sleep in the evening when she goes to bed. She gets up once or twice to urinate. In the sleep study that I referenced (her most recent study) her sleep efficiently rate was listed as 96.6%. Even though her fatigue remains high she hasn’t struggled much to get used to the machine/mask, etc. She’s had some issues with the bridge of her nose getting a bit red and raw but the mask (or struggling with air pressure) doesn’t keep her up at night for the most part. I wish I could detect a trend in AHI movement but it comes up and down seemingly at without a discernible pattern. It will drop down around 14 for a couple nights, bounce up to the mid 20’s, or go all the way up to approaching 40. Her combined central and obstructive apneas (at least as Encore reports them) will go down 5’ish and her hypopneas will jump up to 25. I guess I was expecting the comfort that seeing some sort of data trend but it’s all over the map. I concur that he fractured sleep could be in part caused by her medication or her other health issues – it sure is a bugger trying to make sense out of it when they’re all tangled up together. My gut tells me that it would be foolish to hang all of her fatigue and fogginess on sleep apnea but I think it’s contributing. I think I’m going to look into getting a second opinion on her sleep disorder. I’d like to do it without slashing and burning our relationship with her current doctor. I know my mom’s ‘case’ is a particularly challenging one and I don’t think her current doctor is fundamentally flawed but I’m wouldn’t exactly describe her as ‘dogged’. Her advice to ignore the data the Encore provides gave me an uneasy feeling. If my mom felt better I’d feel differently but it still feels like her sleep apnea is not being treated.
Thanks again,
Artimus60
Machine: REMStar BiPAP AutoSV Advanced
Humidifier: REMstar Heated Humidifier
Mask: Mirage Quattro Full Face w/ Headgear
Humidifier: REMstar Heated Humidifier
Mask: Mirage Quattro Full Face w/ Headgear
Re: Are Encore sleep statistics credible?
Those particular ASV machines do report centrals and thus the Encore software reports that you see are indicative of what the machine is reporting. Encore doesn't make up what isn't there. They do flag centrals. How they determine them....if I ever read...I have forgotten.Artimus60 wrote: I assumed (quite possible incorrectly) that it differentiated between central and obstructive events because the EncoreBasic program breaks them out as such when you run a report.
And he had to buy a DT3500 Infineer card to get the reports. His mom is for sure using the machine shown the his profile.
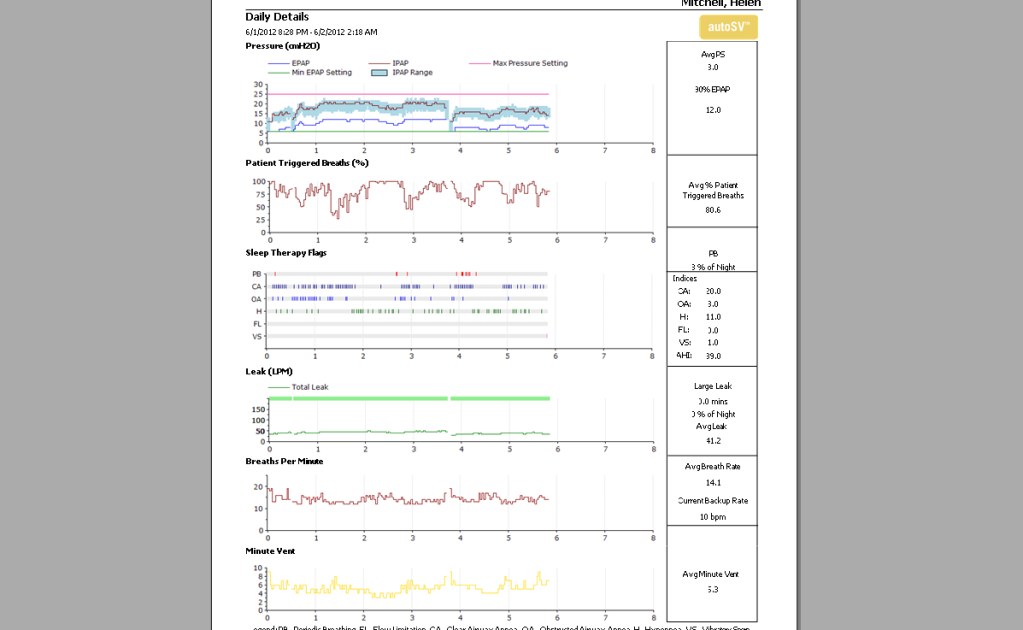
Anyone wondering what is going on..here is an old report. It is really hard to explain away all of those centrals especially with the history of documented centrals in original sleep studies. We might could explain away some...but not this many.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
Re: Are Encore sleep statistics credible?
Unfortunately, the standard medical practices in this country are set up to benefit the medical community, not just the patient. The medical mafia is a closed community like the lawyers, bankers, government, oil companies, and big business in general. Even the responsible members of the community tend to believe in the value of what they're doing. The system wants to do what's profitable and good for the system, and peer pressure tends to steer the independent thinkers back into the company way of thinking.
There are a number of bad reasons why doctors tend to ignore CPAP machine data.
1)The most important reason is profit. A PSG (in lab sleep test) can net the system lots of dollars. Heaven forbid someone uses data obtained cheaply from the CPAP machine, and you end up doing fewer PSGs.
2) You have to look at data and actually think to properly utilize CPAP machine data. The system wants them to ring the register and get on to the next patient. They like to pretend everything is cut and dried.
3) You have to do some study (not much) to know how to do a quick check on CPAP data enough to make some use of it. You could then spot a lot of problems, figure out you need to do more investigation, or figure out things are about right. It's not much work, but there is pressure to ring the register quickly.
4) There is a subculture of "sleep specialists" who want referrals. They don't want your average GP doctor to look at CPAP data and handle it himself. They'll try to make it seem as mysterious as possible and scare the GPs away from looking at the very useful data collected by the machine.
5) A PSG will give you a lot better data than the data recorded by a CPAP machine, so a lot of doctors ignore CPAP data. Unfortunately, you don't get a PSG very often, and you can get very useful data from the CPAP any time you want it. It's like ignoring a heart patient's blood pressure and heart rate because a nuclear stress test gives you better data.
6) Because of the way insurance works, it's more profitable to sell CPAP machines that don't collect any therapy data than ones that collect a lot of data. The system rationalizes selling the more profitable machines by pretending that the data collected is not valuable.
7) If the patient looks at his own data, he may figure out things on his own. It's more profitable to pretend that only the complicated specialized data is valuable.
8) Hypochondriacs are a problem for doctors. If they pretend that the data available to the patient is useless, dealing with hypochondriacs is easier.
9) Meddlesome parents or loved ones often interfere with treatment and waste the doctor's time. The meddlers are probably wrong more often than they are right. It's easier to assume the meddlers are always wrong and not bother to listen.
10) Patients themselves often read something wrong on the internet, or argue about their therapy when the doctor is right and the patient is wrong. They may even choose some less effective treatment because they have the wrong idea about something. Some patients are really bad that way. I suspect most apnea patients denied they had sleep problems before they had a test. It's easier to assume the doctor is always right.
Any doctor managing a CPAP patient should at least look at the data collected by the machine and realize it gives him some hints whether the treatment is working well. If something doesn't look right, he should investigate. Just because it's not the ultimate high tech expensive definitive diagnostic tool doesn't mean he should ignore it.
While it's important to monitor how the patient feels, remember that many people with really bad apnea deny they have any breathing problems during sleep at all before they get a sleep test. The patient's perception is sometimes not as good as objective data from a PSG or a CPAP machine.
To get back to the original question, the data collected by the CPAP machine is valuable diagnostic information. There's a good chance it will detect problems that need to be handled. Yes, sometimes the machine doesn't give you the definitive answer, but it gives you additional potentially valuable data to analyze. In many ways, it's a lot more valuable data than the data from a PSG that was in a strange environment, and was taken some time ago, sometimes years ago.
There are a number of bad reasons why doctors tend to ignore CPAP machine data.
1)The most important reason is profit. A PSG (in lab sleep test) can net the system lots of dollars. Heaven forbid someone uses data obtained cheaply from the CPAP machine, and you end up doing fewer PSGs.
2) You have to look at data and actually think to properly utilize CPAP machine data. The system wants them to ring the register and get on to the next patient. They like to pretend everything is cut and dried.
3) You have to do some study (not much) to know how to do a quick check on CPAP data enough to make some use of it. You could then spot a lot of problems, figure out you need to do more investigation, or figure out things are about right. It's not much work, but there is pressure to ring the register quickly.
4) There is a subculture of "sleep specialists" who want referrals. They don't want your average GP doctor to look at CPAP data and handle it himself. They'll try to make it seem as mysterious as possible and scare the GPs away from looking at the very useful data collected by the machine.
5) A PSG will give you a lot better data than the data recorded by a CPAP machine, so a lot of doctors ignore CPAP data. Unfortunately, you don't get a PSG very often, and you can get very useful data from the CPAP any time you want it. It's like ignoring a heart patient's blood pressure and heart rate because a nuclear stress test gives you better data.
6) Because of the way insurance works, it's more profitable to sell CPAP machines that don't collect any therapy data than ones that collect a lot of data. The system rationalizes selling the more profitable machines by pretending that the data collected is not valuable.
7) If the patient looks at his own data, he may figure out things on his own. It's more profitable to pretend that only the complicated specialized data is valuable.
8) Hypochondriacs are a problem for doctors. If they pretend that the data available to the patient is useless, dealing with hypochondriacs is easier.
9) Meddlesome parents or loved ones often interfere with treatment and waste the doctor's time. The meddlers are probably wrong more often than they are right. It's easier to assume the meddlers are always wrong and not bother to listen.
10) Patients themselves often read something wrong on the internet, or argue about their therapy when the doctor is right and the patient is wrong. They may even choose some less effective treatment because they have the wrong idea about something. Some patients are really bad that way. I suspect most apnea patients denied they had sleep problems before they had a test. It's easier to assume the doctor is always right.
Any doctor managing a CPAP patient should at least look at the data collected by the machine and realize it gives him some hints whether the treatment is working well. If something doesn't look right, he should investigate. Just because it's not the ultimate high tech expensive definitive diagnostic tool doesn't mean he should ignore it.
While it's important to monitor how the patient feels, remember that many people with really bad apnea deny they have any breathing problems during sleep at all before they get a sleep test. The patient's perception is sometimes not as good as objective data from a PSG or a CPAP machine.
To get back to the original question, the data collected by the CPAP machine is valuable diagnostic information. There's a good chance it will detect problems that need to be handled. Yes, sometimes the machine doesn't give you the definitive answer, but it gives you additional potentially valuable data to analyze. In many ways, it's a lot more valuable data than the data from a PSG that was in a strange environment, and was taken some time ago, sometimes years ago.
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Also SleepyHead, PRS1 Auto, Respironics Auto M series, Legacy Auto, and Legacy Plus |
Please enter your equipment in your profile so we can help you.
Click here for information on the most common alternative to CPAP.
If it's midnight and a DME tells you it's dark outside, go and check for yourself.
Useful Links.
Click here for information on the most common alternative to CPAP.
If it's midnight and a DME tells you it's dark outside, go and check for yourself.
Useful Links.
- chunkyfrog
- Posts: 34545
- Joined: Mon Jul 12, 2010 5:10 pm
- Location: Nowhere special--this year in particular.
Re: Are Encore sleep statistics credible?
An old explanation of quantum physics (probably over-simplified)
compared the value of a few samples of very accurate data with many samples of less accurate data;
and found them to be of similar usefulness.
There might be a correlation here, but hard to substantiate.
Heck, I believe it.
compared the value of a few samples of very accurate data with many samples of less accurate data;
and found them to be of similar usefulness.
There might be a correlation here, but hard to substantiate.
Heck, I believe it.
_________________
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Airsense 10 Autoset for Her |











