deltadave wrote:Sleep disturbance masquerading as SDB.
Repeated wakefulness during sleep can theoretically contribute to unstable central breathing/ventilation. You're wondering if JIMCHI might experience circadian cycles of nighttime wakefulness (impaired sleep drive)? Theoretically those could manifest as cyclic HI oscillations over many days as circadian sleep-drive waxes and wanes...deltadave wrote:My thought is that the respiratory events might be circadian in nature (hence, need about a month of detailed reports)(BTW, can you upload the first 3 pages of the detailed report?).
Here's my own relevant sleep/wake/sleep example resulting in frank central apneas: viewtopic/p563159/Collection-of-Oddball ... ml#p552606
JIMCHI, post the results whenever you'd like.JIMCHI wrote: I'm going to give this a try and will report results. ...post the results every day or just fill in the whole grid afterwards and then report ?
JIMCHI wrote: Also had an issue when exhaling that it felt like there was little resistance- annoying and kept me from getting to sleep right away.
BiFlex strives to minimize the "feel" of exhale resistance. And when EPAP is low, the "feel" of exhale resistance is going to seem very low. If setting EPAP min too low bothers you, then I'd suggest skipping all EPAP min =4 trials. That would leave a 2 x 3 exploratory grid instead. If residual HI is still high after experimenting with that remaining 2 x 3 grid, you could always add another exploratory column for EPAP min = 10 (at those same three PS min values)---and pending doctor approval.JIMCHI wrote: Do you have any thoughts about that problem I reported from last night-- that when I exhaled it seemed like there was a little resistance for maybe a second or two and then it just went to a full uninhibited exhale-- disturbing when you are trying to get to sleep and maybe, subconsciously, when you are sleeping. What variable affected that?
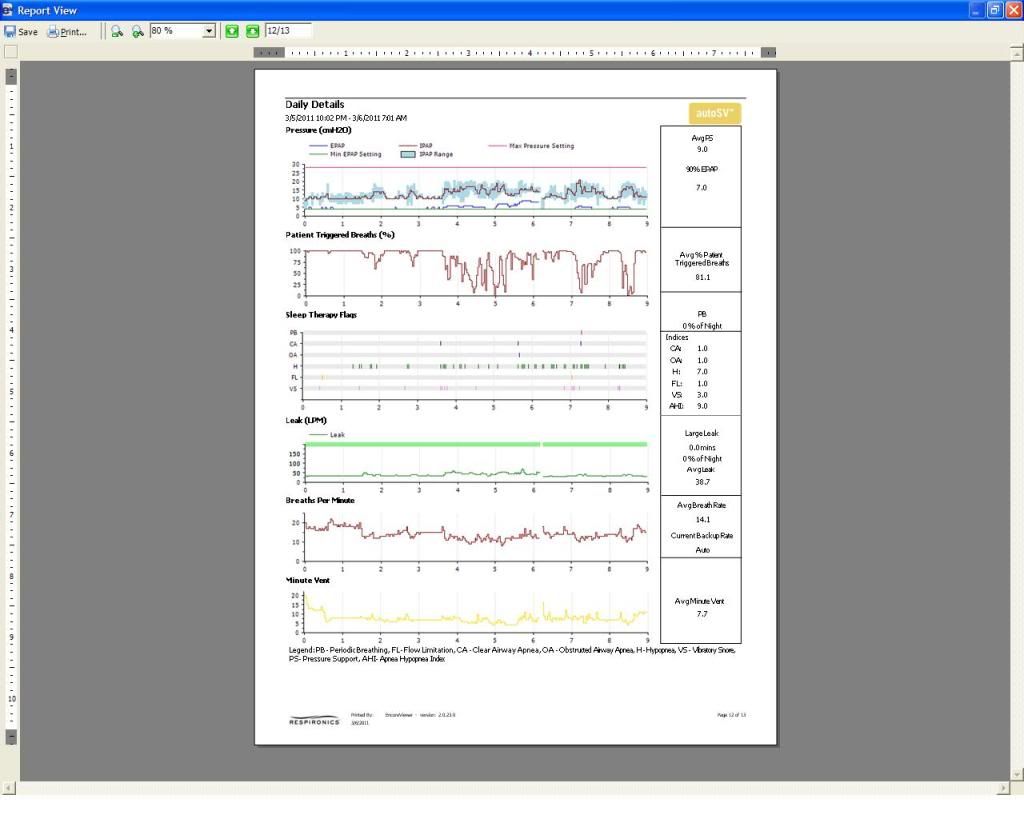
It's very difficult to see any details on those reports. But I can see residual HI is still up there. Hoping sleep is okay.JIMCHI wrote:Here's a link to an album with the 4 pages of the Encore Reports plus last night's data.
http://www.stanford.edu/~dement/epworth.htmldeltadave wrote: For daytime functioning, all the EPAP 4.0s will be 14, the 6.0s will be 11, and the 8.0s will be normal (<10).
JIMCHI, deltadave predicts that your experimental changes in daytime functioning (Epworth) will correlate to your changes in EPAP min. Lacking significant AHI variation, that prediction offers yet another implied assumption that your lower EPAP pressures can leave too many outstanding RERAs preventing restorative sleep:
http://www.google.com/search?q=rera+aro ... 1fdd569703