Help Interpreting CPAP Data
Re: Help Interpreting CPAP Data
I take two AD's, one, twice a day. I stopped taking the afternoon one for several days but that had no effect on my CPAP sleep experience. I haven't tried decaf for sometime. That's a good suggestion; I'll give it a try or just give up coffee, a least for now. Last night was another bad night. The leak reading was way high: Leak: 1.22L/s, AHI: 14.6, AI: 0.6, HI: 14.0. I'm seeing my sleep doctor this afternoon, and I'm hoping he can give me some solutions. Did I say I tried taping my mouth? It worked the first night but not last night.
Re: Help Interpreting CPAP Data
Dogbone, how bad were your limb movements in the titration report? It should tell you how many of the movements resulted in arousal. If you do have a severe problem, all the restless sleep could make you more prone to leaks than one who lies still most of the night.
Did your doc mention checking your ferritin level? Seems a lot of RLS sufferers have ferritin levels near the lower range of normal. For those with RLS, it is recommended their level be kept in the upper half of the normal range. I don't know how many actually see improvement with getting their ferritin level up, but I do know one forum member gets transfused periodically as hers will not increase with iron supplements. She says her movements improve after transfusion.
Another thing you may want to look at is if any meds you are on are known to cause problems with RLS. Seems I remember reading on here that some antidepressants being a problem. Hopefully someone else can speak to that. My sleep doc did not recommend benedryl for me due not only to possibly causing difficulty sustaining sleep, but because some experience worsening RLS symptoms with it. I'm wondering if treating your OSA and resolving the limb movements might change your need for some of the meds.
Seems to me a systematic approach will be most helpful to you because if you do too many things at once you won't be sure which really helped you. Here's how I see it...
...keep working on optimizing your cpap treatment
...talk to pharmacist or doc about your meds and any correlation with RLS and act accordingly
...check ferritin level and treat if lower than about 60
...decide if Mirapex is still needed
If necessary, you could use the Mirapex while working on the ferritin level, but I would be concerned about adding Mirapex to a mix of meds if it may be fighting a side effect of another med. If you choose to take the Mirapex, you could use it as a temporary tool to assess if controlling the limb movements gives you the sleep you need and if achieving that reduces your need for any of the other meds. Yes, there are some scary possible side effects listed for Mirapex. And I'm a witness that they not only can but do happen, as I experienced several on the list. However, the side effects of long term fractured sleep aren't desirable either. Just based on my experience, if you take it, start out at a low dose and stay there a few weeks before increasing. At every level of dosing, remain there a few weeks. Sometimes it can take a while to see the benefits. While some side effects are about getting used to it, some can be related to dosage, so keep it at the lowest effective dose. Be aware of the side effects so you can repsond to them if they appear. You can always go off the med, but MUST WEAN OFF.
Best wishes as you move forward.
Kathy
Did your doc mention checking your ferritin level? Seems a lot of RLS sufferers have ferritin levels near the lower range of normal. For those with RLS, it is recommended their level be kept in the upper half of the normal range. I don't know how many actually see improvement with getting their ferritin level up, but I do know one forum member gets transfused periodically as hers will not increase with iron supplements. She says her movements improve after transfusion.
Another thing you may want to look at is if any meds you are on are known to cause problems with RLS. Seems I remember reading on here that some antidepressants being a problem. Hopefully someone else can speak to that. My sleep doc did not recommend benedryl for me due not only to possibly causing difficulty sustaining sleep, but because some experience worsening RLS symptoms with it. I'm wondering if treating your OSA and resolving the limb movements might change your need for some of the meds.
Seems to me a systematic approach will be most helpful to you because if you do too many things at once you won't be sure which really helped you. Here's how I see it...
...keep working on optimizing your cpap treatment
...talk to pharmacist or doc about your meds and any correlation with RLS and act accordingly
...check ferritin level and treat if lower than about 60
...decide if Mirapex is still needed
If necessary, you could use the Mirapex while working on the ferritin level, but I would be concerned about adding Mirapex to a mix of meds if it may be fighting a side effect of another med. If you choose to take the Mirapex, you could use it as a temporary tool to assess if controlling the limb movements gives you the sleep you need and if achieving that reduces your need for any of the other meds. Yes, there are some scary possible side effects listed for Mirapex. And I'm a witness that they not only can but do happen, as I experienced several on the list. However, the side effects of long term fractured sleep aren't desirable either. Just based on my experience, if you take it, start out at a low dose and stay there a few weeks before increasing. At every level of dosing, remain there a few weeks. Sometimes it can take a while to see the benefits. While some side effects are about getting used to it, some can be related to dosage, so keep it at the lowest effective dose. Be aware of the side effects so you can repsond to them if they appear. You can always go off the med, but MUST WEAN OFF.
Best wishes as you move forward.
Kathy
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
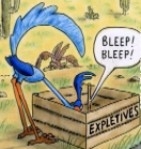
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: Help Interpreting CPAP Data
Dogbone, try the Hybrid, it might help with the leak problem. It's has the comfort of pillows with the security of not losing therapy air. Plus, it comes with 3 sizes of oral cushions, 3 sizes of pillows that can be set at 2 heights making getting a good fit fairly easy. Good luck with tackling each obstacle to restful sleep one at a time. Remember, the keywords patience and persistence.
ResMed S9 range 9.8-17, RespCare Hybrid FFM
Never, never, never, never say never.
Never, never, never, never say never.
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: Help Interpreting CPAP Data
Check Ferritin and Iron and TIBC and Transferrin Saturation and Transferrin, not just Ferritin.
Check Folate.
Antidepressants can exacerbate PLMs (I don't know about RLS). Most can affect sleep quality and sleep architecture (many suppress REM).
Check Folate.
Antidepressants can exacerbate PLMs (I don't know about RLS). Most can affect sleep quality and sleep architecture (many suppress REM).
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
Re: Help Interpreting CPAP Data
Big break thru for me. I slept the night through except for getting up twice for bathroom visits. I took one Benedryl generic capsule an hour before going to bed. The sleep doc lowered the pressure on my CPAP from 12 to 8. He told me to not tape my mouth and to not be concered about mouth breathing. The CPAP takes that into account, he said. I used the Mirage mask (goes over my nose but no pillows).
My reading this morning:
Leak .64L/s
AHI 10.6
AI 1.1
HI 9.5
The smart start is off; Leak arlert is off; FPA is off. I'm wondering if any of these should be on and if so, how do I turn them on.
In response to questions about my sleep study results (don't have the second study).
Periodic movements: 166; Index 33.8
Periodic w/arousal: 19
ferritin level: the doc said nothing about that. What is it?
I asked about continuing the Mirapex. He was not emphatic about continuing. I ask about taking magnesium for RSL, and he said it would help along with calcium and something else which I didn't write down. I think I'll stop the Mirapex and see what happens. I don't want to take it because of cost, though the Doc said there is a generic form.
The bottom line is that I'm progressing with your help.
My reading this morning:
Leak .64L/s
AHI 10.6
AI 1.1
HI 9.5
The smart start is off; Leak arlert is off; FPA is off. I'm wondering if any of these should be on and if so, how do I turn them on.
In response to questions about my sleep study results (don't have the second study).
Periodic movements: 166; Index 33.8
Periodic w/arousal: 19
ferritin level: the doc said nothing about that. What is it?
I asked about continuing the Mirapex. He was not emphatic about continuing. I ask about taking magnesium for RSL, and he said it would help along with calcium and something else which I didn't write down. I think I'll stop the Mirapex and see what happens. I don't want to take it because of cost, though the Doc said there is a generic form.
The bottom line is that I'm progressing with your help.
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: Help Interpreting CPAP Data
Dogbone, Ferritin is one of the blood tests run to assess for iron deficiency. The problem is that most doctors only run ferritin and not the other iron tests that I mentioned. You can be iron deficient and it won't show up on the ferritin, but will show up on one of the others. Most doctors don't know this and will only run ferritin.
When you tell your doctor you want them all run, tell them some kook on an internet forum told you to do this. (Good luck with that ) This kook told her son's doctor to run them all, and he humored her. Ferritin was normal but one of the iron tests came back abnormal. Doctor then supplemented iron.
If you are iron deficient, which I'm guessing you won't, you need to find out why. A grown man should not be deficient in iron without a good explanation.
Congrats on the better night.
When you tell your doctor you want them all run, tell them some kook on an internet forum told you to do this. (Good luck with that ) This kook told her son's doctor to run them all, and he humored her. Ferritin was normal but one of the iron tests came back abnormal. Doctor then supplemented iron.
If you are iron deficient, which I'm guessing you won't, you need to find out why. A grown man should not be deficient in iron without a good explanation.
Congrats on the better night.
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
- BleepingBeauty
- Posts: 2454
- Joined: Thu Apr 02, 2009 5:30 pm
- Location: Aridzona ;-)
Re: Help Interpreting CPAP Data
Your sleep doctor sounds about as knowledgeable as mine was.dogbone wrote:Big break thru for me. I slept the night through except for getting up twice for bathroom visits. I took one Benedryl generic capsule an hour before going to bed. The sleep doc lowered the pressure on my CPAP from 12 to 8. He told me to not tape my mouth and to not be concered about mouth breathing. The CPAP takes that into account, he said. I used the Mirage mask (goes over my nose but no pillows).
My reading this morning:
Leak .64L/s
AHI 10.6
AI 1.1
HI 9.5
If you're wearing a nasal mask and mouth-breathing, you're NOT getting the therapy the machine is supposed to be delivering. Either get yourself a FFM or keep taping your mouth shut with your nasal mask. Large leaks prevent us from getting effective therapy, so you have to fix that before you worry about other things.
Veni, vidi, Velcro. I came, I saw, I stuck around.
Dx 11/07: AHI 107, central apnea, Cheyne Stokes respiration, moderate-severe O2 desats. (Simple OSA would be too easy. )
)
PR S1 ASV 950, DreamWear mask, F&P 150 humidifier, O2 @ 2L.
Dx 11/07: AHI 107, central apnea, Cheyne Stokes respiration, moderate-severe O2 desats. (Simple OSA would be too easy.
PR S1 ASV 950, DreamWear mask, F&P 150 humidifier, O2 @ 2L.
Re: Help Interpreting CPAP Data
Thanks for the advice. I'm going to keep taping my mouth until I can get a FFMEither get yourself a FFM or keep taping your mouth shut with your nasal mask. Large leaks prevent us from getting effective therapy, so you have to fix that before you worry about other things.