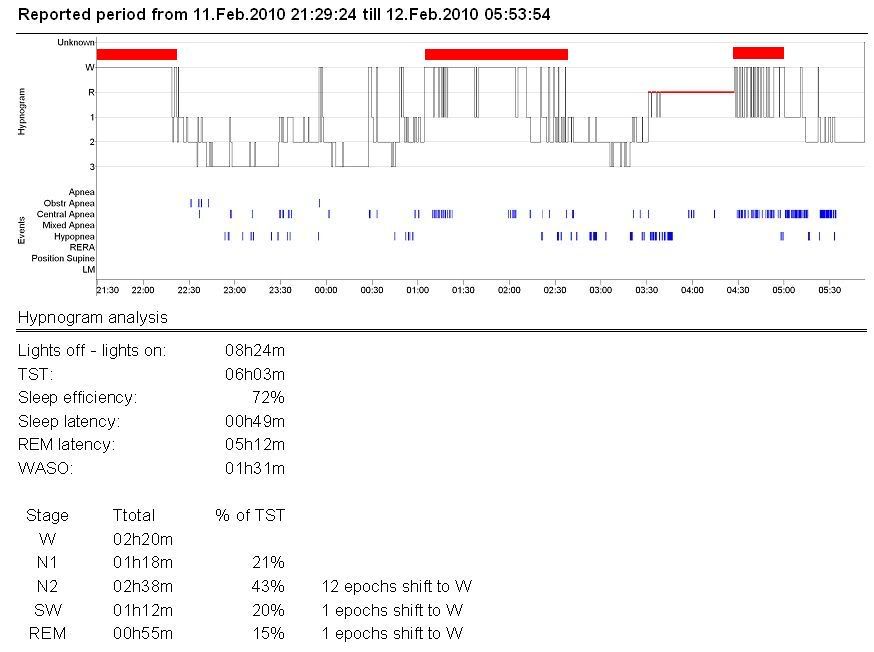
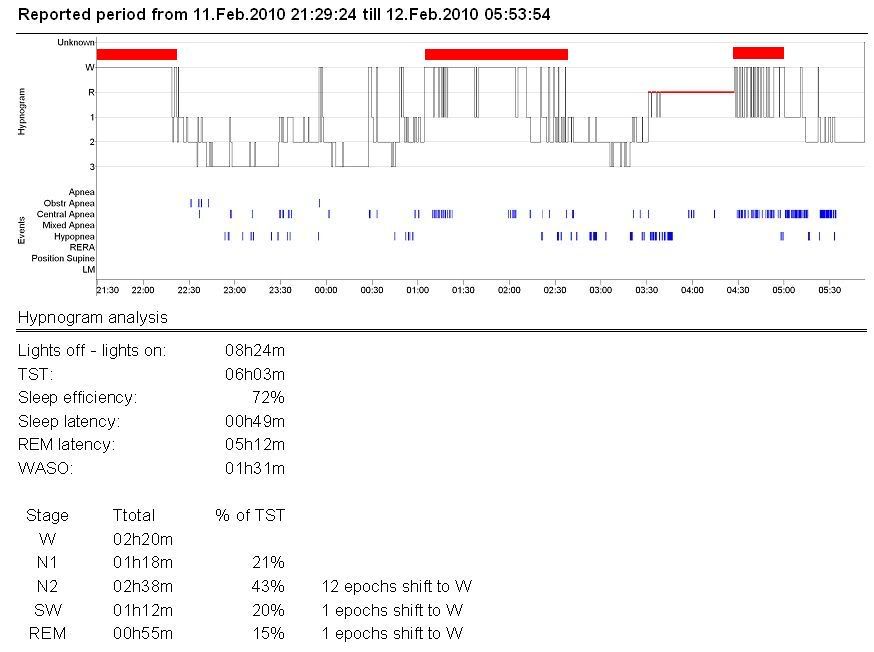
Sleep Efficiency classification should be downgraded from SS to RS.
Muffy
Hi Muffy, Thanks for that - good to have confirmation that my Sleep Centre scoring is consistent with yours.Muffy wrote:Interscorer comparison shows Muffy demonstrating more sleep fragmentation (yet this may be somewhat due to the limitations of the original hypnogram, which makes it difficult to delineate stage changes)...Respiratory scoring shows a few dissimilarities, but generally seems pretty close.
Can you please spell out SS and RS? Sort-of Stuffed and Really Stuffed? Short Sleeper and Regular Sleeper? Cheers,Muffy wrote:Since Lights Out was ~2130, then the initial inability to take sleep must also be counted. With Wake and WASO concentrations marked in red...Sleep Efficiency classification should be downgraded from SS to RS.
Sorta Sucks to Really Sucks.blizzardboy wrote:Can you please spell out SS and RS? Sort-of Stuffed and Really Stuffed? Short Sleeper and Regular Sleeper?Muffy wrote:Since Lights Out was ~2130, then the initial inability to take sleep must also be counted. With Wake and WASO concentrations marked in red...Sleep Efficiency classification should be downgraded from SS to RS.
This sounds really familiar to me.blizzardboy wrote: My daytime symptoms:My nighttime symptoms:
- fatigue
- drowsiness
- frequent sighing
- breathlessness with exertion
- low blood pressure
- acidic perspiration: I was told I have "acid skin" by a fitter-and-turner I used to work with due to leaving visible finger prints on most metal I touched!
- tongue is sensitive to acidic foods, gets painful, red and lumpy
- get small bumps forming at the back of the roof of my mouth from time to time, like little blisters
BTW, I rang my sleep doctor today and left a message - I am starting my push to get a full PFT. Cheers,
- migrating joint pain (hands, feet, shoulders, neck, ankles, knees, hips)
- morning stiffness (alleviated with movement)
- low body temperature
| Mask: ResMed AirFit™ F20 Mask with Headgear + 2 Replacement Cushions |
| Additional Comments: Pressure: APAP 10.4 | 11.8 | Also Quattro FX FF, Simplus FF |
Why not buy some ordinary pH test strips down at the chemist or pharmacist? You can detect those hypothetical oscillations in saliva or urine pH. Alternately you can pin-prick as diabetics do daily to directly measure your blood pH.blizzardboy wrote:Maybe I am oscillating between acidosis during the day (hypercapnic) and alkalosis at night (posthypercapnic due to mechanical ventilation on ASV)!
Probably because I am so confused myself, -SWS!-SWS wrote:Unadog, I'm admittedly a little confused about your recommendations regarding the management of debilitating symptoms. ...Or do you plan to continue with symptom management as a supplementary treatment regiment? What general guidelines/advice might you recommend for others in similar circumstances? Thanks.
blizzardboy wrote:I don't like to admit this because I don't want to have a poorly-understood disorder. I just want a meat-and-veg type of problem that is fixed with a not-tested-on-fuzzy-animals-guaranteed-not-to-have-nasty-side-effects-over-the-counter medication, or with an easy-to-buy-setup-and-use device such as an ASV. Tada...problem solved. I don't want to have the ill-defined problem that requires a well-managed, multi-pronged treatment regime including exotic massages, bleeding-edge drugs, sensual massages, ADMs, gentle massages and hours of mind-stretching CBT. Am I really going to end up with a diagnosis of UARS and FM to explain to my work colleagues and try to convince my GP about? Forced to dabble in acupuncture, touchy-feely massages, meditation in a pyramid, and consumption of foods that might as well have been extracted from a worm farm? Get me that PFT...now!
Hi unadog, You are a fighter!unadog wrote:So OSA is a sleep disturbance, great, a primary cause. Threat that! Yeah - about time – I was told for years that physical therapy was a “cure”, but it was worthless without treating the OSA! SOB’s, I told them from 2001 to 2007 that PT didn’t help, it wasn’t just a matter of “strengthening the muscles …”, I used to work out 6 hours a day …
But then I also have centrals. And I am told that opiates can cause centrals. So I try to go off them, but I can’t sleep without the strong pain meds. So I go back on them, and sleep, and guess what – no centrals, even while on opiates! So do they **really** cause centrals, or does the underlying pain cause the arousals which cause centrals? It is very odd to me that that is an accepted tenant of sleep docs, but is clearly false in my case….
And so it goes. People with fibromyalgia are highly sensitive. Does that **cause** arousals, or is it a product of lack of sleep to begin with, so that it is self perpetuating. Acidosis or alkalinity. Is it caused by the sleep apnea, so that you are describing a pathway? Or is it a root cause of pain, and treating it is a cure?
I have heard so many different theories, and I have spent thousands of dollars per year fotr at least 20 years pursuing different solutions, so that I am not sure what to believe, or who to believe, or what avenue to pursue.
Yes, BB. I do have a Black Belt Certification in 6 Sigma ()statistics and quality systems), plus a degree in Logic, so I am a bit on the same wavelength.blizzardboy wrote:History shows that people will tend to create explanations for phenomena, regardless of the presence of scientific proof.
Show me the data. Show me the PFT! Cheers,
I think this is Muffy's "60s pop star" of choice: http://www.dillonaero.com/.unadog wrote:Now can you explain this whole Dillion thing?
Hi jnk, Wise words IMO. Cheers,jnk wrote:Sometimes it helps to give something a name. Sometimes it doesn't. It depends on why you give it a name. What does it change? Does knowing other people face similar problems make the situation easier? ...it is important, in my opinion, not to neglect the overall common-sense things, such as exercise, diet, sleep hygiene, rest, family, friends, joy, love, purpose, and focus. A little placebo effect can sometimes then be the cherry on top.
Hi DD, And I am convinced for now that my joint pain is caused by my use of CPAP due to the rapid and acute onset of this symptom, the total absence of any symptoms such as this prior to CPAP use, and the presence of pain typically only following CPAP use. Hence why I am focused on an explanation for joint pain centred on respiration and blood gases. I just don't feel the need to walk into the FM wood for now. Cheers,DreamDiver wrote:This sounds really familiar to me.
jnk wrote:The first time my health went haywire (I had been recovering from a serious respiratory infection that I could not shake until they dropped a broad-spectrum antibiotic on me), my PCP eventually told me that I fit the definition for chronic fatigue syndrome.
....
Might as well check in to the nursing home at the same time. You ain't neve rcomng out of that maze!blizzardboy wrote:I just don't feel the need to walk into the FM wood for now