Irregular Heartbeat w/OSA?
-
kurtr
Irregular Heartbeat w/OSA?
Does anyone have irregular heartbeat caused by OSA?
During my sleep test after a long apnea my heart would go into a Brady-Tachy irregular beat. Sometimes it does it during the day also.
Does CPAP straighten this out?
Thanks....
During my sleep test after a long apnea my heart would go into a Brady-Tachy irregular beat. Sometimes it does it during the day also.
Does CPAP straighten this out?
Thanks....
- snoozie_suzy
- Posts: 244
- Joined: Fri Jan 06, 2006 2:43 am
- Location: NorthShore, Massachusetts
I'm not sure if OSA is the cause of irregular heartbeats, but I have them too. Mine are PVC's and I've had them for years. Premature Ventricular Contractions and I recently wore a Holter Monitor overnight from the hospital to record them and have an extra beat every three seconds. I am on a beta blocker right now to control them. My cardiologist believes there might be a link to them. I just got diagnosed with severe OSA three months ago. Because I'm still fairly new at treatment, I haven't noticed that they've decreased at all but it will be interesting to see on my next sleep study if they diminish at all.
Suzy
Suzy
_________________
| Mask: Ultra Mirage™ Full Face CPAP Mask with Headgear |
| Additional Comments: after 1.5 years of feeling crummy on regular auto cpap, bileval therapy has changed my life |
-
Guest
This is from Pulmonary and Critical Care Update:
Cardiovascular Abnormalities in Sleep-Disordered Breathing
Here is an excerpt (I highlighted one sentence in red):
Acute Cardiovascular Changes in Apnea
In patients with SDB, repetitive upper airway obstruction during sleep leads to cyclic decrements in airflow (apneas and hypopneas), which are terminated by cyclic brief arousals that lead to transient resumption of airflow. The apnea-recovery-apnea cycle may occur hundreds of times over the night. Varying levels of cyclic oxygen desaturation are associated with respiratory events, with the oxygen desaturation nadir occurring at the termination of the event. The severity of oxygen desaturation depends upon the length of the respiratory events, the completeness of airway obstruction (apnea vs hypopnea), the frequency of respiratory events, and the oxygen stores in the lung, which, in turn, depend upon body weight, body position, and the presence or absence of respiratory disorders. In addition, other factors that affect oxygen delivery and consumption are likely to be important. Because of the normal motor atonia of REM sleep, individuals are more at risk for the development of apnea during REM sleep than NREM sleep. Oxygen desaturation also tends to be more prominent in REM sleep.
In association with recurrent apneas, there are cyclic changes in blood pressure, heart rate, and central hemodynamics, which may have acute effects (Table 2). Blood pressure is lowest at the start of the apnea, increases gradually during the event, and rises markedly at apnea termination coincident with arousal, the nadir of oxygen saturation, and the release of negative intrathoracic pressure and resumption of airflow. The normal dipping pattern of blood pressure during sleep may disappear and be replaced by a pattern such as the one shown in Figure 1. Heart rate decreases during apnea, particularly just before apnea termination, and accelerates with arousal. Pulmonary artery pressure increases with apnea, with the greatest increments during REM sleep in patients with daytime pulmonary hypertension. Reductions in stroke volume and cardiac output, most marked at apnea termination, have been reported in humans, although more recent animal data suggest that stroke volume declines during apnea and returns to normal at apnea termination. Cerebral autoregulation is insufficient to protect the brain from these hemodynamic changes and cerebral perfusion pressure declines, particularly early in apnea when increased intrathoracic pressure is associated with a fall in systemic blood pressure and a rise in central venous pressure with a concomitant increase in intracerebral pressure. Continuous positive airway pressure (CPAP) therapy of SDB has been shown to improve many of these transient hemodynamic changes.
Table 2—Acute Cardiovascular Changes in Apnea Parameters Altered During Recurrent Apneas
Heart rate
Blood pressure
Central venous pressure
Pulmonary artery pressure
Cardiac output
Stroke volume
Cerebral perfusion pressure
Potential Acute Effects
Arrhythmias
Myocardial ischemia
Cerebral ischemia
Nocturnal pulmonary edema
--------------------------------------------------------------------------------

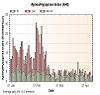
Figure 1. A 9-min polysomnographic segment from a patient with SDB. Note the elevations in systemic blood pressure following apnea termination as well as the transient decreases in systolic blood pressure (arrows) when inspiratory efforts were made during the obstructive portion of the mixed apnea. Reprinted with permission from Shepard.
--------------------------------------------------------------------------------
The acute consequences of SDB during the night may include arrhythmias and conduction disturbances, cardiac and cerebral ischemia, and nocturnal pulmonary edema. Tachy-brady arrhythmia is the most common arrhythmia associated with SDB, but sinus pauses, heart block, and ventricular ectopy have all been described. Owing to an imbalance in oxygen delivery and consumption, acute cardiac and cerebral ischemia may occur in patients with preexisting vascular disease, but this has been less well characterized. Nocturnal pulmonary edema has been described in humans and in animal models of obstructive sleep apnea.
Pathophysiologic Mechanisms of Acute Cardiovascular Changes in Apnea
As detailed in a recent review, the proposed pathophysiologic mechanisms for the acute cardiovascular changes that accompany the apnea-recovery-apnea cycle include (1) negative intrathoracic pressure, (2) hypoxia, and (3) arousals. Negative intrathoracic pressure resulting from upper airway obstruction is associated with increased left ventricular transmural pressure with resultant increased left ventricular afterload and increased venous return to the right heart, leftward shift of the interventricular septum, and resultant decreased preload of the left ventricle. The combination of increased afterload and decreased preload leads to a decrease in stroke volume during apnea and an initial fall in blood pressure. Aortic baroreceptors are activated by the increased transmural intrathoracic aortic pressure, but carotid baroreceptors are inhibited because of the fall in blood pressure related to the decreased cardiac output. Sympathetic nerve activity is initially suppressed because the effect of aortic baroreceptors predominates. As the apnea continues, hypoxia may occur, with or without hypercapnia, and this, in turn, stimulates sympathetic output via peripheral chemoreceptors. Sympathetic activity increases peripheral vascular resistance through a-adrenergic receptors in the peripheral vasculature and increases heart rate and cardiac output through cardiac receptors. Thus, as shown in Figure 2, cyclic changes in blood pressure and heart rate mirror the changes in sympathetic tone. Arousals also contribute to the sympathetic activation at the termination of the apnea.
_______________________________________________________________________
Cardiovascular Abnormalities in Sleep-Disordered Breathing
Here is an excerpt (I highlighted one sentence in red):
Acute Cardiovascular Changes in Apnea
In patients with SDB, repetitive upper airway obstruction during sleep leads to cyclic decrements in airflow (apneas and hypopneas), which are terminated by cyclic brief arousals that lead to transient resumption of airflow. The apnea-recovery-apnea cycle may occur hundreds of times over the night. Varying levels of cyclic oxygen desaturation are associated with respiratory events, with the oxygen desaturation nadir occurring at the termination of the event. The severity of oxygen desaturation depends upon the length of the respiratory events, the completeness of airway obstruction (apnea vs hypopnea), the frequency of respiratory events, and the oxygen stores in the lung, which, in turn, depend upon body weight, body position, and the presence or absence of respiratory disorders. In addition, other factors that affect oxygen delivery and consumption are likely to be important. Because of the normal motor atonia of REM sleep, individuals are more at risk for the development of apnea during REM sleep than NREM sleep. Oxygen desaturation also tends to be more prominent in REM sleep.
In association with recurrent apneas, there are cyclic changes in blood pressure, heart rate, and central hemodynamics, which may have acute effects (Table 2). Blood pressure is lowest at the start of the apnea, increases gradually during the event, and rises markedly at apnea termination coincident with arousal, the nadir of oxygen saturation, and the release of negative intrathoracic pressure and resumption of airflow. The normal dipping pattern of blood pressure during sleep may disappear and be replaced by a pattern such as the one shown in Figure 1. Heart rate decreases during apnea, particularly just before apnea termination, and accelerates with arousal. Pulmonary artery pressure increases with apnea, with the greatest increments during REM sleep in patients with daytime pulmonary hypertension. Reductions in stroke volume and cardiac output, most marked at apnea termination, have been reported in humans, although more recent animal data suggest that stroke volume declines during apnea and returns to normal at apnea termination. Cerebral autoregulation is insufficient to protect the brain from these hemodynamic changes and cerebral perfusion pressure declines, particularly early in apnea when increased intrathoracic pressure is associated with a fall in systemic blood pressure and a rise in central venous pressure with a concomitant increase in intracerebral pressure. Continuous positive airway pressure (CPAP) therapy of SDB has been shown to improve many of these transient hemodynamic changes.
Table 2—Acute Cardiovascular Changes in Apnea Parameters Altered During Recurrent Apneas
Heart rate
Blood pressure
Central venous pressure
Pulmonary artery pressure
Cardiac output
Stroke volume
Cerebral perfusion pressure
Potential Acute Effects
Arrhythmias
Myocardial ischemia
Cerebral ischemia
Nocturnal pulmonary edema
--------------------------------------------------------------------------------

Figure 1. A 9-min polysomnographic segment from a patient with SDB. Note the elevations in systemic blood pressure following apnea termination as well as the transient decreases in systolic blood pressure (arrows) when inspiratory efforts were made during the obstructive portion of the mixed apnea. Reprinted with permission from Shepard.
--------------------------------------------------------------------------------
The acute consequences of SDB during the night may include arrhythmias and conduction disturbances, cardiac and cerebral ischemia, and nocturnal pulmonary edema. Tachy-brady arrhythmia is the most common arrhythmia associated with SDB, but sinus pauses, heart block, and ventricular ectopy have all been described. Owing to an imbalance in oxygen delivery and consumption, acute cardiac and cerebral ischemia may occur in patients with preexisting vascular disease, but this has been less well characterized. Nocturnal pulmonary edema has been described in humans and in animal models of obstructive sleep apnea.
Pathophysiologic Mechanisms of Acute Cardiovascular Changes in Apnea
As detailed in a recent review, the proposed pathophysiologic mechanisms for the acute cardiovascular changes that accompany the apnea-recovery-apnea cycle include (1) negative intrathoracic pressure, (2) hypoxia, and (3) arousals. Negative intrathoracic pressure resulting from upper airway obstruction is associated with increased left ventricular transmural pressure with resultant increased left ventricular afterload and increased venous return to the right heart, leftward shift of the interventricular septum, and resultant decreased preload of the left ventricle. The combination of increased afterload and decreased preload leads to a decrease in stroke volume during apnea and an initial fall in blood pressure. Aortic baroreceptors are activated by the increased transmural intrathoracic aortic pressure, but carotid baroreceptors are inhibited because of the fall in blood pressure related to the decreased cardiac output. Sympathetic nerve activity is initially suppressed because the effect of aortic baroreceptors predominates. As the apnea continues, hypoxia may occur, with or without hypercapnia, and this, in turn, stimulates sympathetic output via peripheral chemoreceptors. Sympathetic activity increases peripheral vascular resistance through a-adrenergic receptors in the peripheral vasculature and increases heart rate and cardiac output through cardiac receptors. Thus, as shown in Figure 2, cyclic changes in blood pressure and heart rate mirror the changes in sympathetic tone. Arousals also contribute to the sympathetic activation at the termination of the apnea.
_______________________________________________________________________
- NightHawkeye
- Posts: 2431
- Joined: Thu Dec 29, 2005 11:55 am
- Location: Iowa - The Hawkeye State
None Since Beginning Therapy
Before xPAP therapy I had frequent (as in nightly) incidents of atrial flutter/fibrillation; not a single incident in the three weeks since starting xPAP therapy though. Also had bradycardia which caused oximeter to alarm occasionally. It too, appears reduced now.
Regards,
Bill
Regards,
Bill
I also had severe PVC. At times I'd throw a PVC every 2nd or 3rd beat. Went for nuclear stress test, and finally an angiogram. Absolutely nothing wrong with my heart. Except it throws PVCs. They don't know what causes them and the medication they give you doesn't really STOP them. It just makes it so you don't notice them as much.
The GOOD news is that after about 50 days of 100% compliance on my new auto PAP, I have not had a PVC episode. I'm reasonably sure that, at least in MY case, it has something to do with oxygen levels or varying blood pressure and that the APAP is treating the condition that got the PVCs going.
BUT (and it's a big but) since MEDICALLY they do not know what CAUSES PVCs, I can only take my best guess. Several of these heart symptoms could have different triggers in different people. So CPAP therapy may or may NOT work depending on what the underlying cause may be.
wow... I really DO ramble.... my wife is RIGHT!
The GOOD news is that after about 50 days of 100% compliance on my new auto PAP, I have not had a PVC episode. I'm reasonably sure that, at least in MY case, it has something to do with oxygen levels or varying blood pressure and that the APAP is treating the condition that got the PVCs going.
BUT (and it's a big but) since MEDICALLY they do not know what CAUSES PVCs, I can only take my best guess. Several of these heart symptoms could have different triggers in different people. So CPAP therapy may or may NOT work depending on what the underlying cause may be.
wow... I really DO ramble.... my wife is RIGHT!
_________________
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: original pressure 8cm - auto 8-12 |
- NightHawkeye
- Posts: 2431
- Joined: Thu Dec 29, 2005 11:55 am
- Location: Iowa - The Hawkeye State
Keep on ramblin
Yardbird, what you've written is not rambling at all. It is clear, precise and to the point; quite the opposite of rambling.wow... I really DO ramble.... my wife is RIGHT!
Regards,
Bill
-
LittleAudrey
Re: Irregular Heartbeat w/OSA?
Yes. My OSA is mild. I have been on CPAP therapy for a little over a month now. It all started with arrhythmias (eventually diagnosed as three heart blocks, PVCs/PACs and, on a Holter monitor, 30 minutes of atrial flutter with rapid heartbeat) and breathing/swallowing problem while first trying to sleep. It then became uncharacteristic (for me) anxiety while trying to sleep, then during the day at certain times. I feel like I've been around the world feeling like an invalid and not knowing what my fate would be.kurtr wrote:Does anyone have irregular heartbeat caused by OSA?
During my sleep test after a long apnea my heart would go into a Brady-Tachy irregular beat. Sometimes it does it during the day also.
Does CPAP straighten this out?
Thanks....
Honestly I have no concrete evidence that CPAP therapy has straightened it out. My anxiety (for a variety of reasons) is all but gone, except for a few known trigger situations (if you will:-) that bring it out. That relief began when several things were ruled out as causes of my symptoms.
CPAP seems to be bringing me full circle. Funny that I use the F&P Opus 360 pillows mask;-) It took a good 10 days to get used to it and the absolutely foreign act of breathing over the machine. I know this is an old thread, but was apropos to my situation. I never actually had the typical SA symptoms. I had to push for a sleep study after reading an article about the number of people (in the study) with pacemakers who had untreated sleep apnea.
I have read precious few posts like mine, which means that no case is exactly alike. I feel exceedingly lucky to have had an easy transition to therapy. I have a friend who was SUPPOSED to have been religiously using CPAP for more than 5 years now. Not really my place to tell her story, but suffice it to say that she is very much my my "canary in the coalmine."
Re: Irregular Heartbeat w/OSA?
What started me on CPAP was PVC's, I was getting it so bad for two weeks that my heart was skipping every 3 seconds. Some days I had none (usually when I had the holter monitor on) and some days was mild and some terrible. Most brought on by stress, caffeine oh and the big killer SLEEP APNEA!
After about 6 months I had a sleep study and they realised my AHI was 141.2 (pretty high!) Since being on CPAP/APAP my PVC's have reduced substantially. I still have them usually on days when I drink a lot of caffeine, stress levels are high but overall PVC's and skipped beats are better for me.
After about 6 months I had a sleep study and they realised my AHI was 141.2 (pretty high!) Since being on CPAP/APAP my PVC's have reduced substantially. I still have them usually on days when I drink a lot of caffeine, stress levels are high but overall PVC's and skipped beats are better for me.
Re: Irregular Heartbeat w/OSA?
I have something that is hard to describe. I don't know if this is skipping like dave21 said but it is like this:
/\ /\
---/\---/\---/\--------/ \---/\---/\---/\--------/ \---
Sorry for the terrible sinus graph that I draw but this is how my heart works. It is not all the time, I may have this occurrence once a day or every two days, or simple stops for a while and then comebacks. It is like skipping but then comes back strong.
Anyone experience anything like this?
EDIT. The /\ at the first line of the graph should be at the top of the skip beat in the second line. I guess the forum software does not recognize the spaces
/\ /\
---/\---/\---/\--------/ \---/\---/\---/\--------/ \---
Sorry for the terrible sinus graph that I draw but this is how my heart works. It is not all the time, I may have this occurrence once a day or every two days, or simple stops for a while and then comebacks. It is like skipping but then comes back strong.
Anyone experience anything like this?
EDIT. The /\ at the first line of the graph should be at the top of the skip beat in the second line. I guess the forum software does not recognize the spaces
Last edited by fidelfs on Tue Mar 23, 2010 3:13 pm, edited 1 time in total.
Re: Irregular Heartbeat w/OSA?
Yeah Fidelfs I get that all the time. Apparently nothing to worry about but the beat after the pause sure can be felt!
_________________
| Machine: Airsense 10 Card to Cloud |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Emay EMO-60 oximiter |
Re: Irregular Heartbeat w/OSA?
Tachycardia and PVC's (you can have one without the other) can be caused by a lot of things--benign and not so benign--including stress and an apnea episode. Before being treated for OSA, I would wake up once every couple of months with my heart racing (tachycardia) at about 160 beats a minute. After walking around for a few minutes, it would slowly go back down to normal. I don't get that any longer, but I do get PCV's (AKA"skipped" beats--although they're not really skipped) that have been declared as not something worry about by my doc. Have had them for as long as I can remember--which is a LOOONG time, 'cause I'm old (LOL). When I'm stressed I get them more often.
_________________
| Machine: DreamStation 2 Auto CPAP Advanced with Humidifier |
| Additional Comments: Oscar Software | APAP: 9-10 |
Re: Irregular Heartbeat w/OSA?
I don't know if it's the same thing, but when I was having PVC's, that would probably be the way that I would try to 'draw' then on a keyboard. IF they are PVC's they are probably nothing to fret over. Everyone has some of them. While a PVC feels like a skipped beat, it is actually and extra beat from the ventricle. If they are severe enough, your cardiologist may put you on a beta blocker to control them. If it concerns you or changes your life-style, see your cardiologist. Most likely, he will tell you there is nothing serious going on. That news alone can be a big stress reliever.fidelfs wrote:I have something that is hard to describe. I don't know if this is skipping like dave21 said but it is like this:
/\ /\
---/\---/\---/\--------/ \---/\---/\---/\--------/ \---
Sorry for the terrible sinus graph that I draw but this is how my heart works. It is not all the time, I may have this occurrence once a day or every two days, or simple stops for a while and then comebacks. It is like skipping but then comes back strong.
Anyone experience anything like this?
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Additional Comments: EPAP = 12 / IPAP = 12-20 / Backup rate = AUTO / Central Sleep Apnea - Cheyne-Stokes Respirations diagnosed May 29, 2009; otherwise healthy |
Re: Irregular Heartbeat w/OSA?
The PVC's or what's termed as skipped heart beats is when you feel a sudden THUD from your heart. It's usually because your heart is beating normally then there's a slight gap (one beat that doesn't come in on time) then your heart picks up and you get two beats at the same time (which feels like the thud).
This thud (or PVC) / skipped beat, can happen as much as once every couple of seconds in worse conditions. Usually when I get it really bad I get the PVC every 2-3 seconds but since being on CPAP that's very rare now, most of the time if I do get it under stress then it can happen about once or twice every minute.
This thud (or PVC) / skipped beat, can happen as much as once every couple of seconds in worse conditions. Usually when I get it really bad I get the PVC every 2-3 seconds but since being on CPAP that's very rare now, most of the time if I do get it under stress then it can happen about once or twice every minute.
Re: Irregular Heartbeat w/OSA?
I never felt the 'thud' when I have/had PVC's. I knew when they started, though, because I could feel myself suddenly get short-of-breath, even if I had been inactive; sitting at the computer, watching TV, etc. I don't think my cardiologist really believed me much, though, until I wore a 30-day event monitor, which confirmed PVC's were happening when I got short-of-breath.
Tony
Tony
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Additional Comments: EPAP = 12 / IPAP = 12-20 / Backup rate = AUTO / Central Sleep Apnea - Cheyne-Stokes Respirations diagnosed May 29, 2009; otherwise healthy |
Re: Irregular Heartbeat w/OSA?
Shortness of breath, feeling faint, feeling tight chested, butterfly type sensation around your chest (instead of your stomach) and thuds / skipped beats, are all symptoms of PVC's