SleepySandy wrote:...and do the 3 I had during my titration study matter?
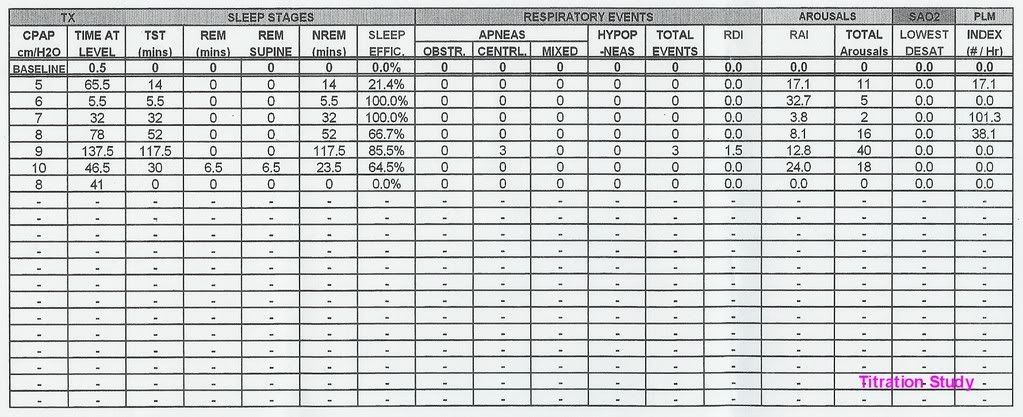
I'm not even sure if this is something to worry about but on Friday I finally received additional information about my first sleep studies - posted below. It showed that I had 3 centrals during my titration study when the pressure was 9. I didn't know about this until Friday. My prescribed pressure has been 10. I didn't have any centrals at 10 during my titration study but I wasn't at 10 for very long compared to the length of time I was at 9.
I just saw the post by Daffney_Gillfin about Silverlining and I saw how Silverlining shows central apneas.
I'm wondering if the Respironics and Resmed machines recognize centrals. I have had a Respironics M Series Pro for a few months and I have EncorePro. It shows apneas but I don't know if that includes centrals.
My new sleep doc just prescribed a new machine for me - a Resmed S8 Vantage Auto. I'm going to the DME tomorrow.
The prescription form is preprinted and has the M-Series Auto and the Resmed Auto listed. My sleep doc has been certified since 1985 and one of the C-Flex studies was done at his clinic. So, I'm hoping he knows more about the machines than the average sleep doc. I didn't notice that he specified a brand until I got home - I was too shocked that
he recommended an Auto (I hadn't brought it up). I'm going to be calling tomorrow to find out why he chose the Resmed machine for me. But, I'm wondering about the centrals and if I need to consider the Puritan Bennett machine if the Resmed or Respironics machines don't recognize centrals. If the central events during my titration study matter...
I'm so confused
My current sleep doc hasn't seen this information since I just got it on Friday (he has seen the summary reports). The studies were under my former sleep doc. The info I got on Friday also included graphs. If seeing the graphs would be helpful, they're here:
viewtopic/t18905/Help-Interpreting-Slee ... -mean.html
Thanks in advance for your help.
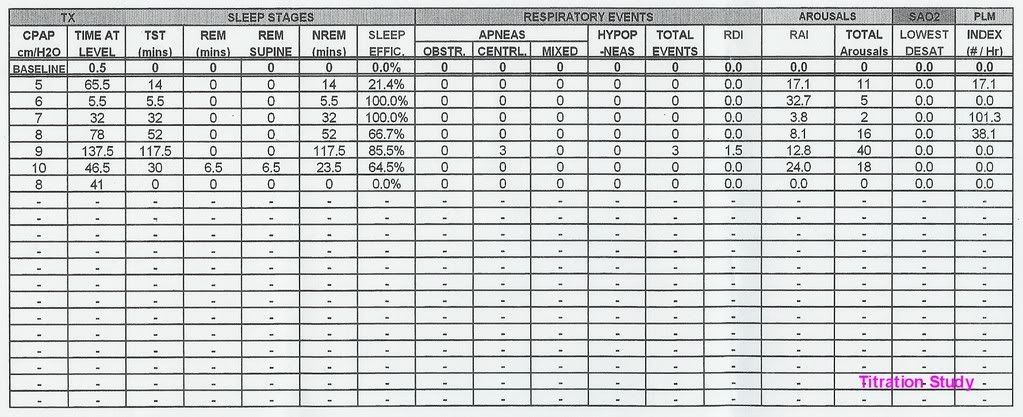
Based upon your titration table, the Resmed S8 Vantage is about the worst machine your doctor could possibly prescribe.
It does a lousy job at avoiding central apnea. Then if you snore it will increase pressure for as long as that snore exists all along ignoring pressures that trigger central. A Remstar will increase pressure by .5cm then monitor, if event still there increase again, then monitor. On the Resmed snore detection mic is on the pressure transducer circuit. Next it has a A10 algorithm, which basically says it won't respond to any apnea whenever the pressure is at 10cm or above.
Look at your titration table, you had 3 Centrals at only 9cm pressure, what do you think setting that threshold to 10cm will do? Yep you guess it, the Vantage command on apnea is already 1cm above your threshold. Look again at your titration table, they went from 9cm (where the 3 centrals where seen) back DOWN to the prior 8cm pressure where sleep was again stable, that was 8cm which is listed in the last line of the titration table. Based upon that data,
your pressure is 8cm not 10cm.
Respirionics NRAH response: It is more an error report that the machine screwed up vs being any kind of Central Apnea detection. The reason is the machine has to see an apnea event remain after 3 prior pressure increases (that is a LONG time when you think about it) before it finally decides that the event did NOT respond to a pressure increase. Very rare if it logs one at all.
I can go from my m series (or classic it doesn't matter which) to the 420e and I can see Centrals show up the very next night and EncorePro reported ZERO "NR" events weeks prior. So is it I didn't have any Centrals or is it the Remstars didn't detect any? My money is on the latter, the Remstar didn't detect any. It is also why I cannot allow a Remstar to run higher than 9cm, if I do it will only climb up to the maximum set pressure.
You would think if I was having regular CA's almost every night detected on a 420e only detecting 6 out of 10 possible centrals seen that I would at least have 1 "NR" event show up. By the time "NR" shows up on a EncorePro report your sleep is already a train wreck.
While Respironics technically classified it correctly as Non-Responsive (an event that didn't respond to prior pressure increases). This ALSO means that if the event went away after only 1 or 2 pressure increases that it would never be scored as a "NR". Even if that event was actually a central event.
What NR really says is: "well that one didn't respond after 3 consequtive pressure increases so ooops! it must have been a central, but we cannot admit we screwed up and applied pressure to a central event so we'll call it Non-Responsive.
You need to address those other PLMD arousals seen on your PSG, those are going to cause you more interruptions to your sleep than the 3 centrals seen. But it seems if you get the right therapy all of those events settle down. I would try the 420e over any other machine. At least you will be able to see more than what you have now.
I bet if you set your current machine down to 8cm pressure you would do better than you did the night before.
someday science will catch up to what I'm saying...