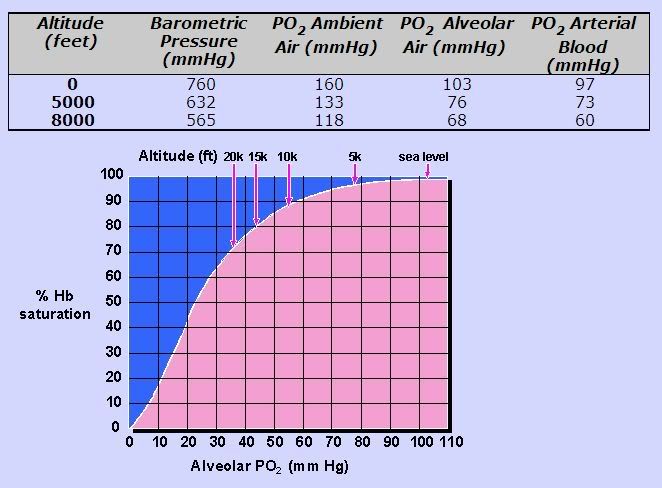
I'll mention the pulmonary testing to the new doctor. My first two sleep studies (in late 2007) were done in Phoenix (elevation of about 1,100 feet). I live in the mountains, at about 4,700 feet. My third and fourth studies were done in my doctor's lab at about 5,000 feet.StillAnotherGuest wrote:OK, sounds like you should make some good headway with your potential new physician. I think a good pulmonary workup is a great idea, which you should get there. This might include the aforementioned pulmonary function test and a pH, pCO2 and pO2 analysis (see Slinky, I didn't say "***"). CompSAS is generally a syndrome of hypocapnia (low pCO2) but due to some breathing restriction, you may have a little hypercapnia (elevated pCO2). And that oxygen baseline hovers a little low on PSG, which gives supplemental oxygen with PAP at least a quick look-see.
BTW, what is the elevation of where you live/where you were tested?
The ASV question is already on my list. I'm not sure what short-cycle and long-cycle means; I've done a little research on CompSAS since I joined the forum here, but I'm so tired, I'm having a hard time comprehending it all and am not retaining the info as well as I should. I asked the receptionist I spoke with whether the doctor utilizes ASV's, but she said that's something I'd have to discuss with the doctor. A consultation is scheduled for a full hour, which is good news; I always feel like my current sleep doctor is in a rush to shoo me out.More questions to ask on the visit:
RIght off, ask if they employ Adaptive Servo Ventilation machines (don't automatically assume they do, and that's a good "ice breaker" to show you know what you're talking about without being too threatening).
If they use ASV, find out which they prefer. If they use the Respironics ASV, we need to determine if you're a long-cycle or a short-cycle CompSAS (although with an AHI of 107, it's probably a safe bet you're a short cycle. Bev, clearly, is a long-cycle).
I'm not a pill-taker by choice, but I'll ask about it.See if they encourage the use of hypnotics (like zolpidem) to help stabilize sleep. That's very "in" right now.
I'll have no problem using straight CPAP, if that's what this new doctor tells me is best for me. If that's the case, my only demand will be an upgraded machine with full data capability. I'll be more than happy to discuss my progress with an interested doctor, but I want and need to be able to monitor my own treatment to determine what works best for me.Not using ASV, or to any great extent, is not necessarily a problem. As noted before, routine CPAP, and time, is being used a lot these days.
SAG
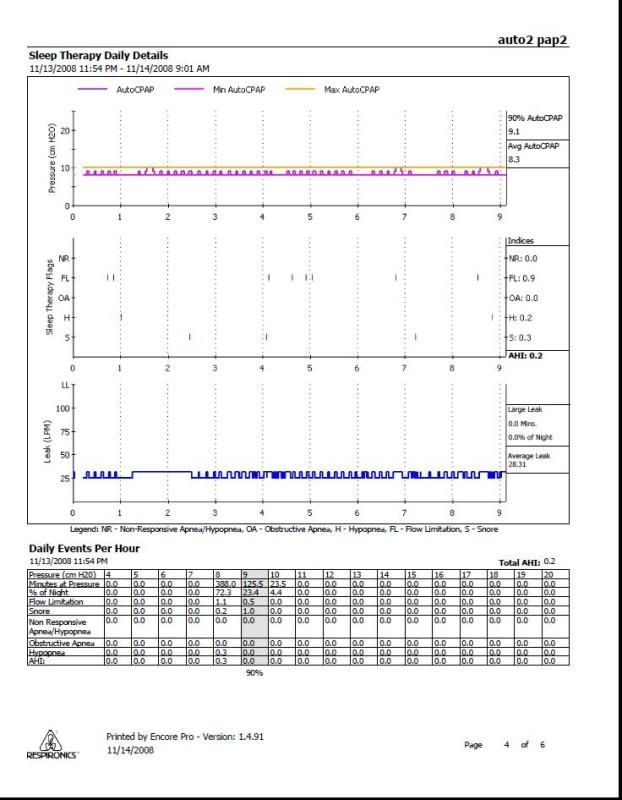
As an aside, I can't wait to return this loaned Autopap machine tomorrow. I haven't felt this tired since before I started CPAP therapy. After a week of what feels like useless therapy from this loaner and repeatedly talking myself out of just abandoning it in favor of my plain old CPAP at 14 cm, I'm ready to rumble with my doctor's office. If I don't get the right answers to my questions tomorrow morning, I'll have to try very hard to keep my head about me and hold my tongue, or I'll fire him on the spot, before I even see the new doctor. I'm in no mood...
Thanks, SAG. I'm taking notes from you and others.