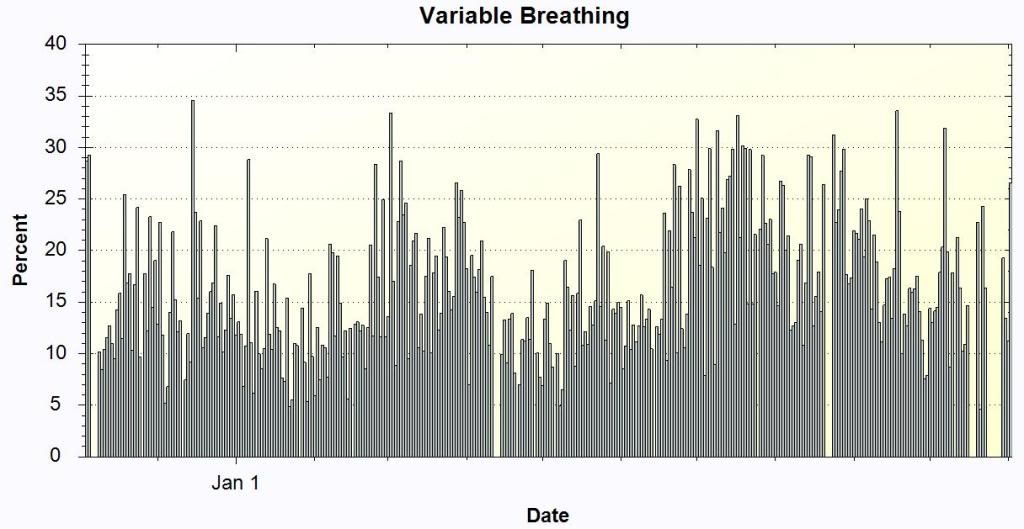
-SWS wrote:...your variable breathing percentages on those charts don't look dissimilar to many Encore reports that have been presented.
However, since nobody here can be considered "normal", I would conclude that that observation means that this is an abnormal result.
I would like to create a "Living Document" to determine an interpretive strategy for the variable breathing (VB) parameter, and would like to start out with:
< 5.0% Normal
5 - 15% Mild Disturbance
15 - 25% Moderate Disturbance
> 25% Severe Disturbance
I know one person, whom I consider to be quite "normal", with a VB of 0%.
And this would put some of dilfo's values in a different dimension.
In an update of an earlier post.......
I would say the contributors to the VB are:
Normal variation (REM sleep, normal wake periods)
Abnormal variation (insomnia, wake/1 transition, arousals from non-respiratory events)
Whatever the VB criteria actually is.
Criteria when it can't kick in (the algorithm hierarchy seems to say that if there are leaks, snores, or apnea/hypopnea, you can't enter Variable Breathing Mode (VBM)(I just made that up, too)(the acronym, not the hierarchy). That's why I believe Periodic Breathing, when there are apneas, would not be relegated to the VB Bucket.
BTW, in a limited study of Periodic Breathers (one) analyzed by Encore 1.8.49 (not the current version recommended for AutoSV) the reported value of PB appeared to be low relative to the clinical situation. But until somebody can cough up the actual algorithm, I don't think anybody should put the mortgage down on the table at the Indian place on what they think the PB% means.
VB is not necessarily related to variable breathing per se, but rather the machine is in VBM. It has seen some erratic breathing and has suspended titration mode. Whether the erratic events are continuous or not is not known.
The basic goal of VBM seems to move the patients back to the setting that was in effect before the onset of erratic breathing. In both APAP and AutoBiPAP, this is accomplished slowly, at a rate of 0.5 cmH2O/minute, up to 2.0 cmH2O (using IPAP in AutoBiPAP, affecting EPAP only if an IPAP change would necessitate an EPAP change because of PS restrictions). Also, pressure changes are tempered based on the presence or absence of snoring prior to the initiation of VBM.
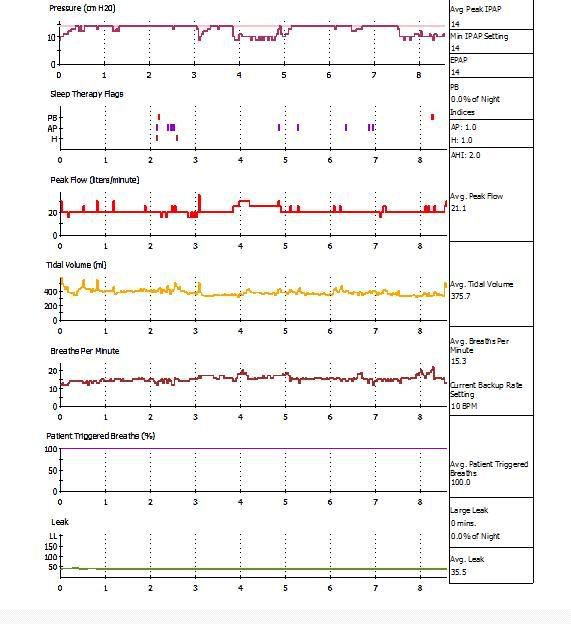
If you could match up VB Mode to time that would be extremely helpful, but I think you can only view VB vs Pressure.
REM sleep in adults is generally pretty stable, at least stable enough that if you see 25% VB you shouldn't think it's all REM. I mean, there may be a little variation, but I think the point of considering VB in REM is that you don't want to poke at it at all with unnecessary pressure changes.
If your NPSG shows decreased sleep efficiency, increased stage shifts (especially Stage 1), increased spontaneous AI and/or increased PLM AI, Ihen I would think those would be the most likely suspects.
In a basic edit of the mechanics of VBM from the patent ("VBPC Lite", so that ol' SFB Mike can understand this)(but this might not even be what's in there now):
Variable Breathing Pressure Control
Once the variable breathing controller has been granted control of the pressure support system, it takes some initial action based on the action the auto-CPAP controller is taking. After this initial action, it performs an independent pressure control operation.
A prior pressure that is flat will cause the pressure delivered to the patient to remain at that level.
A prior pressure that is increasing will cause the variable breathing controller to initially decrease the pressure delivered to the patient at a rate of 0.5 cmH2O per minute. The magnitude of the decrease is dependent on the magnitude of the increase in prior pressure. The pressure decrease is intended to erase the prior pressure increase that possibly caused the variable breathing. However, the total decrease in pressure drop is limited to 2 cmH2O. After pressure decrease, the variable breathing controller holds the pressure steady.
A prior pressure that is decreasing will cause the variable breathing controller to initially increase the pressure delivered to the patient at a rate of 0.5 cmH2O per minute. The magnitude of the increase is dependent on the magnitude of the decrease in prior pressure. The pressure increase is intended to erase the prior pressure decrease that may have caused the variable breathing. However, the total increase in pressure is limited to 2 cmH2O. After pressure increase, variable breathing controller holds the pressure steady.
The pressure curve is provided for 5 minutes or until the variable breathing condition clears. Thereafter, the pressure is controlled according to the following:
The pressure is either maintained at a constant value, or it follows a decrease and hold pattern. The decision to hold the pressure or to decrease the pressure is made by comparing the current pressure with the snore treatment pressure. It is to be understood, however, that this duration can be varied over a range of durations.
If there is no snore treatment pressure stored in the system, which will be the case if the snore controller has not been activated, the pressure is held constant. If there is a snore treatment pressure, and if the current pressure is more than a predetermined amount above this snore treatment pressure, such as more than 2 cmH2O above the snore treatment pressure, the variable breathing controller decreases the pressure to a level that is a predetermined amount higher than the snore treatment pressure and holds the pressure at the lower level. The pressure decreases to the snore treatment pressure +1 cmH2O.
The duration during which pressure is provided according to the paradigms discussed above for region is set to 15 minutes or until the variable breathing condition clears. It is to be understood, however, that this 15 minute duration can be varied over a range of durations.
SAG