One thing pretty consistent in her Lab studies, NO REM. While Bev mentioned melatonin caused her to have vivid dreams, they may have been from not having any for a long long time. I would certainly give it another shot, she may have tried to reach it in one of her studies because they showed a PLM in that report. Either that or if the doctor can try a different medication than lexapro that doesn't supress REM so much.-SWS wrote:We can see an untreated AHI of about 15 at 0 cm pressure here: 152.6 minutes total recording time at 0 cm
CPAP sounds warranted. And there are plenty of symptoms that sort of sound like cataplexy that really aren't cataplexy after all.
Wonder if Walgreens carries over-the-counter tests for either CSF hypocretin levels or HLA subtype DQB1*0602 yet... (just kidding)
Why doesn't APAP respond to apneas?
Re: Why doesn't APAP respond to apneas?
someday science will catch up to what I'm saying...
Re: Why doesn't APAP respond to apneas?
I will add mine but wont get at it for nuther 5 hrs. It is I believe about 1 year old - I got it used but it only had about 20 hrs or less on it.-SWS wrote:Would other AutoSV owners/clinicians mind chiming in if they have a firmware version later than 1.3? Thanks.OutaSync wrote:My SV is version 1.3
Sure hope version 1.3 is bluetooth, firewire, SATA, USB2, and 64-bit Vista compatible...
I do know that the 1st versions of SV well selling in 2005 in the synchrony shaped case. The Respironics SV machine has been around awhile. In those days it was targetted at CHS (Cheynes Stokes) patients later 2007 (IIRC) they expanded the target user base.
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: Why doesn't APAP respond to apneas?
Thanks for checking, dsm!
Bev, if you typically go into a dream state almost immediately after falling asleep then you're probably experiencing SOREMPs highly typical of narcolepsy. But a lack of very quickly reaching a dream state right after sleep onset (without Lexapro or other REM suppressing drugs) very strongly suggests that you do not have narcolepsy. No laughter-based (especially) or strong emotion-based cataplexy also suggests that you do not have narcolepsy.
The good news is that Bev discontinued Lexapro.Snoredog wrote:Either that or if the doctor can try a different medication than lexapro that doesn't supress REM so much.
Bev, if you typically go into a dream state almost immediately after falling asleep then you're probably experiencing SOREMPs highly typical of narcolepsy. But a lack of very quickly reaching a dream state right after sleep onset (without Lexapro or other REM suppressing drugs) very strongly suggests that you do not have narcolepsy. No laughter-based (especially) or strong emotion-based cataplexy also suggests that you do not have narcolepsy.
Re: Why doesn't APAP respond to apneas?
Bev, I've been silent on this thread recently because I can't get a grasp of the SV and the reasons for using it.
I'd like to summarize a few points about your condition for all of us - this is all taken from your posts, Please correct the thing I've got
wrong:
You are 5'8", 125 lbs and had been complainning to your doctors for 30 years of an inablilty to sleep.
Your pre cpap AHI was 20 - that was on you sleep study.
viewtopic.php?p=212622#p212622
You got a cpap with Rx fof 16, struggled with it, the doc's response was to drop the pressure to 12 and then to 10.
Your AHI ranged from 28 to 38 on fixed pressure, when you had leak problems
With an Auto at 6-20 you had and AHI of 17.6 and the events came in clusters.
sleep at all.
A drop to 6.5 to 13.5 raised your AHI and did not help the terrible aerophagia.
You were on Lexapro for most of the first year of therapy, weaned yourself from it sometime in the summer. viewtopic.php?f=1&t=35018&p=300502#p300502
For what its worth, this is my summary and interpretation of what I've read:
I would try either a the 420E, which responds to apneas faster than a Respironics and can identify some central apneas and not respond to them (if they occur at all, or a fixed bi-level that would give you the ability to have higher pressure on inhale only.
A PB420E in combinaton with TimeSnapper can let you pin poin exactly what happen before, during and after each apnea, because you can get a second by second break down of your breathing. (I'll post an example of that breakdown later on).
Once you've really got the Lexapro out of your system - I don't know how long that takes - I would look for a good cognitive behavioral theapist to help you with you sleep problems.
Early on in this thread I suggested the banquet hall on you minimum pressure indicated your breathing pattern confuses the Respironics. Here carboman's recent report, look at the minimum there.
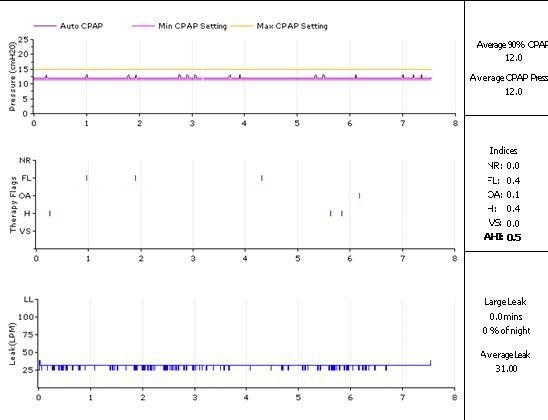
His min. is at his recommended 90%, and his machine is doing very little of that "can we do any better? yes we can , ohno we can't " cycling.
O.
I'd like to summarize a few points about your condition for all of us - this is all taken from your posts, Please correct the thing I've got
wrong:
You are 5'8", 125 lbs and had been complainning to your doctors for 30 years of an inablilty to sleep.
Your pre cpap AHI was 20 - that was on you sleep study.
viewtopic.php?p=212622#p212622
You got a cpap with Rx fof 16, struggled with it, the doc's response was to drop the pressure to 12 and then to 10.
Your AHI ranged from 28 to 38 on fixed pressure, when you had leak problems
With an Auto at 6-20 you had and AHI of 17.6 and the events came in clusters.
You doctor did mention that the next step might be bi-level, and you had a second - bi-level sleep study on which you felt you didn'tWhen I was on the straight CPAP I tried lowering my pressure and as it went down the QHIs seemed to go up. At a pressure of
10 it got up to 44. That is whent the Dr. told me that I should be at 19 but he didn't think I could tolerate that pressure so he set it at
16.
sleep at all.
I start out sleeping on my back, but after awhile my back hurts so I turn on my side and then my shoulder hurts, so it's a lot of
tossing and turning and waking up to mask leaks, belching, passing gas, hot flashes. My last sleep study had me waking up 29
times during the night and that was with an Ambien and with CPAP.
You never had a follow up for a bi-level, you did insist on an SV in your June 2008 appointment.I've been 100% compliant for over 8 months and take Melatonin and Ambien every night. I still am wakened numerous times
duting the night with flatuence. As soon as I sit up the air in my stomach comes up, but the air in my gut leaks out all day in the most
uncomfortable and embarassing way!
A drop to 6.5 to 13.5 raised your AHI and did not help the terrible aerophagia.
You were on Lexapro for most of the first year of therapy, weaned yourself from it sometime in the summer. viewtopic.php?f=1&t=35018&p=300502#p300502
As I said, I don't understand the SV, and why it was suggested.Another thing that I"ve noticed is that the machine rarely increases pressure when I have an apnea. It doesn't react at all. That's why I have the bottom raised so high. If i let the top pressure go up, I get NRs, so I have to cap that, too. I've been on CPAP for a year and have NEVER woken up feeling refreshed. Although I'm better than a year ago when I was spending 40 minutes a night in apnea.
For what its worth, this is my summary and interpretation of what I've read:
- You've got sleep apnea - as indicated in your PSG
Your long standing sleep apnea has had a bad impact on your ability to fall asleep and to maintain sleep.
During year on CPAP therapy you've been taking a drug "used to treat mental depression and generalized anxiety disorder" which is also know to inhibit REM sleep, the side effects of which are the following:
(this is from the Mayo clinic). Those are common side effects of that medication, I've colored the one's you've been suffering from.More common
Constipation
Decreased interest in sexual intercourse
Diarrhea
Dizziness
Dry mouth
Ejaculation delay
Gas in stomach
Heartburn
Impotence
Inability to have or keep an erection
Increased sweating
Loss in sexual ability desire, drive, or performance
Nausea
Sleepiness or unusual drowsiness
Sleeplessness
Stomach pain
Trouble sleeping
Unable to sleep
You are concerned at the lenght of your apneas, and the fact your machine does not raise pressure after they occur.
You are using a machine that needs 3 apneas to happen within a couple of minutes before it figures out it has to raise the pressure.
I would try either a the 420E, which responds to apneas faster than a Respironics and can identify some central apneas and not respond to them (if they occur at all, or a fixed bi-level that would give you the ability to have higher pressure on inhale only.
A PB420E in combinaton with TimeSnapper can let you pin poin exactly what happen before, during and after each apnea, because you can get a second by second break down of your breathing. (I'll post an example of that breakdown later on).
Once you've really got the Lexapro out of your system - I don't know how long that takes - I would look for a good cognitive behavioral theapist to help you with you sleep problems.
Early on in this thread I suggested the banquet hall on you minimum pressure indicated your breathing pattern confuses the Respironics. Here carboman's recent report, look at the minimum there.
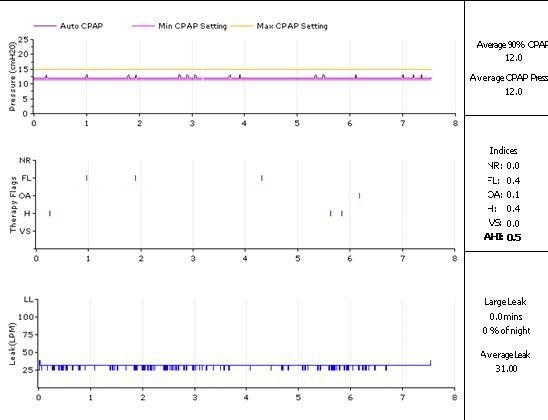
His min. is at his recommended 90%, and his machine is doing very little of that "can we do any better? yes we can , ohno we can't " cycling.
O.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Re: Why doesn't APAP respond to apneas?
My SV version is 1.2-SWS wrote:Would other AutoSV owners/clinicians mind chiming in if they have a firmware version later than 1.3? Thanks.OutaSync wrote:My SV is version 1.3
Sure hope version 1.3 is bluetooth, firewire, SATA, USB2, and 64-bit Vista compatible...
DSM
Now where can we find out about the differences
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Re: Why doesn't APAP respond to apneas?
That's great, the way you've gathered so much of Bev's info in one spot, ozij.
There aren't enough chairs along carbonman's pressure line to have much of a Thanksgiving dinner gathering, are there? Wow, that's steady. Bet he could leave IFL1 on for sure, if he were using a 420E. Interesting.ozij wrote:His min. is at his recommended 90%, and his machine is doing very little of that "can we do any better? yes we can , ohno we can't " cycling.
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Re: Why doesn't APAP respond to apneas?
Thanks very much for consolidating all that information, ozij!
Do I think that Bev's titration charts above are describing problems with flow limitations? Flow limitation scoring is not included in those PSG charts. But I don't believe Bev's proven erratic tendencies for much harder Apnea and Hypopnea closures can be explained by tiny, perhaps even barely measurable flow limitation closures. If nearly imperceptible airway closures are the cause for all those much larger airway closures, we're on to.... chaos and bifurcation of all things! And a yet another proposed sleep disordered phenotype.
If we can fix all those symptoms in Bev's pathophysiology by bumping pressure to eliminate marginal flow limitations, then I'm kind of thinking that treatment trend would have been previously discernible by both the medical and patient communities. There's no doubt in my mind that UARS pathology can be mitigated by simply removing flow limitations, but I think that strategy cannot fix the hard Apnea and Hypopnea pressure-associated disorder we see on those titration charts.
At best, while using only standard CPAP or BiLevel, I suspect Bev will slowly and partially acclimate to pressure, while being pestered by outstanding RDI causing EDS and poor daytime cognition:
The manufacturer suggests that the BiPAP autoSV can address complicated breathing patterns:ozij wrote:As I said, I don't understand the SV, and why it was suggested.
One of those targeted phenotypes is complex sleep apnea (CompSA/CSDB), which Bev shows some indicators for. One indicator of CompSA/CSDB is the inability of the clinician to reduce sustained AHI below 5 with CPAP. Let's review Bev's CPAP titration:Respironics wrote:The device is designed to treat complicated breathing patterns. Complicated breathing patterns are mixed breathing patterns with OSA, Central, Mixed/Complex Sleep apneas and periodic breathing components
Another CompSA/CSDB indicator is the emergence of a central component when placed on CPAP, BiLevel, or APAP. If there's any central component above, it would be only slight irregular or periodic breathing. But during Bev's BiLevel titration, she very clearly met both CompSA/CSDB indicators mentioned thus far:CPAP Titration Chart:
0 cm = 14.9 AHI (@152.6 min)
5 cm = 20.0 AHI (@12.0 min)
7 cm = 10.9 AHI (@38.5 min)
9 cm = 0.0 AHI (@13.5 min)
11 cm = 12.2 AHI (@39.5 min)
13 cm = 7.6 AHI (@39.7 min)
14 cm = 4.7 AHI (@12.9 min)
15 cm = 11.7 AHI (@25.7 min)
16 cm = 31.3 AHI (@40.2 min)
17 cm = 21.3 AHI (@25.4 min)
18 cm = 60.0 AHI (@4.0 min)
19 cm = 4.5 AHI (@13.4 min)
----------------------------
(note: no central or mixed apneas above; central hypopnea emergence is unknown)
In my opinion, Bev's starting to look like a pretty good candidate for irregular breathing. She did score Periodic Breathing given the scoring criteria of the BiPAP AutoSV. And there are other physiologic presentations that very strongly hint at machine-induced dysregulation:BiLevel Titration Chart:
------------------------
12/8 cm = 29.8 AHI (@ 38.2 min) w/emergent CSA @ 68% or more*
14/10 cm = 18.6 AHI (@ 51.5 min) w/emergent CSA @ 19% or more*
16/12 cm = 6.3 AHI (@ 28.6 min) 3/3 events undifferentiated hypopneas
17/13 cm = 41.4 AHI (@ 23.2 min) w/emergent CSA @ 6% or more*
18/14 cm = 25.3 AHI (@ 52.2 min) 11/22 events undifferentiated hypopneas
19/15 cm = 29.3 AHI (@ 4.1 min)
20/16 cm = 8.8 AHI (@ 75.0 min) w/emergent mixed/CSA @ 27%
21/17 cm = 24.0 AHI (@ 7.5 min)
22/18 cm = 35.9 AHI (@ 21.7 min) w/emergent mixed/CSA @ 15% or more*
23/19 cm = 6.6 AHI (@ 63.9 min) w/emergent CSA@ 14% or more*
24/20 cm = 13.4 AHI (@ 94.3 min) w/emergent CSA@ 19% or more*
25/21 cm = 25.5 AHI (@ 30.6 min) w/emergent CSA@ 15%
--------------------------------
(*note: all hypopneas undifferentiated as central/obstructive; central hypopnea emergence unknown)
This AHI trend in particular is extremely interesting IMO. With no CPAP Bev will experience an AHI of somewhere on the order of 15 or 20 (only 15 during the beginning of her titration study). However, with some transient (leaky) pressure Bev's AHI will spike as high as 28 to 38. Sure can't explain that hard collapsing trend in sensor skew measurement error, servo-motor lag, or even airway-collapse related physics that I am aware of. When the machine goes into an LL state then maybe. But that's not the case here. I think that hard AHI spike is much better accounted for somewhere in stimulus/response driven physiology. Some pressure should keep the airway open better than no pressure. But in Bev's case the wrong pressure stimuli can be biologically much worse than no pressure.ozij wrote:Your pre cpap AHI was 20 - that was on you sleep study...
Your AHI ranged from 28 to 38 on fixed pressure, when you had leak problems
Do I think that Bev's titration charts above are describing problems with flow limitations? Flow limitation scoring is not included in those PSG charts. But I don't believe Bev's proven erratic tendencies for much harder Apnea and Hypopnea closures can be explained by tiny, perhaps even barely measurable flow limitation closures. If nearly imperceptible airway closures are the cause for all those much larger airway closures, we're on to.... chaos and bifurcation of all things! And a yet another proposed sleep disordered phenotype.
If we can fix all those symptoms in Bev's pathophysiology by bumping pressure to eliminate marginal flow limitations, then I'm kind of thinking that treatment trend would have been previously discernible by both the medical and patient communities. There's no doubt in my mind that UARS pathology can be mitigated by simply removing flow limitations, but I think that strategy cannot fix the hard Apnea and Hypopnea pressure-associated disorder we see on those titration charts.
At best, while using only standard CPAP or BiLevel, I suspect Bev will slowly and partially acclimate to pressure, while being pestered by outstanding RDI causing EDS and poor daytime cognition:
The Resmed ASV's EEP described above is the equivalent of EPAP on the Respironics AutoSV machine. Getting that EPAP up to 14 cm may be a good thing for Bev regarding RDI unrelated to A and H. It may help her aerophagia as well, since the instantaneous pressure travel from EPAP to IPAP peak will actually be less. Eventually I hope that Bev can go in for a proper AutoSV titration---but by experienced technicians:Stephen E. Brown, MD, DABSM wrote:Initially, we were hesitant to increase the EEP too rapidly; with experience, we have become more aggressive with our titrations...In another patient, undertitration occurred as the technologist adjusted the EEP for apneas and hypopneas, but did not adequately increase the pressure for residual RERAs. Our experience suggests that some of the early failures with ASV may be inadequate SDC/technologist experience, and not necessarily a problem with the device.
Stephen E. Brown, MD, DABSM wrote:There is a learning curve for the technologists. For the routine patient, the titration is extremely simple. However, extra skill and experience are required for some of the more difficult patients. Based on our experience, we suggest that initially only a small core group of a SDC's most experienced technologists become involved with ASV.... Our experience suggests that some of the early failures with ASV may be inadequate SDC/technologist experience, and not necessarily a problem with the device.
Last edited by -SWS on Wed Oct 22, 2008 2:50 pm, edited 3 times in total.
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Re: Why doesn't APAP respond to apneas?
Thank you, -SWS, for consolidating a lot of the info from Bev's sleep studies, too. And for your thoughts regarding the complicated puzzle her SDB (sleep disordered breathing) presents -- not only to the health professionals trying to figure out what she's got (or as we might say in the South.."what all she's got ) but also how, in the meantime, to treat "whatever it might be."
Pssst, Bev.... good thing you've got a sense of humor, and the determination and intelligence to keep working at it. We tend to talk about you at times like you're not even here, don't we?
Pssst, Bev.... good thing you've got a sense of humor, and the determination and intelligence to keep working at it. We tend to talk about you at times like you're not even here, don't we?
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Re: Why doesn't APAP respond to apneas?
I need to work on that. I envision that we're all huddled together in supportive analysis and conversation---happily putting our heads together trying to help Bev. So the whole exercise is all about Bev and all for Bev in my view. But some of that conversation will go back and forth in response to specific comments.rested gal wrote:We tend to talk about you at times like you're not even here, don't we?
Ozij didn't understand the rationale for suggesting BiPAP AutoSV. While I don't expect everyone to agree with it, I was hoping to shed a little more light on the rationale. I realize that Bev's AHI eventually stabilized at APAP 14-17 cm at home. The pressure response actually looks similar to CPAP at 14 cm, take away those chairs that don't solve anything.
On that basis I might even be curious to see what "CPAP@14 + SV" mode might eventually do for Bev if she can also better acclimate to BiLevel. So that statement is me talking to Bev and all. Because we sure have plenty of great people with great ideas involved in this thread of Bev's.
Re: Why doesn't APAP respond to apneas?
And plenty more of us hanging on to every word each of you has written... By the way thanks to DSM and Ozij and -SWS for the summary posts. It really helped me understand the whole discussion much better. Especially all those acronyms that were getting thrown around (PB? You mean PB&J? )-SWS wrote:...
So that statement is me talking to Bev and all. Because we sure have plenty of great people with great ideas involved in this thread of Bev's.
I'm learning so much from all of you! Thank you
And still keeping my fingers crossed for you Bev - hope it all goes better!
PR System One APAP, 10cm
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Re: Why doesn't APAP respond to apneas?
I still don't get it.
I don't understand why you consider the titration charts more meaningful that her results when sleeping at home on APAP. How do you explain the fact that Bev's AHI is lower when she raises the auto pressure?
What does it mean, that the APAP machine can and does reduce her AHI to less than 5? Is that - at all - possible in cases of CompSA/CSDB? It was my impression that CompSA/CSDB is diagnosed based on the response to treatment, not to titration.
If normal breathing can be dysregulated by machines, then how can the Bev's dysregulation on the SV prove anything?
O.
I don't understand why you consider the titration charts more meaningful that her results when sleeping at home on APAP. How do you explain the fact that Bev's AHI is lower when she raises the auto pressure?
What does it mean, that the APAP machine can and does reduce her AHI to less than 5? Is that - at all - possible in cases of CompSA/CSDB? It was my impression that CompSA/CSDB is diagnosed based on the response to treatment, not to titration.
If normal breathing can be dysregulated by machines, then how can the Bev's dysregulation on the SV prove anything?
O.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Re: Why doesn't APAP respond to apneas?
Poor Bev, this is like MASH, she's laying there trying to get some sleep and we all walk by and grab her chart, she must think her cot is next to the chow line-SWS wrote:I need to work on that. I envision that we're all huddled together in supportive analysis and conversation---happily putting our heads together trying to help Bev. So the whole exercise is all about Bev and all for Bev in my view. But some of that conversation will go back and forth in response to specific comments.rested gal wrote:We tend to talk about you at times like you're not even here, don't we?
Ozij didn't understand the rationale for suggesting BiPAP AutoSV. While I don't expect everyone to agree with it, I was hoping to shed a little more light on the rationale. I realize that Bev's AHI eventually stabilized at APAP 14-17 cm at home. The pressure response actually looks similar to CPAP at 14 cm, take away those chairs that don't solve anything.
On that basis I might even be curious to see what "CPAP@14 + SV" mode might eventually do for Bev if she can also better acclimate to BiLevel. So that statement is me talking to Bev and all. Because we sure have plenty of great people with great ideas involved in this thread of Bev's.
But I too would like to see that, I don't see CPAP@14 +SV being much different than Auto @14 cm. The major difference with SV over what she has tried in the past is the variable Pressure Support. In her other titrations that has always been static. PB wasn't seen until her 2nd night on the SV. I really don't think those chair pressure responses are anything of concern on her Auto report, I have seen them many times including on my own. I understand them to be the "circuit" the machine uses when no other event or circuit has control over the machine. When an apnea or hypopnea is seen control is handed to the A/H control circuit. When a FL is seen it is handed over to FL circuit, when Snore is detected it is handed over to the Snore circuit. When it has nothing to do it puts those little chairs up and has a seat for a while You will notice when a event puts up a tic they go away. What it does it increase pressure, waits, increases again and then drops looking for something as the pressure falls, if it sees anything it should respond to it hands it over to that circuit. Maybe its part of digital autotrac I don't know. I've read about it doing that for years and there was even a comment about it in one of the trade journals magazines about it. Actually, I think it happens every 15 minutes or so.
If you put her EPAP=14, that is the same as AFlex at 14, if you put her IPAP Max 4 higher at 18 cm. Then PS of 4 cm will be provided, I don't think that is enough to trigger any kind of PB. Her doctor really wants to see her lower, he suggested too low in my opinion with 4 cm, I'd never go that low, 6.5 is the lowest I'd try. Maybe he wants her that low to see what she does rebreathing more of her CO2, would be my guess.
Obviously the AFLEX @14 produces the best AHI but we all know that doesn't mean best quality sleep once you get there. We have to get her into more REM in my opinion. Long sleep sessions >9 hrs, still waking up tired, that says too much deep sleep to me and not enough REM. IF she was getting the quality sleep she needed, she would be waking sooner and in REM, remembering dreams good or bad. I know I get decent dreams late in the morning, I know I should be waking but man it is just too much fun staying in that dream.
So why should she continue trying the SV? Curiosity if we could possibly get PS up she may land into REM. If she is not getting any REM now, she is getting way too much SWS, that would coincide with the long sleep sessions.
I wish we had a snapshot of her current sleep architecture.
http://www.dreamviews.com/sleepstages.php
I don't know about you guys, but when I awaken from REM and a dream I feel great. Wake up in Stage3 or 4, and I feel like crap, the other day I woke up in deep sleep, removed my mask, looked at it and it had air coming out, wondered to myself what the heck was that doing on my face, COULDN'T figure out how to turn it off so I just set the mask down on top of the machine and went to the bathroom. When I wake up from deep sleep, I have no idea where I am or what I'm doing. When I come back from the bathroom, oh yeah the On/Off button stops that air and noise. Being in a stupor is the best way I can describe it.
someday science will catch up to what I'm saying...
Re: Why doesn't APAP respond to apneas?
I think Bev's EDS may be caused by those consant little pressure challenges from the Respironic, or by the Lexapro or both.
O.
O.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Re: Why doesn't APAP respond to apneas?
ozij wrote:I think Bev's EDS may be caused by those consant little pressure challenges from the Respironic, or by the Lexapro or both.
O.
FYI: She is NO longer on Lexapro, that has been mentioned several times now.
someday science will catch up to what I'm saying...
Re: Why doesn't APAP respond to apneas?
Ozij,ozij wrote:I still don't get it.
I don't understand why you consider the titration charts more meaningful that her results when sleeping at home on APAP. How do you explain the fact that Bev's AHI is lower when she raises the auto pressure?
What does it mean, that the APAP machine can and does reduce her AHI to less than 5? Is that - at all - possible in cases of CompSA/CSDB? It was my impression that CompSA/CSDB is diagnosed based on the response to treatment, not to titration.
If normal breathing can be dysregulated by machines, then how can the Bev's dysregulation on the SV prove anything?
O.
My understanding is that once on the SV we were able to see data that the APAP wasn't providing. The SV data shows 3 very important sets of data and other supporting data.
1) Erratic breathing rate (cpap-apap data would not show the extent of this)
2) Fluctuating volume (periodic breathing) the cpap-apap would not show this)
3) The extent the machine was driving Bev's breathing - Patient TRiggered Breaths graph (related to point 1)
Supporting data was ...
a) The time the macgine spent at IpapMax (indicating some secondary problems)
b) The AI HI & PB scoring
c) Bev's av peak flow & tidal volumes
Bev is a special case & her titration is clearly an exercise for a very experienced RT doctor. A CPAP / APAP bascially would have masked the data we got off the SV so without Bev having used it we would be a lot further away from where we are today in honing in on what is best for her. SWS has demonstrated yet again his extraordinary insights by honing in on the bifurication aspect so quickly (bifurication being that Bev showed on the SV that she goes from normal stable respiration to erratic respiration regularly). The neurological component was another line SWS & others honed in on early. The questions re narcolepsy & its lesser variants proved very informative when Bev explained her family history.
To some extent the SV appeared to be doing its job but the data we get from the SV reports is not granular enough for us to look at exactly what the PS was doing at any given instant (say a 16 min window expanded out so the we see the actually pressure rises and falls very clearly across a page). But Bev's headaches were indicative of the therapy not working the right way, i.e. the machine appeared to be mechanically sorting Bev out but not in a way that gave her a good day afterwards.
Cheers
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)











