AfibApnea wrote:A few details:
I don’t remember (I can assume I was sleeping) the 2230 to 0215 segment. (I must’ve woken, and turned the machine off at around 23:45, probably for a bathroom break.)
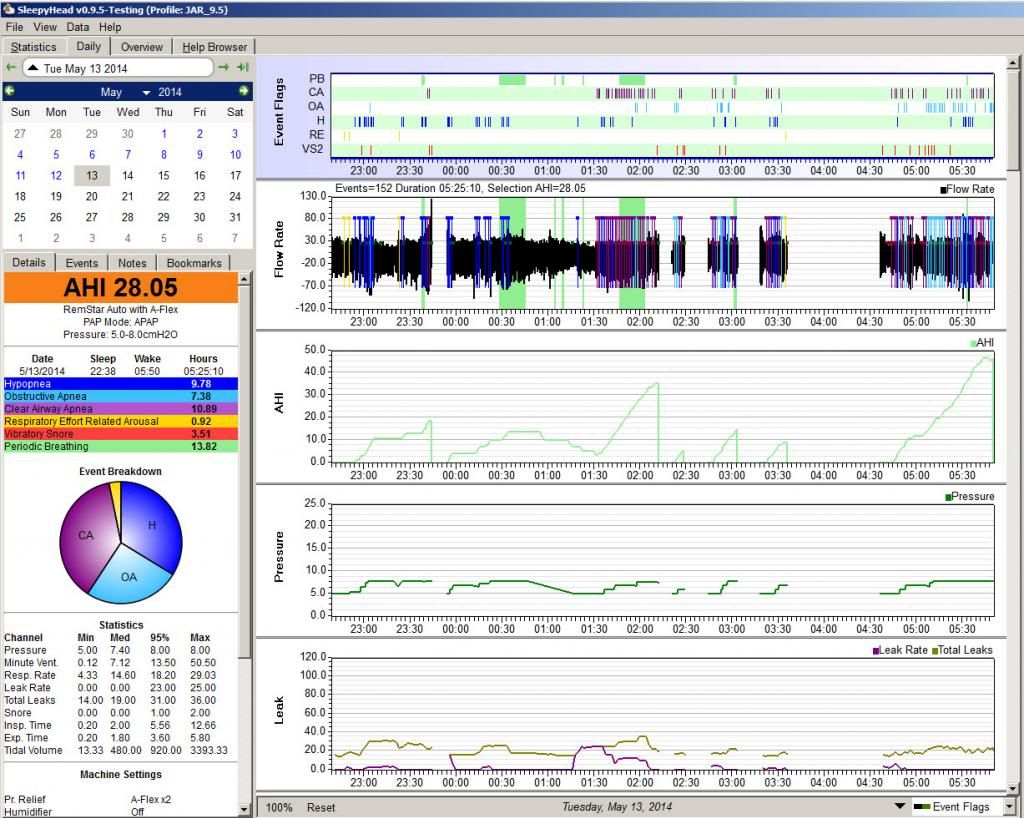
So there's a good chance that the excessively large number of CAs scored between 1:30 and 2:00 AND the PB scored during 0:30-0:45 and 1:45-2:00 are the REAL thing. And because the PB is likely really there, some or all of those Hs scored between 0:15-0:40 may be
central rather than
obstructive. There's no way to tell which they are from the CPAP data; that really requires the data gathered in a full in-lab PSG study. The data from 22:30 to 2:15 is still strong enough to support your doc's idea that you may be dealing with emergent central apnea of some sort.
At around 2:15 I got up fairly frequently (for some reason I always think a lot more time has gone by) and did little more than (turn the machine off and) just sit by the side of the bed waiting for my nasal passages to clear (this is not the type of thing that required blowing my nose or the equivalent).
So some of the stuff going on between 2:15 and 4:30 may be sleep/wake/junk---i.e. irregular wake breathing patterns mixed in and getting misscored by the machine as OAs, Hs, and CAs. But it could also be the case that every time you started to drift off to sleep, your breathing became unstable and the CAs started to emerge. Only an in-lab sleep test can really distinguish between sleep/wake/junk and clinically significant problems with transitional central apneas.
From 0330 to 0430 I got up, went downstairs and read.
So the gap in the data is easily explained.
From 0430 to 0545 I did not get up. Instead I breathed as well as I could, often compensating nasal breathing with: nasal-in/mouth-out. It’s hard to explain why my body uses this strategy.
Again though the question is
how much sleep did you get during this time? And I don't mean your
impression of how much sleep---I know you think you were awake the entire time.
But just like we don't remember short wakes when we're sleeping well, we also don't remember short sleeps when we're lying in bed fighting to get back to sleep. And so again the question becomes teasing out sleep/wake/junk patterns that don't mean anything from transition to sleep problems that DO mean something significant.
That said, let's look at what you're describing as your breathing pattern:
Instead I breathed as well as I could, often compensating nasal breathing with: nasal-in/mouth-out. It’s hard to explain why my body uses this strategy.
- - One reason seems to be that it is much harder to breath out against the air pressure;
- Second reason: it’s a reset mechanism. Breathing out through the mouth seems to restore some sort of pressure-balance through which it is easier both to breathe in and breathe out.
What you are describing is call "exhalation puffs" and they're actually recorded on either the F&P or Devillbass PAPs as I recall. But they can also be described as "Pursed Lip Breathing" that is commonly used by people with COPD (in the daytime as well as at night).
Exhalation puffs are
often considered a potential problem for getting CPAP therapy optimized.
Part of this is that when your are exhaling through your mouth there's a chance that you are losing therapeutic pressure. (Although at your pressure range, that's not likely to be as big of a problem as it would be for someone using a higher pressure setting.
Another reason that exhalation puffs can be problematic is that they can confuse the machine about the breathing pattern, leading to the scoring of false events. (And also occasionally making it easier for a machine to
miss scoring a real event.)
Exhalation puffs would also explain
why you notice the exhaust flow so much more on your inhalations rather than your exhalations: When you are exhaling through your mouth, much (perhaps most) of the venting is being done through your mouth and NOT through the exhaust vents. But as soon as you close the mouth at the start of the inhalation, all the venting from the system is once again through the mask's exhaust vents. So of course it's much more noticeable.
Since you are doing a lot of exhalation puff breathing, the bigger issue that has to be addressed is:
Why are you finding it so much more difficult to exhale through your nose? You may think it's just "congestion". But given the afib, I beginning to wonder if there isn't something more to this. Are you ever short of breath during the daytime? Do you ever do the exhale puffs when you are NOT trying to use the CPAP? Do you do a lot of chest breathing? Or are you mainly a diaphragmatic breather?
You could try increasing the Flex from 2 to 3: That will provide a bit more exhalation relief pressure at the beginning of the exhalation, which should make it easier to exhale. But if switching from Flex = 2 to Flex = 3 makes the problem WORSE rather than better, then there's a chance that part of what's driving your discomfort on exhalation is the fact that the PR System One's Flex system
starts to increase the pressure before the end of the exhalation. And in some super sensitive folks (like me) that subtle increase in the pressure
during the second half of the exhalation can make it feel as though it is very diffiult to fully exhale against the machine. And in that case? Turning Flex off completely make make it easier to exhale.
But the long term solution to the exhalation problem may be a switch to a different machine. Both a BiPAP and ASV will have two distinct pressures: One for inhalations (IPAP) and one for exhalations (EPAP). And the machine can be set up so that there is NO pressure increase until the beginning of the inhalation is detected (in "spontaneous" mode) OR when an ASV machine decides that it needs to start "triggering" inhalations because your breathing pattern is unstable and you are at high risk of having a cluster of CAs get started.
Does this explanation explain anything or cause you to change the way you read the data?
Not really.
I'm willing to consider the data collected AFTER 2:15 as possibly having significant sleep/wave/junk patterns, but that does NOT explain the data collected between 22:30 and 2:15, when you don't remember any serious restlessness. And the data between 0:15 and 2:15 is pretty troubling and has way too many CAs for me to be comfortable saying that it's ok to ignore the possibility of CompSA or CSA being a issue.
And
given your history of afib and the fact that your sleep doc has good reasons to worry about the possibility of CompSA or CSA, I'm inclined to think that this stuff needs to be properly investigated in an in-lab sleep test, even though that's not a comfortable thing to deal with.
Out of curiosity, could you post a more typical night's data---one where you don't remember being awake for most of the night???