Greetings! If you don't mind, I'll jump into this conversation. First, I would like to point out some observations I made while looking at your data.
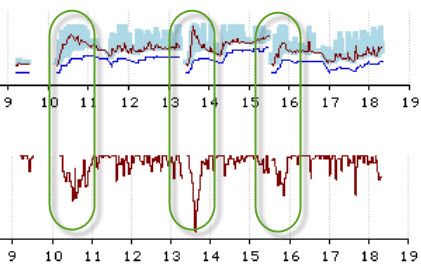
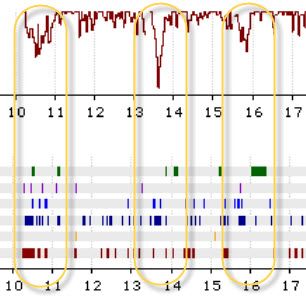
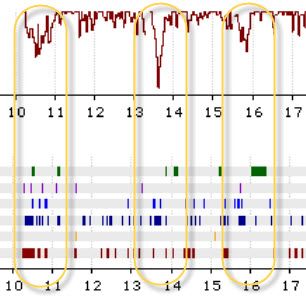
First of all, you, my friend, also suffer from pretty bad central apneas as you fall asleep. You can see that in the following graph. This shows that as you fall asleep your various scores also jump up in number. In fact, from looking at the scores over several nights it appears as if the obstructive apneas tend to trigger the central apneas. That is often the case. The lack of oxygen creates a swing back and forth in your respiration from hyper- to hypo- ventilation. And central apneas often result from the hyper-ventilation.
A little bit of an education is in order. During the hyperventilation your body blows off too much CO2, which your body measures by measuring the acidity of your blood. The acidity of the blood drives ventilation. If it becomes too acidic your body will breathe more rapidly to blow off the CO2. If it becomes to base (not acidic) then your respiratory drive decreases until the acidity climbs. This depression of the respiratory drive can cause the central sleep apnea.
As you can see your "Patient Triggered Breathing" falls as you fall asleep.
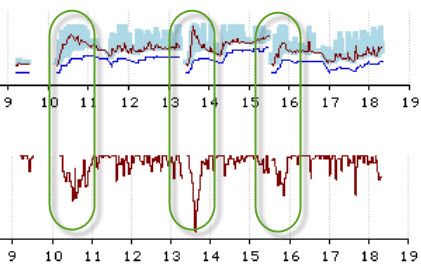
That leads to an increase in obstructive apneas and hypopneas during the same time period. Since these seem to proceed the central apneas, it would be wise to address the obstructive apneas and hypopneas.
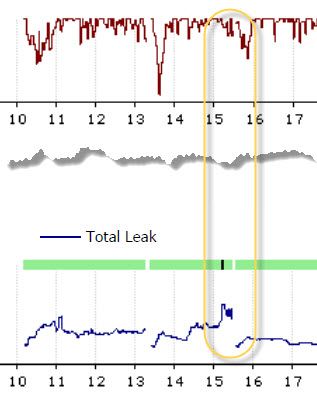
Sometimes leaks seem to trigger the wakeup. You might find mask liners helpful with an ASV unit. You can find mask liners at the following websites:
http://www.remzzzs.com/
http://padacheek.com/
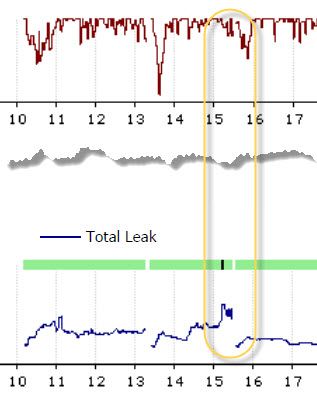
Finally, when we compare your Breaths Per Minute (BPM), you can see another confirmation of this correlation.

So, what to do about this? Well, you are on the correct path. Too often the sleep centers just leave the units "wide open" to allow them to dynamically address the problem. However, this can allow those obstructive apneas and hypopneas to make matters worse. You are doing the right thing. Gradually adjust your Minimum EPAP and Pressure Support. Since it's now at 5.5, I would wait another week before making further changes.
Why wait such a long time? Well, one day a trend does not make! There are several things you need to consider. First, it takes MONTHS before your body fully adjusts to the ASV therapy. It's not at all normal to have the pressure changing all over the place. However, as your body adjusts the AHI will naturally fall .. because your body is learning to use the ASV therapy as a reminder to breathe regularly and effectively.
Second, you need several days to really be able to see if you have a good trend. If at the end of the week your AHI remains above 5 then you should increase the Minimum EPAP by 0.5 (and no change to PS .. a PS of 4 is a fairly common separation between EPAP and IPAP).
Third, don't forget to let your doctor know the changes you've made. And show him the graphs so he can see that you are using the machine data to help guide the adjustments.
Hope that helps.