Jay Aitchsee wrote:Avi, I've found the hardest part of my lab to "sync" is the pulse-oximeter, since it doesn't have real clock. What I do is try to create artifacts at known times, like put it on and take it off, so i can align it with the rest of the data. Fortunately, desats are not a major problem for me, so I don't wear it too often. I, too, suffer from fragmented sleep and lack of deep sleep. What I've been able to determine is that my sleep disturbances are not caused by REM - which is good since I understand that's the hardest to overcome. I'm also pretty sure my sleep is not being significantly interupted by apneas since my AI is usually down around 0.5 or less. That leaves pain and/or PLMD and my sleep Dr and I are are trying different meds to see if we can improve my sleep. I've just started on a new med and my apneas and awakenings are higher than normal which is not uncommon when I start a new therapy. So we'll give it a couple weeks and see how it develops. I am lucky to have found a Dr who encourages my participation in my own treatment. She treats the results of my "home sleep lab" with respect and we use them, in part, to determine the efficacy of treatment.
I'm not sure why you don't submit to a PSG to resolve some of the issues you are having. Is it because it's uncomfortable to go, or do you think the results would not be the same as at home? I don't know what medicare rules are, but I've had 3 in about 5 years. So, depending on your last, it's likely they would pay for another. It does sound as if something with a full EEG would be helpful in determining the cause of your fragmentation.
I would think you could get your AI under control with your S9 and ResScan. But, as I think you have said many times, that alone may not resolve all your sleep issues. I think many of us suffer from more than one type of sleep disturbance simultaneously and all we can do is tackle them one at a time. And that is precisely why I started to put together my own "lab".
Jay
I'm not sure why you don't submit to a PSG to resolve some of the issues you are having ?.
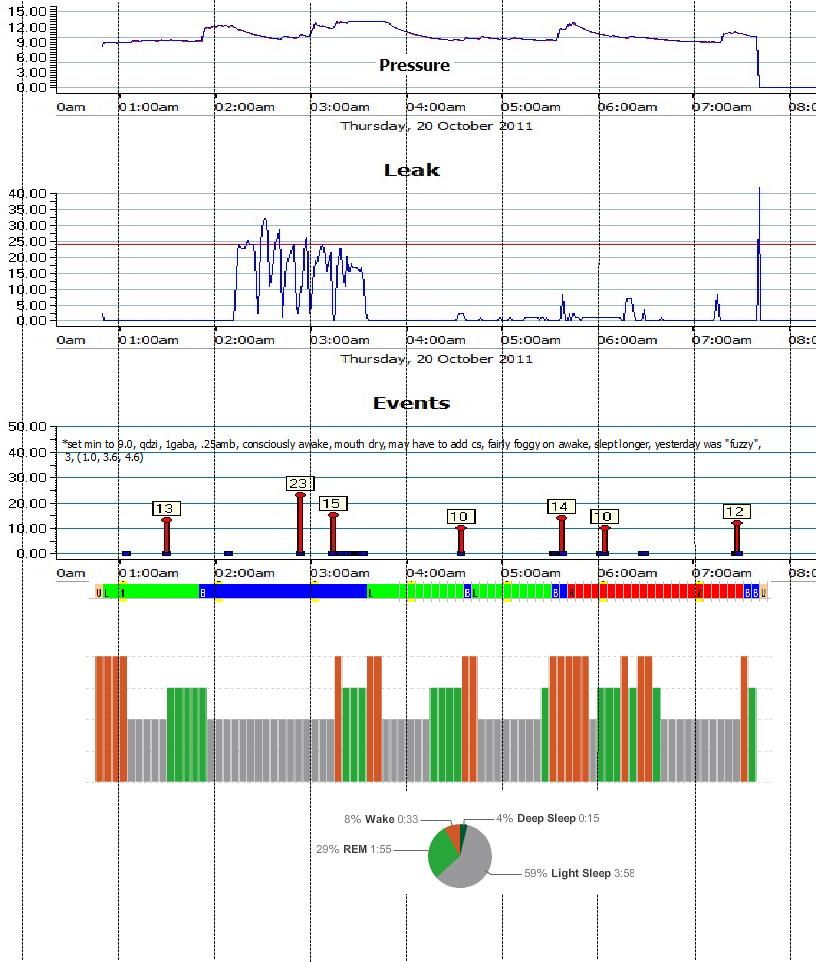
reply to jay (only): Because I don't trust the technicians in the clinic that I used before. See here that about a year ago the effective titration result for me was for 6 cmH2O, however when I titrated my self to find out if I could get better results, see what happened:
There are better results at diff pressures:


So to carry out a new PSG I need to look for another place. But I do like my current
sleep MD who partially owns this
sleep clinic.
Also, if I could avoid doing PSG, often, why not find a In Home system which would indicate vital signs of wrong treatment and cost a lot cheaper?
p.s. Jay, looking at your graphs I don't see anything wrong and your events are miniscule. IMO, your
sleep fragmentation comes from some underying medical conditions which are not related to respiration or
sleep architecture. How about Diabetes, Depression, hi Epworth sleepiness score, alcohol, smoking, •Neurologic syndromes, etc.?
Or any of these causes:
This discussion includes the differentiation of various central
sleep apnea syndromes from one another. Central
sleep apnea in various forms can be seen in the following conditions or events:
•
Cheyne Stokes breathing-central
sleep apnea: CSB-CSA is characterized by classic a crescendo-decrescendo pattern that typically occurs with a periodicity of 45 second or greater cycles (see image below). The ICSD-2[2] specifies that at least 10 central apneas and hypopneas per hour of
sleep should occur, accompanied by arousals and derangement of
sleep structure. The arousals occur at the peak of the hyperpnea phase. Patients usually have predisposing factors such as heart failure, stroke, or renal failure, as well as a lower resting PaCO2 than normal.
◦Heart failure
◦Stroke
◦Renal failureCheyne Stokes: This polysomnogram represents Cheyne Stokes breathing and occurred subsequent to continuous positive airway pressure titration for OSA in the same patient in the previous media file. Cheyne Stokes breathing has a classic crescendo-decrescendo breathing pattern.
•
Central
sleep apnea due to a medical condition: The patient has a history of an underlying disorder other than heart failure or renal failure. Patients with stroke can have either classic CSB-CSA or central apneas without a crescendo-decrescendo pattern. ◦Stroke
◦Diabetes mellitus
◦Hypothyroidism
◦Parkinson disease
◦Multiple system atrophy or Shy-Dragger syndrome
◦Familial dysautonomia
◦Postpolio syndrome
◦Damage to medullary respiratory centers by tumor, infarction, or infection
◦Arnold-Chiari malformation types I-III
◦Cervical cordotomy
◦Muscular dystrophy
◦Myasthenia gravis
◦Prader-Willi syndrome
◦Idiopathic cardiomyopathy
◦Acromegaly
•
High-altitude periodic breathing: The single most important feature is that high-altitude periodic breathing occurs only with recent ascent to high altitudes. Many patients develop this at an altitude of 5000 meters or greater, while almost everyone develops it at an elevation of 7600 meters. The cycle length is shorter than in CSB-CSA, 12-34 seconds.
•
Use of opiates and other CNS depressants: This is most easily recognized by a history of opiate use. Wang et al[6] demonstrated that 30% of participants in a stable methadone maintenance program had a central apnea index (CAI) of greater than 5 and 20% had a CAI of greater than 10. Methadone blood concentration was significantly associated with the severity of central
sleep apnea.
•
Primary central
sleep apnea: This is an uncommon condition in which 5 or more central apneas, lasting 10 seconds or more, occur per hour of
sleep. Patients have a low-normal PaCO2. The central apneas terminate abruptly with a large breath and without associated hypoxemia. They do not have a crescendo-decrescendo pattern of breathing
•
Complex
sleep apnea: Central
sleep apnea may emerge during titration of CPAP in patients previously diagnosed with obstructive
sleep apnea. This syndrome, termed complex
sleep apnea, has become a controversial topic in the
sleep literature[17] and has been raised as a possible type of difficult-to-treat obstructive
sleep apnea. As many as 6.5% of patients with obstructive
sleep apnea may develop emergent or persistent central
sleep apnea with CPAP treatment. CPAP emergent central
sleep apnea is generally transitory and is eliminated after 8 weeks of CPAP therapy. Persistent CPAP-related central
sleep apnea has been observed in approximately 1.5% of treated patients.[18] Similarly, complex
sleep apnea can occur following a tracheostomy for obstructive
sleep apnea. Central apneas have been found initially after a tracheostomy, but after an extended period, central
sleep apnea decreased on repeat PSG.[19]
•
Physiologically normal apneic events ◦Central
sleep apnea during
sleep-wake transition: Up to 40% of healthy individuals may exhibit central apneas during
sleep-wake transition. The central apneas occur during the period that chemoreceptors are resetting and instability of ventilation control occurs. They are usually brief and not associated with significant oxygen desaturation. The clinical significance of this entity is unknown. Once stable
sleep is reached, normal individuals should not have more than 5 central apneas per hour of
sleep.
◦Postarousal central apnea or postsigh central apnea: During a PSG review, central apneas are commonly seen following an arousal or after a sigh and are usually inconsequential. They are thought to be a result of Herring-Breuer reflex or hypocapnia induced by hyperventilation caused by a sigh or arousal.
Lets hope that there is none of the above.