Re: ASV: AHI still high, suggestions?
Posted: Fri May 13, 2011 9:26 am
del
See, this is where I feel like we diverge a little bit. You said you felt better -- I feel worse. Not "awful OMG terrible" worse, like I did on the BiPAP S/T where I felt like I was in a fog all day, but definitely just more drained and depleted. It's not so much feeling tired. And on the nights when I'm managing around 9 hours, I certainly don't feel great either.Mr Bill wrote:I felt better but I remarked to my friends that now that I was getting some sleep I actually was starting to feel lack of sleep! I'm up to a little over 6 hours a night average. I just can't seem to stay asleep most nights much longer than that. But the nights I have slept 8-9 hours; Oh man! Its wonderful, my mind is so clear and sharp!
We're probably talking past each other a bit here, but the things I've read are like http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2576323/. If the existence or onset of centrals is 100% iatrogenic in nature, then as this article alludes, the CompSA *is* the disease itself.avi123 wrote:Brian, if you really have Complex Sleep Apnea Syndrom then, I keep reading that there are other issues to deal with besides the ASV machine settings.
My emphasis.BiPAP autoSV Advanced has at its core the clinically-proven 1, 2 REMstar Auto algorithm. Utilizing a blend of advanced Respironics technologies (Digital Auto-Trak and REMstar Auto titration algorithm plus auto EPAP) the device is uniquely able to continually and effectively manage the patient's airway. Our proven servo ventilation algorithm then works to assure that with each and every breath, the patient is appropriately ventilated.
I am not surprised.BrianinTN wrote:I wouldn't say I'm sleeping very well, but the air pressure is a LOT less disruptive than it was on CPAP (13 cm) and BiPAP (20/16).
http://bipapautosvadvanced.respironics. ... otocol.pdf
*If pt has known CPAP pressure of
< 10 set EPAPmin at 4 cm H2O
or patient comfort
*If pt has known CPAP pressure of
> 10 set EPAPmin at 6-8 cm H2O
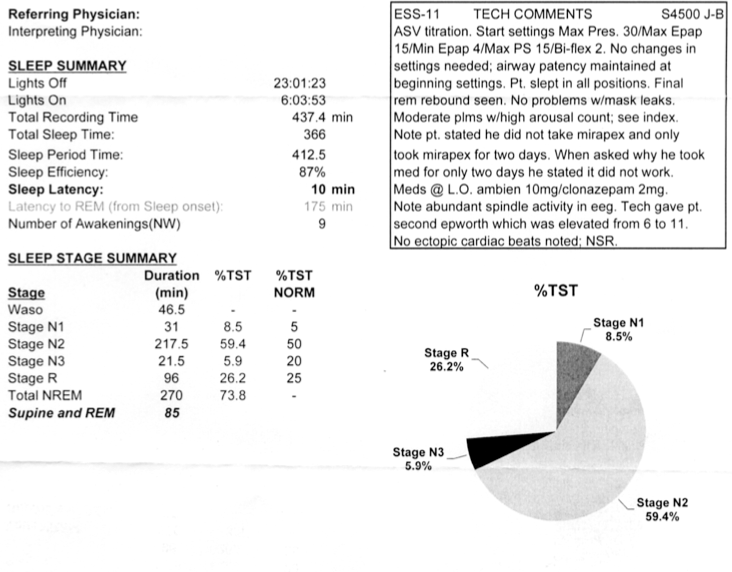
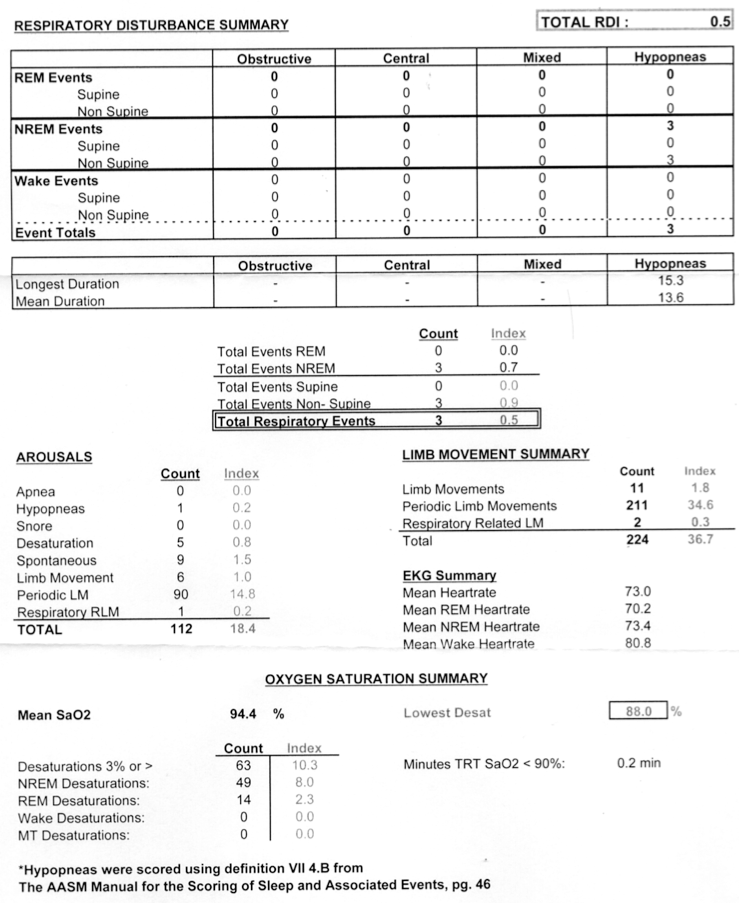
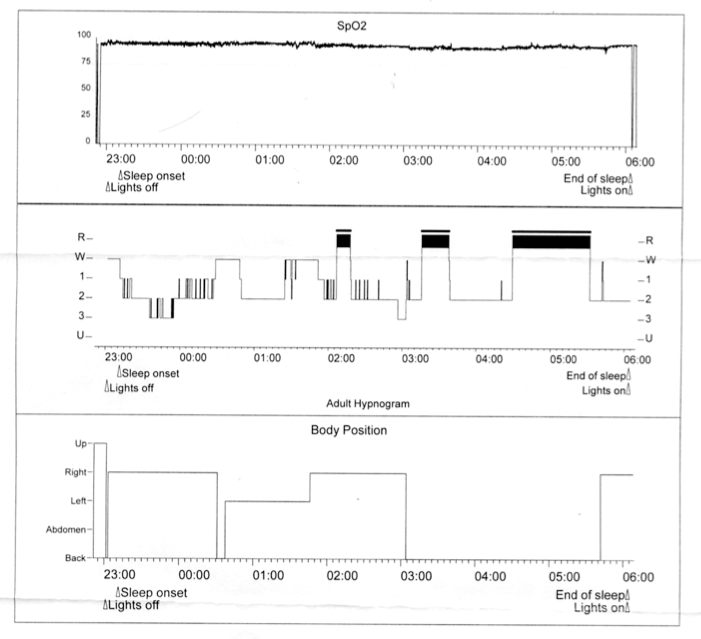
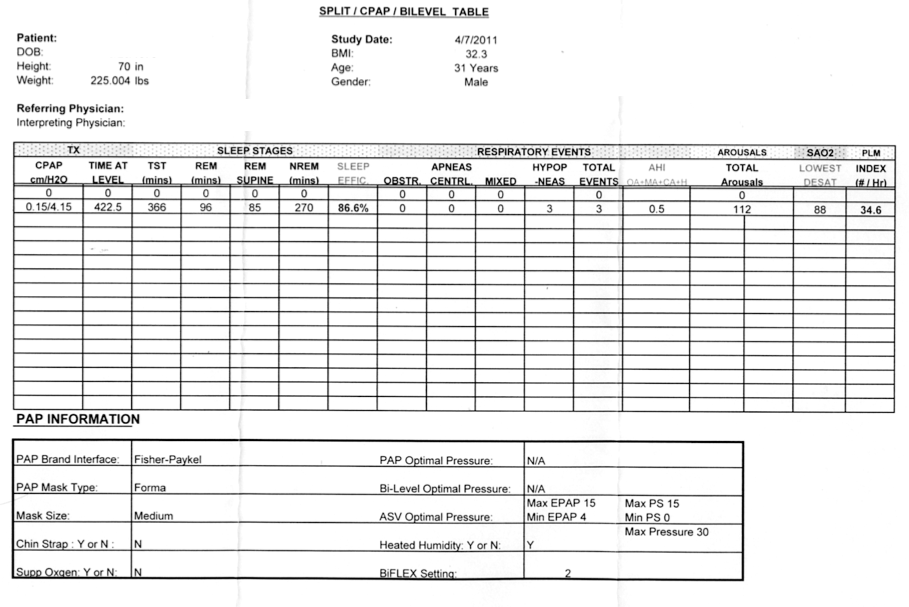
or patient comfortMy emphasis.BrianinTN wrote:ozij, the current settings for my machine are precisely those from the end of my titration. They left it basically in the same mode it comes out-of-the-box, and the clinician did not have to adjust a single setting throughout the entire night. He told me this, and I saw the sleep study which showed only a couple hypopneas throughout the night.
You have a known CPAP pressure of 13, a BIPAP of 20/16, they left you with an EPAP minimum of 4, they did not try you with an EPAP min of 6-8.
And with EPAP Min=4 your are having residual hypopneas and unsatisfactory therapy.
My problem is simply that my home results, despite matching those in-lab titration settings, are not coming out as good.
To continue with the 'matrix' (that you are already using) it would be helpull if you gave the results EPAP Min 4 and PS Min 1, 2, 3. Otherwise, your thread is just so much fodder (i.e. pig food). How would you like to proceed?BrianinTN wrote:I'm fully prepared to give it time; I've been at this for a year already. Mostly I'm just hoping to figure out some tweaks to make this work better for me, both in the short-run and the long-run.
As John said - it is always advisable to discuss details with you doctor.back in the beginning of the thread JohnBFisher wrote:Brian, I agree with avi123. It appears most of your AHI score is due to hypopneas. You probably should talk with your sleep doctor about this. It might be you need a slightly higher EPAP pressure to help keep your airway open. But as is true with anyone with an ASV unit, there is a lot to consider (such as, higher pressure can trigger more central apneas). In such cases, it is always advisable to discuss the details with your doctor.
StillAnotherGuess wrote:Throwing out the AHi 15 for the "additional 3 hours sleep", it would appear that a slight separation between EPAP and PS Min is already trending better for you. This would be consistant with the sleep communities expectation for bi-level therapy.BrianinTN wrote:It's been two days. I don't have all that data yet. I've tried PS=2 and the results are mixed (AHI of 4 on the first night of seven hours, 15 for additional three hours of sleep the next morning, and 4 last night for six hours). Subjectively, I've felt meh.
I was formerly a pretty active weightlifter until injuring my shoulder a year or so ago, so even the body weight is misleading.avi123 wrote:I can't find anything out of the ordinary in above PSG besides the BMI being on the hi side (obese), but I am not a Doc. Also, I can't see a reason for using an ASV. So I am out of here.
That article went on to note that there are two primary treatment methods (see the subsection titled "Management of CompSAS) -- BiPAP S/T, which did not work well in my case, and ASV, for which the jury is still out. I think your confusion may be stemming from the fact that the only PSG results I pasted in this thread were from my ASV titration, which was my fourth sleep study in the past year. There were three prior studies: the initial diagnostic study, which showed over 30 obstructive events per hour (which qualifies as moderate OSA); the CPAP titration, where centrals were emergent and frequent; and the BiPAP S/T titration, where the pressure of 20/16 appeared to control both the obstructive events and iatrogenic centrals in the couple hours of lab testing. Because my BiPAP S/T results at home were exceptionally poor both quantitatively (AHI around 35) and qualitatively (I felt like dung using it), I was sent in for an ASV titration. Hopefully that clears things up.While obstructive events respond well to continuous positive airway pressure (CPAP) therapy, the response of central events is often incomplete and not sustained over time. CPAP treatment of obstructive events can, itself, lead to the development of central sleep apneas (CSA) or a Cheyne-Stokes respiratory (CSR) pattern in some patients. This syndrome of obstructive events or mixed central and obstructive events with short cycles of obstruction, minimal disease in rapid eye movement sleep, and incomplete response to positive airway pressure (PAP) has been labeled “complex sleep apnea syndrome” (CompSAS)