Page 2 of 4
Re: What if you have mostly hypnopeas and not apneas?
Posted: Wed Dec 22, 2010 10:17 pm
by Cindy Lou Who
I consider myself a newbie. And see there is so much to learn. This is my experience. In two separate home studies by different providers, my hypopneas were 127/hr and 121/hr respectively. There was one Central and 8 Obstructions per hour on average. My O2 dropped to 83% and 82% respectively.
Prior to treatment I was depressed, had elevated blood pressure, short-term memory loss, was constantly irritated, prone to rage over the slightest thing, always exhausted no matter how much I slept, and struggled to perform at work. I made so many mistakes in December '09 that part of my work responsibilities were removed. I thought I had early-onset Alzheimer's. I was terrified I would get fired.
That motivated me to get the first home study. The in-hospital sleep lab was a disaster, and said I didn't have OSA. I requested a second home study as a 'tie breaker', and asked the Dr to give me an auto machine based on the 2 home studies. He wisely did!
Depression, memory loss, irritation, mood swings, rage, exhaustion... all gone. The ability to fully function, multitask and learn new things has returned with a clarity I have not known in years.
In conclusion, partial obstructions had a major impact on me.
Thank you RDawkinsPhDMPH and NotMuffy for your informative posts. And a big "Thank You" to the original poster for asking questions.
Cindy
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 11:16 am
by larry63
larry63 wrote:RDawkinsPhDMPH wrote:As stated, the definition of obstructive sleep apnea syndrome counts hypopneas equal with apneas. For reasons not worth the space here: for all intents and purposes a hypopnea is as bad for your health as an apnea. I even won a Medicare hearing on this back in the early nineties when Medicare didn't normally recognize hypopneas.
As for the O2, I totally disagree with your PCP that O2 is the primary determinant of the severity of your apnea. It is usually, in my opinion, an important secondary indicator of the severity. Just my humble opinion.
OK, good point about the O2 level. I can see where where frequent awakenings, for example, without and O2 drop, can cause health problems.
But excuse me, but part of my question implicitly asked if a hypnopnea is comparable to an apnea in terms of negative health consequences.
And your answer it is that it is is just as bad for you. But yet you state "for reasons not worth the space" you won't explain why.
So, I asked a question, and basically you didn't answer it, but just stated an unfounded opinion.
It if is not worth the space to answer on this forum, then please respond by PM, or better yet, simply post a link to to the relevant research papers.
Oh by the way, did you know that for reasons not worth the space here: the moon is made of chocolate? Unfortunately, there is not enough space here to explain the reasoning, so I trust you will take this as fact.
Best Regards
Wow, as someone else said, re-reading what I wrote, it sounds a bit combative, and I'm sorry. In person I would speak this way, but in email it somenohow
sounds more beligerent.
In any case, I already found one paper/study that asserts that hypnopeas are as bad as apneas. But there are different opinions.
So please don't go out of your way to dig up backing information - I should learn to web-search before I send replies like this. The problem is that
when I'm posting, I'm a little grumpy because I feel sleep deprived and hence tired and irratble even with CPAP and want to know why.
In any case, I am very greatful of how you and other people have been cutting me some slack. I will try to tone it done a bit (although I _will_ continue to ask for cites, hopefully in a more polite manner). One thing that Impresses me about this forum in fact, is that many posters do in fact post citations to back up their opinions. I've dealt with forums dealing with other diseases, and often people post just their own opinions with out any references to actual studies to back it up.
Thanks for r
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 11:30 am
by larry63
robysue wrote:larry63,
A quick question, if I may.
I believe that you mainly or only had hypopneas during your sleep study.
And you're now using an S9.
On a typical night, does the S9 record more hypopneas or more apneas?
In other words, is the AI higher or is the HI higher? If you only have the data off the LCD, the HI = AHI - AI.
Thanks,
robysue
Hi robysue - getting ready for a road trip so probably won't have time to look at resscan before monday or tuesday, but if I do find the time I will let you know.
I do now when I last looked at it there were a more centrals then during my dx sleep study. Total AHI is usually under 5 every night. I personally think that
I have more true awakenings (not just stage 2 to alpha for example) with CPAP, due to irritaion, sores, waking up every time I change position, rainout, etc,
and possibly that is causing me to feel worse with CPAP therapy.
Next week I well look at resscan and let you know.
~~larry
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 12:32 pm
by robysue
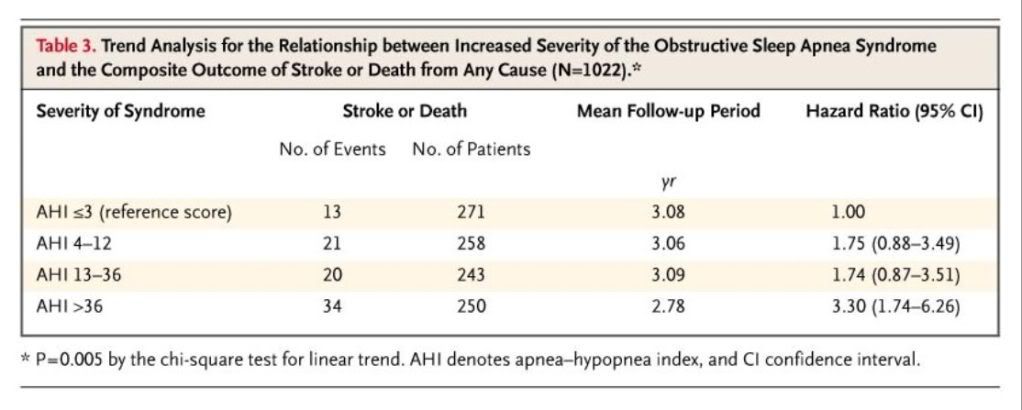
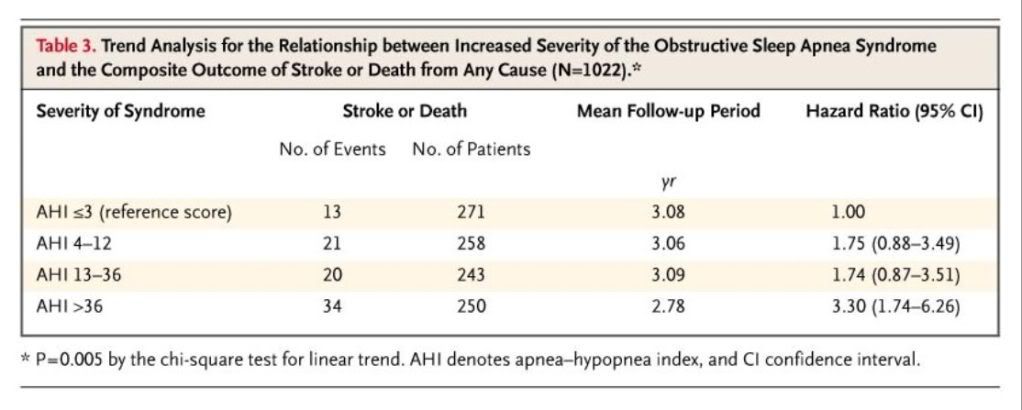
NotMuffy wrote:In another huge study, Yaggi et al (2005) looked at AHI and the risk of catastrophic events, and it became quite clear that severe OSAS (AHI > 36) was associated with much greater risk:
The scary part, however, was that these patients
were being treated:
Many patients with the obstructive sleep apnea syndrome received some type of treatment for sleep apnea after the initial evaluation. Thirty-one percent achieved a weight reduction of 10 percent or more; 58 percent were using airway pressurization for at least four hours per night for five nights or more per week; 15 percent underwent upper-airway surgery.
Are the AHI in Figure 3 the UNTREATED AHI (from the diagnostic sleep studies) for the now treated patients? Or are these the TREATED AHI's? That's not clear and it makes a huge difference in how to appropriately interpret this very interesting data.
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 2:00 pm
by RDawkinsPhDMPH
larry63 ... that's OK, I shouldn't have been so dismissive. I was just being lazy.
robysue ... that was at baseline, untreated.
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 3:57 pm
by robysue
RDawkinsPhDMPH wrote:
robysue ... that was at baseline, untreated.
Thanks!
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 6:24 pm
by NotMuffy
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 6:32 pm
by LoQ
This is an interesting thread. We have several people here that think it doesn't matter how high the AHI goes, as measured by an S7 or S8 machine, as long as the AI is very low. I wonder if this is changing any minds on that view?
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 6:54 pm
by Captain_Midnight
Excellent thread topic and discussion!
R Dawkins, you cite Sulit, et al., Sleep, 2006 as writing... "Vascular responses may be more directly related to sympathetic surges and arousals, whereas metabolic sequelae may be mediated more by hypoxic stress." and that seems to make sense (although I suspect that metabolic sequelae could easily be a secondary consequence to sympathetic surges as well.)
Some random thoughts (as So Well might say.) When I reviewed my sleep study, I was interested in the A v. H pattern. I started of with an enormous obstructive apnea (lasted forever), then for the next few hours, one hypopnea after another. My guess, and it's just a guess (from an "n" of only one) was that the deep apnea triggered the hypopneas as a protective response to avoid more frank apneas; the spooling up our nervous system to throttle us up into a tweener state of sleep which is shallow enough that a blast of epinepherine every minute or so will keep us from suffocation. My thought here is that the consequences of repetitive hypopneas on blood vessels, hormone axes, and a dozen other processes and functions all conspire to mess up our health in the cause of chronic prevention of deeper apnea (suffocation). Hypopneas are (as we scientists love to say) non-trivial.
A possibly similar example is that we apneics tend to increase our RBC count in response to chronic, intermittent hypoxia. This can be serious if it gets up toward polycythemia. Again, a protective response to apnea becomes a risk factor.
.
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 7:51 pm
by robysue
LoQ wrote:This is an interesting thread. We have several people here that think it doesn't matter how high the AHI goes, as measured by an S7 or S8 machine, as long as the AI is very low. I wonder if this is changing any minds on that view?
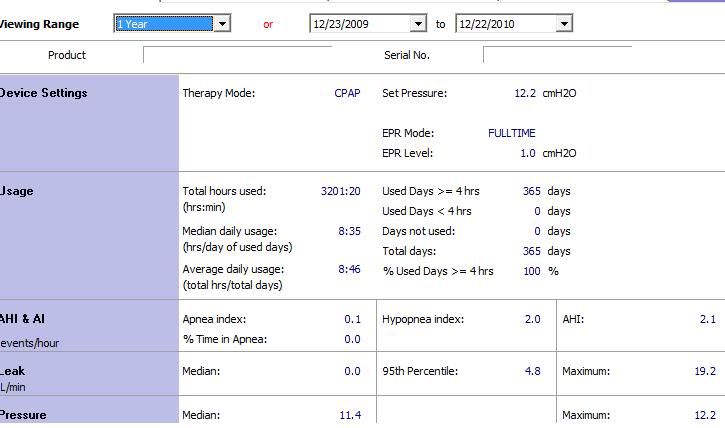
My concern all along has been that the S9 was seriously under reporting my hypopneas. And since its reported number for my apneas has consistently been only a little bit lower than my rather low number of apneas in my untreated diagnostic sleep study, the freak-out part of my brain has begun to become increasingly concerned about whether my true number of hypopneas with the S9 might also actually be much closer to the number of hypopneas in my baseline study. Because in 13 weeks of using the S9, I have not started feeling better; indeed I have continued to feel worse than before I started using the S9.
This is NOT meant to be a slam against the S9. Rather it is an indication of the current state of my sleep deprived, anxiety prone mind some 13 weeks into my specific therapy that has not been going particularly well with the S9 AutoSet. My medical team has been working with me to resolve my problems with CPAP/APAP, and I believe that my problems with the S9's therapy are more about how my body is put together (and not the S9) and how my body has been reacting to the S9's way of delivering therapy and are not actually any kind of an indication of a potential problem with the S9's quality. In any human-designed algorithm, there are design constraints and decisions: Those constraints and decisions will cause some instances of failure in outliers, and I am most likely an outlier. There is most likely something in my particular anatomical make-up and my tendancy to arousal and my apnea/hypopnea mixture that has caused my titrated settings on the S9 AutoSet to create more disruptions to my sleep patterns than expected. The sleep doctor recommended a bi-level titration a while back and I was able to switch to a PR BiPAP this week. It is very early in my BiPAP therapy, but already there are signs that the differences between bi-level therapy and S9's CPAP/APAP therapy modes are significant in my case. And if the positive trends continue to build as time goes by, it will not be because the PR BiPAP is somehow a "better" machine than the S9; rather it will be because the PR BiPAP will prove to be a more appropriate machine for my particular body to use than the rather remarkable S9 AutoSet turned out to be.
Re: What if you have mostly hypnopeas and not apneas?
Posted: Thu Dec 23, 2010 8:26 pm
by carbonman
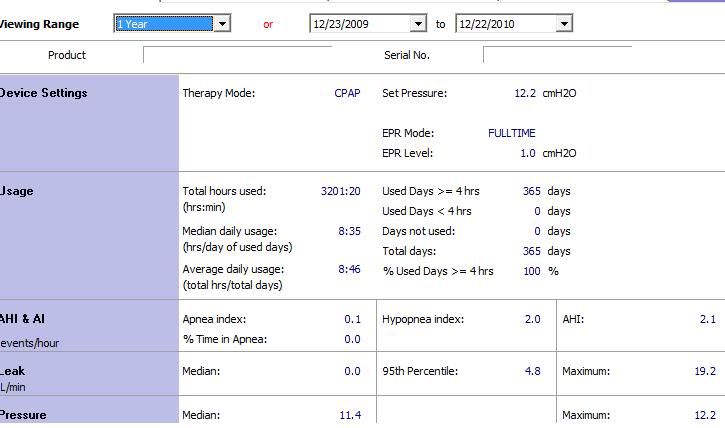
Given an AHI of 71 at the sleep study, w/hypopneas being the majority of events,
I will take these numbers any day.
I have my life back.
I fear no blue dots.
I have no reason to doubt my S8s.
Re: What if you have mostly hypnopeas and not apneas?
Posted: Fri Dec 24, 2010 12:31 am
by Muse-Inc
Thanks! Read an abstract in the past several months (sorry can't remember the title or link, can't even find my copy *sigh*) which did a comparison of diabetics, diabetics with apnea, and apneics. They did a scraping of the arterial wall in the forearm (sounds really
ouchy to me) to evaluate the endothelial tissue health. They projected the worst damage would be with the diabetics; turns out the worst damage was associated with apnea; little damage in the diabetics
without apnea.
Shame we don't have a study with severe apneics effectively-treated (100% compliance, low AHIs) at say 6 months, then 1 and 2 years. We know from that one study that the brain lesions common in men diagnosed with severe apnea disappear (well, 99%) following 12 months of CPAP therapy (lost that link & article too *sigh*...too much stress, sorry!)...I assume the same is true of women in the severe category as I don't think the estrogens play much of a protective role at least not in the amts we produce when we develop apnea, tho our higher amts of progesterone if we use bioidentical progesterone provide some protection.
Re: What if you have mostly hypnopeas and not apneas?
Posted: Fri Dec 24, 2010 3:46 am
by NotMuffy
LoQ wrote:This is an interesting thread. We have several people here that think it doesn't matter how high the AHI goes, as measured by an S7 or S8 machine, as long as the AI is very low. I wonder if this is changing any minds on that view?
Well, "IMHO", I think you have to specifically define hypopnea; identify the type that one has on diagnostic NPSG; and then decide if a ResMed algorithm is the way one chooses to go in the treatment of their SDB.
8 years ago, Michael Berthon-Jones (inventor of the A10), when asked
Why doesn’t ResMed's AutoSet respond to hypopnoea?
Said:
Michael Berthon-Jones wrote:When you are lying quietly awake, or when you first go to sleep, or when you are dreaming, you can have hypopneas (reductions in the depth of breathing) which are nothing to do with the state of the airway. For example if you sigh, which you do every few minutes, you usually have a hypopnea immediately afterwards. This can also happen if you have just rolled over and are getting settled, or if you are dreaming. And the annoying thing is that when you are on CPAP, this tendency to have what are called central hypopneas - hypopneas that are nothing to do with the state of the airway - is increased. If you make an automatic CPAP device that responds to hypopneas, you will put the pressure up to the maximum while the patient is awake.
And then:
Do you think there is a misconception clinically that all hypopneas should be treated?
Said:
Michael Berthon-Jones wrote:For simple obstructive sleep apnea, central hypopneas should not be treated. They are not a disease. Everyone has them. And they don’t go away with CPAP.
So before somebody thinks "Gee, the ResMed algorithms are no good because they don't treat hypopneas", that's by design. The attack is based on apneas (to a point, and that's true if you're whether using A10 or FOT), snoring and flow limitation.
Re: What if you have mostly hypnopeas and not apneas?
Posted: Fri Dec 24, 2010 12:31 pm
by LoQ
NotMuffy, please understand, I vehemently disagree with the assertion that we should not care "how high the AHI goes as long as the bulk of it is from hypopneas," no matter what machine you use. Do you agree with the assertion that HI (on S7/S8) does not matter, or do you agree with me, that it might in fact matter?
NotMuffy wrote:
Michael Berthon-Jones wrote:
When you are lying quietly awake, or when you first go to sleep, or when you are dreaming, you can have hypopneas (reductions in the depth of breathing) which are nothing to do with the state of the airway. For example if you sigh, which you do every few minutes, you usually have a hypopnea immediately afterwards. This can also happen if you have just rolled over and are getting settled, or if you are dreaming.
Yeah. Well, in my case, those hypopneas that don't matter on my S7 machine happen when I am in REM (dreaming?), and are also accompanied by marked decreases in oxygen saturation level. Funny, that.
From my own experience, I can tell you for a fact that a high AHI
DOES matter, even when the AI=0.0, as is often the case for me, and even on an S7 machine. Oxygen desatuations matter, even if they are occurring when AHI is high and AI is zero.
Michael Berthon-Jones wrote:
And the annoying thing is that when you are on CPAP, this tendency to have what are called central hypopneas - hypopneas that are nothing to do with the state of the airway - is increased. If you make an automatic CPAP device that responds to hypopneas, you will put the pressure up to the maximum while the patient is awake.
Not every patient is the same. Not treating hypopneas while awake leads to not treating them during REM when they might actually matter. Poor algorithm. At the very least they might try putting a configurable delay before treating hypopneas to avoid treating the awake ones.
NotMuffy wrote:So before somebody thinks "Gee, the ResMed algorithms are no good because they don't treat hypopneas", that's by design. The attack is based on apneas (to a point, and that's true if you're whether using A10 or FOT), snoring and flow limitation.
Well I don't have apneas, except for the occasional harmless central. Perhaps the ResMed algorithm is not suitable for patient who have hypopnea syndrome. Is there a better algorithm out there for us, one which will actually treat hypopneas? I don't snore, but I do have flow limitations. However, the ResMed fuzzy flow logic is not really identifying my FL's. It's easy to see that they are being totally missed on any of my charts from the S9.
Re: What if you have mostly hypnopeas and not apneas?
Posted: Fri Dec 24, 2010 1:00 pm
by LoQ
gvz wrote:LoQ,
Why can't you understand? Hypopneas are just baby apneas which haven't grown up yet. They look so cute in ResScan. In fact, it is desirable to have little blue babies visit you in your sleep.
That is one of the stupidest things ever said here. Very smurfy. La la, la la la la, la la la la la la.....