Page 30 of 75
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 3:48 pm
by blizzardboy
dsm wrote:Something like this may alleviate your worries ...capnometry...noninvasive method...won't be cheap
I am going to talk to a sleep physician about this today. Cheers,
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 4:51 pm
by dsm
BB
Just came across some data I had saved from past discussions & wanted to make a point about getting leaks completely under control when using Bilevels and ASV machines (IMHO your leak level is higher than it need be). This info may be of general interest rather than specific to your case, but worth posting.
The following comments & data come from 2 manuals - Puritan Bennett Knightstar PB330 & the Resmed Vpap III.
DSM
From the PB330 manual ...

****************************************************************************************************
From the Vpap III manual ...

>>
The amount of rebreathing is dependent upon
respiratory rate, tidal volume, I:E ratio, leak characteristics of the patient interface, deadspace, and EPAP pressure.
To a lesser extent, IPAP pressure will also affect rebreathing. Lower pressures, higher tidal volumes, and higher percentage IPAP will increase the amount of retained CO2 and thus increase rebreathing.
The graph on page 54 (not included here) provides the exhalation port pressure and flow characteristics of ResMed masks available for use with the VPAP flow generator. The CO2 rebreathing table on page 44 (see above) provides information on CO2 rebreathing at several pressures. This information may assist in assessing the CO2 rebreathing potential at particular device settings. The characteristics of other masks may be different, and it is important to select a mask that provides comfort while delivering correct treatment.
Note: The data provided is derived from bench testing and is for guidance only. The amount of CO2 rebreathing in actual clinical use may vary. It is recommended that patient monitoring be performed to assess the adequacy of patient CO2 level management, particularly at low EPAP pressures.
<<
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 7:39 pm
by blizzardboy
blizzardboy wrote:dsm wrote:Something like this may alleviate your worries ...capnometry...noninvasive method...won't be cheap
I am going to talk to a sleep physician about this today. Cheers,
I enjoyed my chat with the new sleep physician today. Here is a summary of our discussion:
- Had not received my blood results yet
- Was happy to engage with me at a deeper level of discussion
- Not condescending but listened and informed
- Said that I was a complex case, was treating one other like me
- Looked at my PSGs, said I wasn't a difficult diagnosis: non-periodic, unstable breathing with apneic event/arousal issues mainly during lighter (stage 1/2) sleep
- No apnea problems when I make it too deeper (SW) sleep
- Felt my RDI could effect be over-scored due effective double counting of respiratory events coupled to arousals
- Not concerned about my health
- Would consider me treated once my AHI<10
- Happy with the current treatment of my AHI
- Don't even try to chase AHI=0, waste of time
- Talked about Loop Gain circuit underlying sleep stability
- Said he was going to Thoracic meeting in US tomorrow to find out latest research on trying to keep people like me in deeper levels of sleep to avoid arousals
- Showed me a table of latest research showing that on average depression is the number one contributor to arousals (about 10/hour) with BMI at number two (about 5/hr) and OSA at number 7 (about 2/hr)
- Said that my ABG was probably closer to apneic thresholds that the average thus contributing to sleep instability
- Said it was good that I was receiving CBT
- Agreed that a change to fixed CPAP for a while might be a good trial
- Stated that ASV was excellent for treating periodic breathing issues but gave sporadic results for unstable breathers like me
- Was not necessarily concerned about my leg movements, could be normal and may not be periodic
- Wants to review my PSG results before we go any further
- Was open that we don't really know how to treat people like me at present, and was happy that I was endeavoring to find answers
- Didn't think it necessary to combine CPAP with a MAS for now
- Thought it a good idea for me to reduce my weight, of course
- Thought that EEP=8 should be plenty to treat my OSA given my size and weight
- We speculated that increasing EEP above 8 could possible contribute to bringing my PCO2 closer to the apneic threshold
- Was not concerned that my AHI on the Bipap ASV with Epap=8 was around 6-7, thought I was being well treated
- We discussed EtCO2 measurements and said that he would first review my PSG EtCO2 measurement and then go from there
- Concluded that my sleep instability could possibly be related to mental health issues
- Will see me again in 6 weeks to discuss the possibility of further diagnostics/treatment options if any
A lot of the things that this doctor said to me were strikingly similar to some of the advice I have received in this forum...
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 8:21 pm
by Rebecca R
blizzardboy wrote:
I enjoyed my chat with the new sleep physician today. Here is a summary of our discussion:
…
- Said he was going to Thoracic meeting in US tomorrow to find out latest research on trying to keep people like me in deeper levels of sleep to avoid arousals
……
Blasted arousals...Well if he returns with a magic cure, please share. I'm getting tired of them too.
r
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 8:42 pm
by SleepingUgly
blizzardboy wrote:[*]Showed me a table of latest research showing that on average depression is the number one contributor to AHI (about 10/hour)
I'd like to see that research - did you happen to catch an author or anything?
with BMI at number two (about 5/hr) and OSA at number 7 (about 2/hr
I'm confused... How can depression cause apneas + hypopneas, that is, AHI? And OSA IS apneas and hypopneas, so I'd expect a perfect correlation between AHI and OSA?! What am I missing?
Thought it a good idea for me to reduce my weight, of course
What did he say about wearing a Speedo over tights?
Concluded that my sleep instability could possibly be related to mental health issues
(-SWS, I can hear you panting...) Did he explain via what mechanism?
What did he say about the Prozac? BTW, I just read something about SSRIs increasing upper airway patency in NREM sleep... (No idea if that's relevant to you, so take it with a grain of salt)
Did he mention using any medications to enhance slow wave sleep, such as Gabitril?
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 9:45 pm
by blizzardboy
SleepingUgly wrote:with BMI at number two (about 5/hr) and OSA at number 7 (about 2/hr
I'm confused... How can depression cause apneas + hypopneas, that is, AHI? And OSA IS apneas and hypopneas, so I'd expect a perfect correlation between AHI and OSA?! What am I missing?
My bad, was an arousals index. I have edited my original post.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 10:01 pm
by blizzardboy
SleepingUgly wrote:blizzardboy wrote:[*]Showed me a table of latest research showing that on average depression is the number one contributor to arousals (ed.) (about 10/hour)
I'd like to see that research - did you happen to catch an author or anything?
I've rung his clinic to track down the research details. I'll post them if I receive a reply.
What did he say about wearing a Speedo over tights?
He said it definitely wasn't contributing to arousal(s).
blizzardboy wrote:Concluded that my sleep instability could possibly be related to mental health issues
(-SWS, I can hear you panting...) Did he explain via what mechanism?
No, but I am sure we will talk more about this in the fullness of time, especially if he can't find any other explanation for my sleep disturbance. (You haven't got -SWS locked up under the floor have you?)
What did he say about the Prozac?
Didn't buy into any talk of note when I queried on fluoxetine (Prozac) possibly aggravating PLMs. He wanted to review my PSG to see the nature of the leg movements for himself.
Did he mention using any medications to enhance slow wave sleep, such as Gabitril?
No specific drugs but we did touch on the use of benzos to keep sleepers at depth. He then said that he was going to a big Thoracics conference in the US tomorrow where they would discuss this topic in detail and he would bring back a summary of the leading edge treatments in this regard.
http://conference.thoracic.org/
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 10:06 pm
by blizzardboy
Hey Muffy, Going down to pick up tar balls this weekend?
As promised:
http://users.adam.com.au/sixsome/SD_051110.pdf. Cheers,
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 10:10 pm
by blizzardboy
Rebecca R wrote:Blasted arousals...Well if he returns with a magic cure, please share. I'm getting tired of them too.
Hi r, You sure do look tired and aroused in your avatar.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Tue May 11, 2010 10:26 pm
by blizzardboy
SleepingUgly wrote:I'd like to see that research - did you happen to catch an author or anything?
Hi SU, The clinic just called me: Personal communication of yet-to-be-published research by a leading Australian medical scientist. That's the best I can do for now. Cheers,
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Wed May 12, 2010 2:41 am
by Muffy
blizzardboy wrote:Hey Muffy, Going down to pick up tar balls this weekend?
If they're coming up this far we're in BIG trouble.
Did you ask specifically if the fluoxetine was contributing to the sleep instability?
On the other hand, perhaps potentially opening the SSRI Discontinuation Syndrome can of worms was something he really wasn't interested in.
Reducing/stopping caffeine might help that middle of the night Wake. Switch to decaffeinated or mix up a batch of half-and-half to taper down.
I think we're coming up to your Epilogue post soon, too.
Muffy
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Wed May 12, 2010 4:09 am
by Muffy
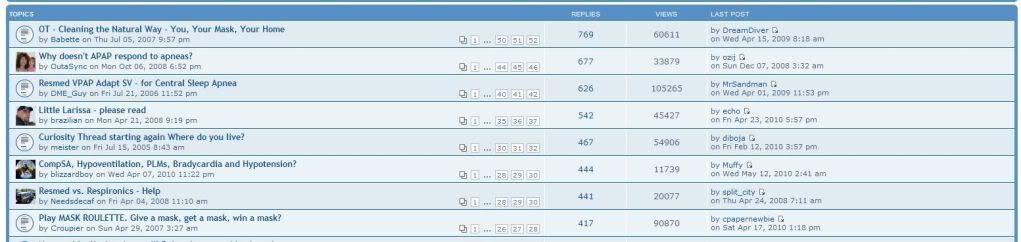
BTW, did you realize that in terms of replies, this is (presently) the #6 thread of all time?
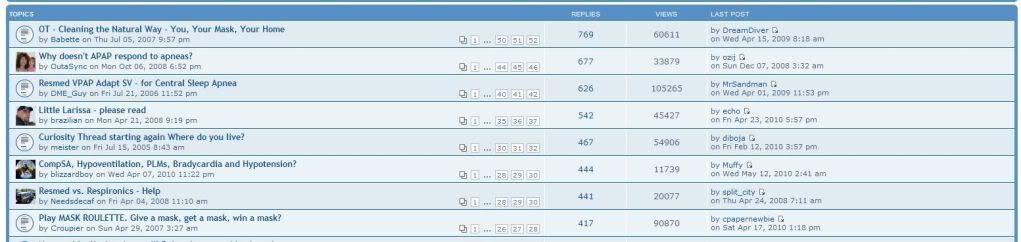
Truly one that will live on in the anals of cpaptalk!
Muffy
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Wed May 12, 2010 5:55 am
by SleepingUgly
blizzardboy wrote:Did he mention using any medications to enhance slow wave sleep, such as Gabitril?
No specific drugs but we did touch on the use of benzos to keep sleepers at depth.
I hope he comes up with something besides benzos... Gabitril enhances slow wave sleep. Gabapentin (Neurontin) might too, not sure.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Wed May 12, 2010 5:58 am
by SleepingUgly
Muffy wrote:Did you ask specifically if the fluoxetine was contributing to the sleep instability?
On the other hand, perhaps potentially opening the SSRI Discontinuation Syndrome can of worms was something he really wasn't interested in.
BB, is he going to review the raw data on your sleep study to see if they are true PLMS as opposed to muscle contractions in respiratory efforts?
Muffy wrote:BTW, did you realize that in terms of replies, this is (presently) the #6 thread of all time?
Yes, you're so lucky to have so much of the experts' attention, when some of us can't get so much as a reply to a PM...
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Wed May 12, 2010 3:15 pm
by blizzardboy
Muffy wrote:Reducing/stopping caffeine might help that middle of the night Wake. Switch to decaffeinated or mix up a batch of half-and-half to taper down.
Hi Muffy,
Those coffees are already half measures (1/2 teaspoon instant coffee) in an attempt to wean myself off caffeine gently.
On waking this morning (interesting how I wake with newly processed thoughts, certainly must be more going on in the sleeping brain than dreams) I realised why you made the alarm clock/snooze comment. You were implying that my awakenings were regular, as thought initiated by an alarm, right? Please excuse me for being a bit slow off the mark.
I remembered another comment that the sleep doctor made yesterday: That it is normal for a man of my age (c.40 y.o.) to have a couple of awakenings during sleep, and that this will only increase as I age (5ish when 50, 8ish when 60, etc).
As suggested by -SWS, I slept last night with fixed CPAP @ P=9.6, that is my ASV EEP pressure (that I have used for the longest.) I would think the most stable breathing that I have exhibited to date, even if my ventilation is still probably lower than the norm:
http://users.adam.com.au/sixsome/ASV/0510/051210/.