Page 68 of 75
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Thu Jun 24, 2010 4:25 am
by Muffy
SleepingUgly wrote:Did they ever look at your sleep studies to see if your PLMS were respiratory-related or not?
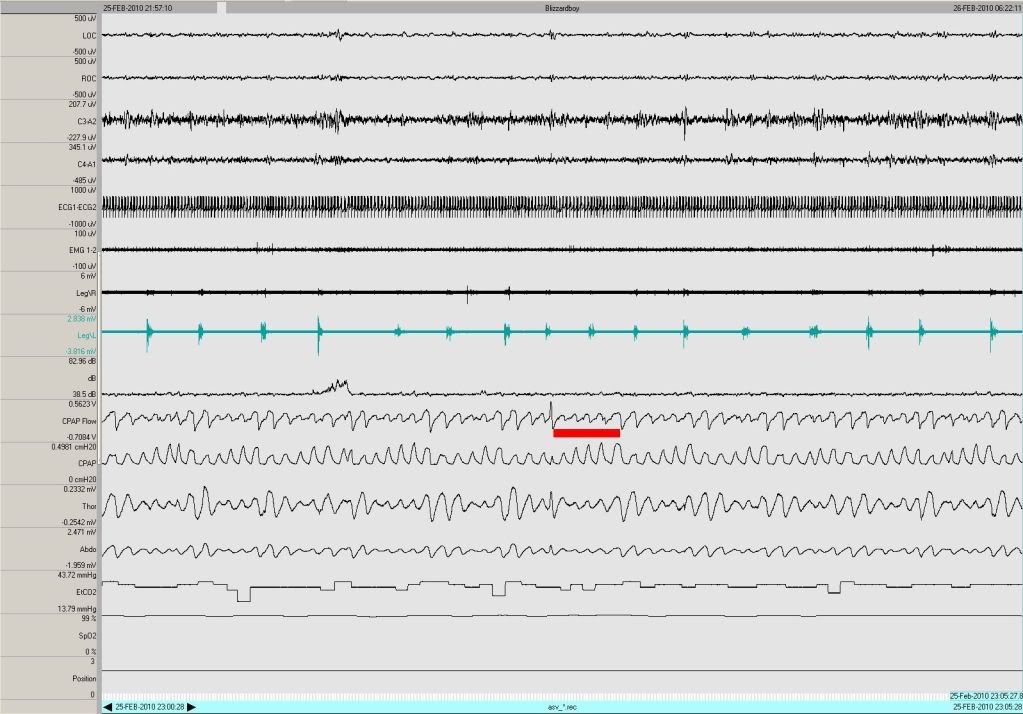
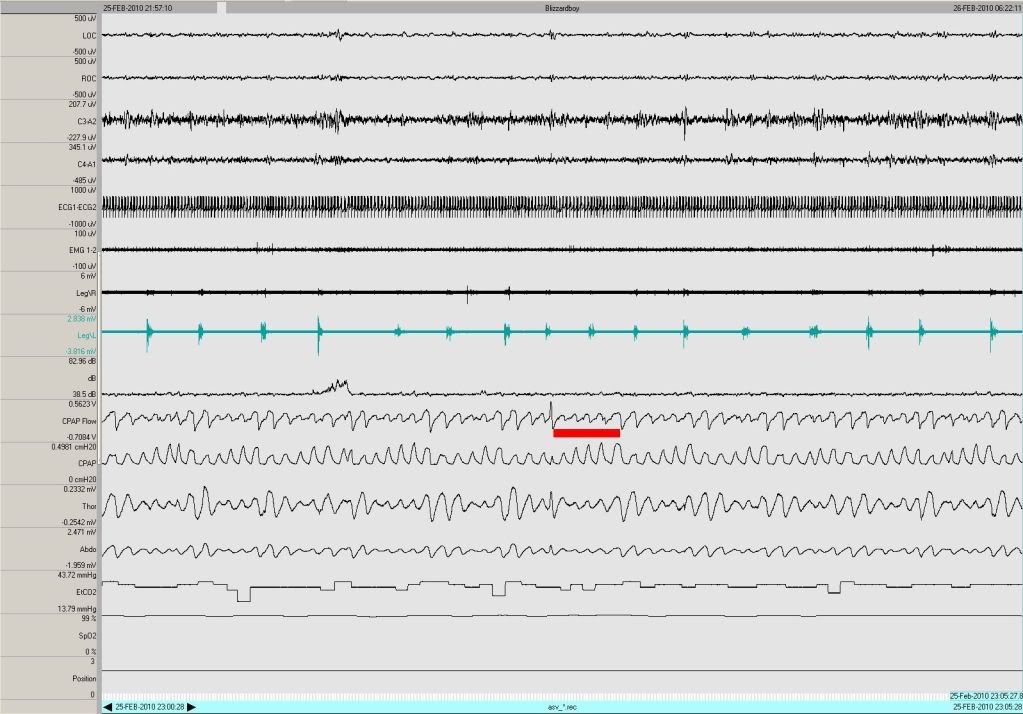
Interestingly, in the ASV Titration, it is the reverse that occurs. Some PLM Runs that result in arousals have compensatory central phenomenon, which in turn causes the ASV to launch an (unnecessary) attack (note the increase in pressure in the CPAP channel):
However, I believe most to all of the PLMs were scored correctly (the actual scoring mask was not submitted).
Muffy
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Thu Jun 24, 2010 4:32 am
by blizzardboy
SleepingUgly wrote:You are tapering off fluoxetine, not going cold turkey, right??
Hi SU, Yes, I tapered off before stopping completely. No negative withdrawal symptoms have been noted to date.
SleepingUgly wrote:How will you know if your PLMS have remitted once you are fully off fluoxetine and it's all washed out? Are you going to do another sleep study?
Won't know really until I sleep through another PSG. It will be interesting to see what my sleep doc makes of my PSG data, and what action he, in conjunction with my GP, recommends.
SleepingUgly wrote:I would NOT be in a hurry to introduce any medications for treatment of PLMS until you're sure that you still have them well after Fluoxetine is washed out, and that they are the cause of your arousals...Medications can cause a whole host of other problems, and who needs that?!
Hear, hear. Cheers,
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Thu Jun 24, 2010 4:38 am
by blizzardboy
Muse-Inc wrote:Aww, BB, you've got my profound sympathy and best wishes for discovery of an effective treatment. Where's 'House' when ya need a great diagnostician?
Hi M-I, Thank you for your good wishes. Well let's hope my sleep doc and/or GP are a dwelling of some sort.
Re: You Can Make Anything Look Like Anything Else
Posted: Thu Jun 24, 2010 4:41 am
by blizzardboy
Muffy wrote:It's a center!!
Doh, and I thought I had it right! Surely that was my first slip up? By Toutatis I swear that I will never do it again. (BB walks to the blackboard)
It is a centre not a clinic.
It is a centre not a clinic.
It is a centre not a clinic.
It is a centre not a clinic.
.
.
.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Thu Jun 24, 2010 4:43 am
by blizzardboy
Muffy wrote:which in turn causes the ASV to launch an (unnecessary) attack (note the increase in pressure in the CPAP channel)
Hi Muffy, Thank you for the latest image. Do you think there is anything clinically significant that can be gleaned from my lack of response to the ramping increase in CPAP pressure delivered by the ASV?
Also, would you please be able to post an example of CPAP flow with a desirable (stable; smooth; un-FL) waveform? Cheers,
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Thu Jun 24, 2010 4:31 pm
by blizzardboy
Hi all,
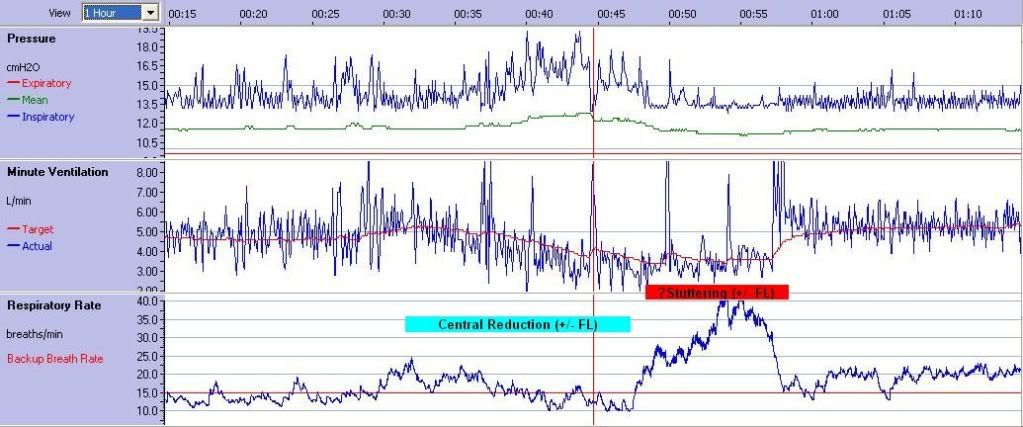
Here is another clear example of the Adapt SV reporting a high resp rate (up to 40 bpm) during times of FL in my breathing (0030-0100):

I don't like seeing my Minute Volume
Target drop down to around 3.5 L/min, yet alone my actual Minute Volume.
and the Adapt SV was trying in vain to overcome my FL with a pressure-increase barrage but then succumbed to the inevitable memory loss of the moving average (zoom of previous image):

PFT today. Cheers,
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Fri Jun 25, 2010 3:44 am
by Muffy
blizzardboy wrote:Muffy wrote:which in turn causes the ASV to launch an (unnecessary) attack (note the increase in pressure in the CPAP channel)
Hi Muffy, Thank you for the latest image. Do you think there is anything clinically significant that can be gleaned from my lack of response to the ramping increase in CPAP pressure delivered by the ASV?
No. There's nothing to respond to.
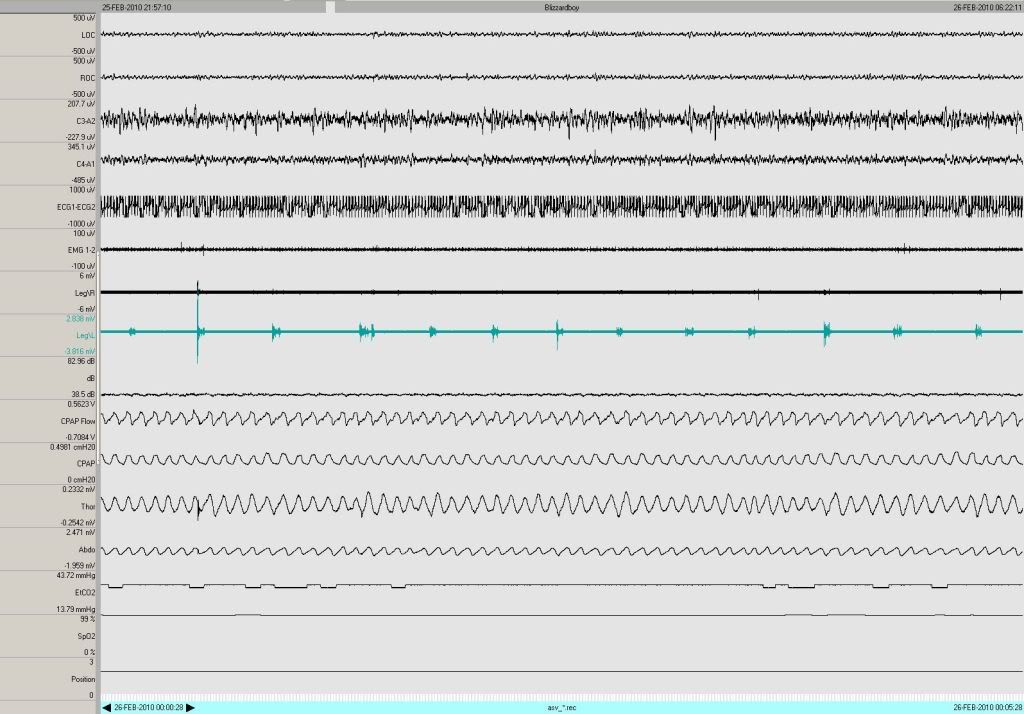
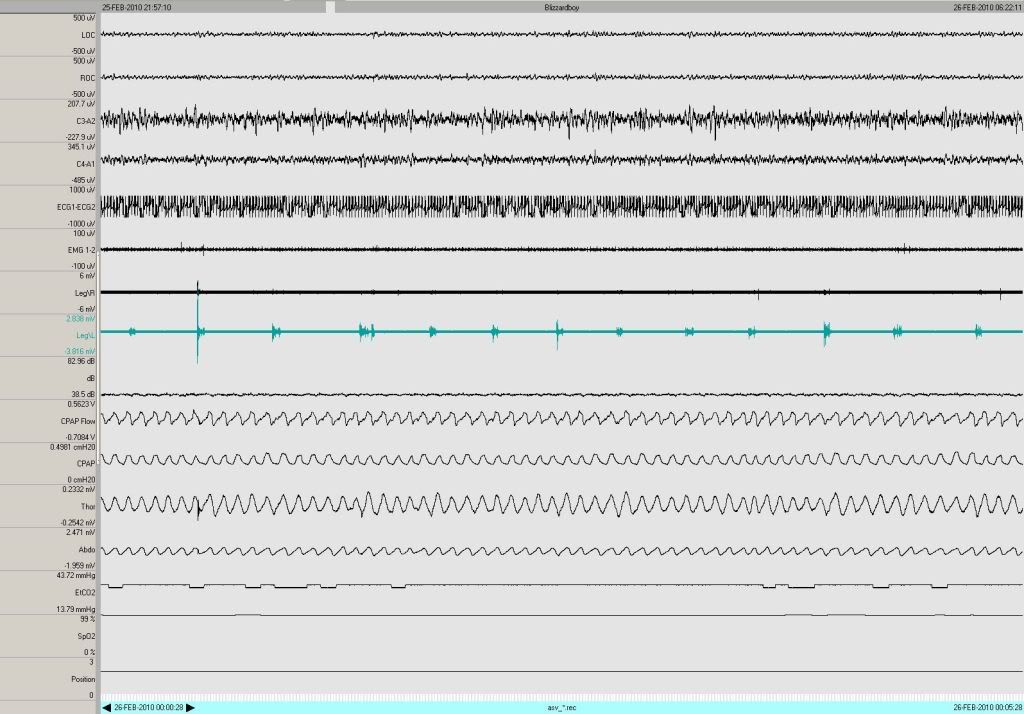
blizzardboy wrote:Also, would you please be able to post an example of CPAP flow with a desirable (stable; smooth; un-FL) waveform?
Sure. Complete with PLMs:
Muffy
Re: You Can Make Anything Look Like Anything Else
Posted: Fri Jun 25, 2010 3:47 am
by Muffy
blizzardboy wrote:Muffy wrote:It's a center!!
Doh, and I thought I had it right! Surely that was my first slip up? By Toutatis I swear that I will never do it again. (BB walks to the blackboard)
It is a centre not a clinic.
It is a centre not a clinic.
It is a centre not a clinic.
It is a centre not a clinic.
.
.
.
Toutatis doesn't seem to be all that effective right about now (saw your first trip up to the blackboard).
Maybe try Apophis.
Muffy
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Fri Jun 25, 2010 3:56 am
by Muffy
blizzardboy wrote:...the Adapt SV was trying in vain to overcome my FL...
How ya figure that to be FL?
Muffy
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Fri Jun 25, 2010 4:15 am
by blizzardboy
Muffy wrote:No. There's nothing to respond to.
Hi Muffy, OK. I can see that from a respiratory need point of view my body has no inclination to inhale during the pressure onslaught as in am in a post big-breath state (natural central). Its just that I visualise that the application of ASV IPAP would cause some degree of increase in flow c.f. treatment of central apneas by ASV. I thought that the fact that I show no response to IPAP maybe indicates that something is amiss in my airway - like something is preventing the increase in pressure from inducing increased airflow.
Muffy wrote:Sure. Complete with PLMs:
Thanks for that. Good to see that I am capable of normal breathing patterns during sleep.
Nothing obvious appeared in my PFT today. The results will be sent to my GP next week after being analysed by the respiratory specialist. Was interesting for me to learn that CO is inhaled to test diffusion efficiency in the alveoli. Cheers,
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Fri Jun 25, 2010 4:20 am
by blizzardboy
Muffy wrote:blizzardboy wrote:...the Adapt SV was trying in vain to overcome my FL...
How ya figure that to be FL?
I assumed that, because of your previous demonstration of stuttering during FL, that this was the case here. Do you think that maybe I have more tricks up my sleeve to get ASV stutters happening?
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Fri Jun 25, 2010 4:44 am
by Muffy
blizzardboy wrote:Muffy wrote:blizzardboy wrote:...the Adapt SV was trying in vain to overcome my FL...
How ya figure that to be FL?
I assumed that, because of your previous demonstration of stuttering during FL...
Where did Muffy correlate "stuttering" with FL?
Muffy
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Fri Jun 25, 2010 4:59 am
by blizzardboy
Muffy wrote:Where did Muffy correlate "stuttering" with FL?
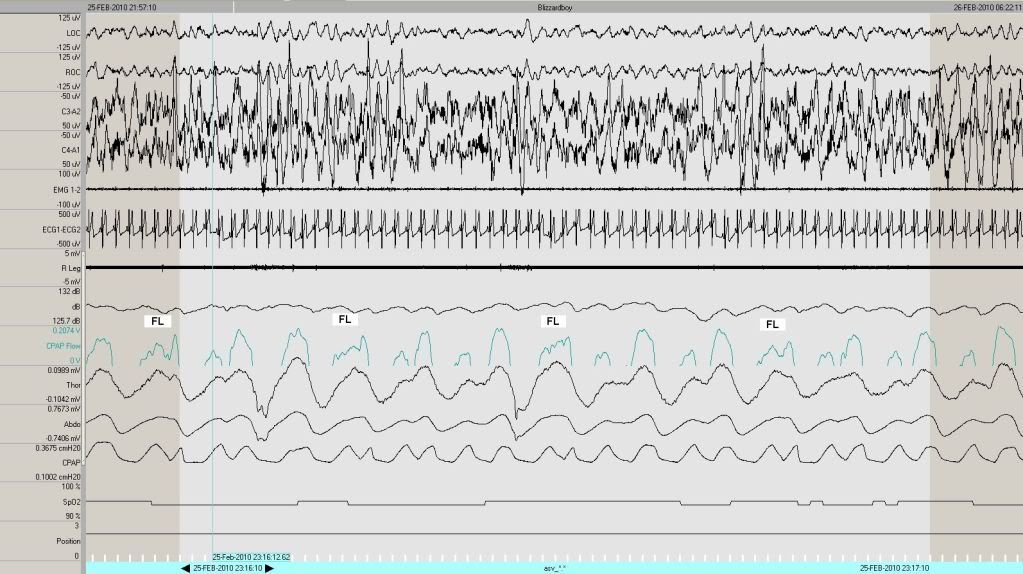
No, I didn't mean to infer that you demonstrated a correlation its just that FL was present when you showed an example of stuttering here:
Muffy wrote:blizzardboy wrote:Muffy wrote:Just about every breath gets a double hit.
I am trying to understand what the algorithm is attempting to acheive during these periods of "double hitting". I suppose, given the flow-metering nature of CPAP, that mid-inhalation the machine senses a partial exhalation followed by the completion of the inhalation cycle i.e. stutter, thus demonstrating the rapid nature of the ASV response to respiratory variations and its charter to maintain tidal volume.
At the risk of microanalyzing your microanalysis, and keeping in mind that this is offered as a possible explanation for something you did
once (recurring theme of solitary events that don't need to be bludgeoned to death), if the CPAP Flow is clipped at 0.0 volts to allow only the + portion, then this should expose only the inspiratory limb of the breath:
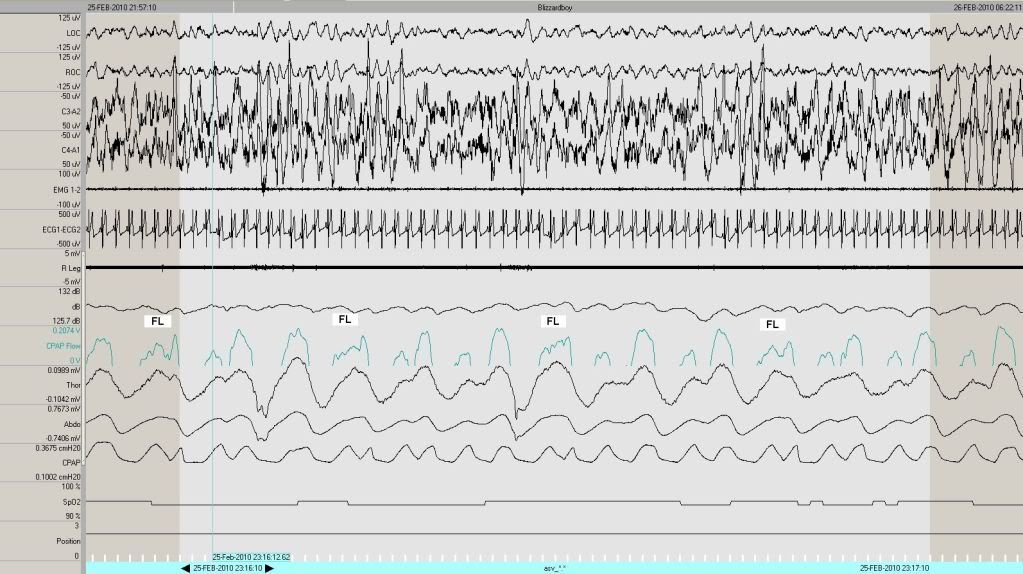
Keep in mind that I don't believe this to be a ResControl signal because of the reasons previously mentioned (and because of the behavior of the Snore Channel, I believe they employed a PTAF2 system), and if so, doesn't represent in the strictest sense what the AdaptSV actually "sees".
So anyway, what I think is happening is that you're having Flow Limitations that slow to the point where the AdaptSV thinks your flow has (briefly) ceased, switched to EEP, then back to IPAP
whatever nearly instantaneously. This completes a single inspiratory effort, but registers as a "stutter" vis-à-vis Respiratory Rate.
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Fri Jun 25, 2010 6:14 am
by Muffy
blizzardboy wrote:Muffy wrote:Where did Muffy correlate "stuttering" with FL?
No, I didn't mean to infer that you demonstrated a correlation its just that FL was present when you showed an example of stuttering here:
OK, that explanation offered was
FL in PSG > stuttering > high respiratory rate
for

where VE remained stable.
It may not be that the reverse will hold true to create a Rule such that
High respiratory rate > stuttering > is always FL in everybody so let's treat it
Anyway, in

there's additional stuff happening, and I don't think
blizzardboy wrote:the Adapt SV was trying in vain to overcome my FL with a pressure-increase barrage
Is what's happening.
In the latest example, VE initially reponds accordingly, there is no apparent stuttering, and the overall appearance is that of some central reduction in VE via a gradual drop in respiratory rate rather than obstructive phenomenon (such as FL):
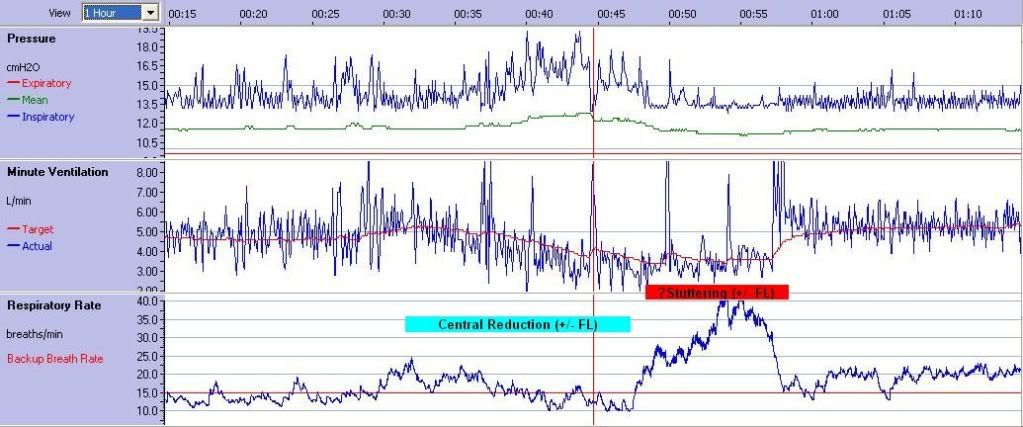
The high RR burst, with no change in VE, however, is probably "stuttering" again.
Muffy
Re: CompSA, Hypoventilation, PLMs, Bradycardia and Hypotension?
Posted: Fri Jun 25, 2010 6:36 am
by blizzardboy
Muffy wrote:It may not be that the reverse will hold true to create a Rule such that
High respiratory rate > stuttering > is always FL in everybody so let's treat it
Anyway...there's additional stuff happening, and I don't think
blizzardboy wrote:the Adapt SV was trying in vain to overcome my FL with a pressure-increase barrage
Is what's happening.
In the latest example, VE initially reponds accordingly, there is no apparent stuttering, and the overall appearance is that of some central reduction in VE via a gradual drop in respiratory rate rather than obstructive phenomenon (such as FL)...The high RR burst, with no change in VE, however, is probably "stuttering" again.
Thanks for that - and I really thought I was on to a winner when I penned "FL" in my post this morning! I hadn't noticed the clear slow descent of my RR into the SoS (State of Stuttering). Would you say that I was probably experiencing this SoS during a SWS stage, and then I had an arousal at the end of the SoS which resulted in the steep pick up of my VE?